Abstract
The aim of this postal survey was to determine the prevalence and impact of patient-perceived leg length discrepancy (LLD) at 5–8 years after primary total hip replacement (THR). A postal audit survey was undertaken of all consecutive patients who had a primary unilateral THR at one elective orthopaedic centre between April 1993 and April 1996. The questionnaire included the Oxford hip score (OHS) and questions about LLD. Questionnaires were received from 1,114 patients. In total, 329 THR patients (30%) reported an LLD, although radiographic analysis revealed that only 36% of these patients had anatomical LLD. Patients with a perceived LLD had a significantly poorer OHS (p < 0.001) and reported more limping than those patients without a perceived LLD. This study found that a third of patients perceived an LLD after THR and that perceived LLD was associated with a significantly poorer midterm functional outcome.
Résumé
Le but de cette étude est de déterminer l’impact et la perception des patients secondaires à une inégalité de longueur (LLD) entre 5 et 8 ans de recul après une prothèse totale de hanche. Matériel et méthode: Nous avons réalisé une enquête postale concernant une série consécutive de patients ayant bénéficié d’une prothèse totale de hanche unilatérale réalisée dans notre centre entre avril 1993 et avril 1996. Ce questionnaire incluait par ailleurs le score d’Oxford (OHS) et des questions concernant cette inégalité de longueur. Résultats: ces questionnaires ont été reçus par 1 114 patients. Au total 329 (30%) rapportaient une inégalité de longueur mais, l’analyse radiographique montrait que seulement 36% de ces 30% avaient une véritable inégalité de longueur anatomique. Les patients qui se plaignent d’une inégalité de longueur après prothèse totale de hanche ont un score d’OHS significativement plus bas que les autres (p < 0.001) et une boiterie de durée plus longue si on la compare à ceux qui ne se déclarent pas porteur d’une inégalité de longueur. En conclusion, cette étude montre qu’un tiers des patients se plaignent d’une inégalité de longueur après prothèse totale de hanche et que cette inégalité de longueur est associée à une résultat fonctionnel significativement plus bas que celui des patients sans inégalité de longueur.
Introduction
Total hip replacement (THR) is considered an effective surgical intervention for the relief of chronic pain and functional disability. Survivorship analysis and surgeon-based outcome measures suggest that outcomes after THR are excellent [1]. However, patient-reported outcome measures have uncovered a significant proportion of patients who experience a poor functional outcome after THR [2–4]. Patient factors that correlate with a poor outcome include higher pre-operative pain and functional disability, older age and more medical co-morbidities [5, 6]. A surgical aspect of THR which can lead to reduced functional outcome is leg length discrepancy (LLD) [7].
Leg length equality after THR is important to optimise hip biomechanics and LLD has several potential negative consequences for the patient, including sciatica, chronic back pain, hip dislocation, the need for a shoe raise and a limp [8, 9]. LLD most commonly involves over-lengthening of the limb on the operative side because of a lengthening of the prosthetic head-neck distance [7]. Although the prevalence of anatomical LLD after THR is high [7], the impact of this leg length inequality on patient-reported functional outcome is unclear. Whereas research has found that LLD has no effect on functional outcome [10], a more recent study found that patients with LLD reported a poorer functional outcome that those patients with equal leg lengths [7]. Because of the disparity in the literature, the aim of this postal survey was to determine the prevalence of patient-perceived LLD after primary THR and its impact on midterm functional outcomes.
Materials and methods
During 2001, a postal audit survey was undertaken of all consecutive patients who had a primary unilateral THR at one elective orthopaedic centre between April 1993 and April 1996. Four questions were included in the survey to assess LLD. Firstly, patients were asked whether they thought their legs were the same length. Those patients who indicated that their legs were different lengths were then asked the following questions: (1) Does the difference bother you? (2) Do you use a shoe raise? (3) Do you feel the operation was worthwhile? Patients indicated either yes or no for each question.
To assess functional outcomes after THR, the Oxford hip score (OHS) [11] was included in the questionnaire. The OHS is a patient-reported outcome measure that was developed to assess functional ability and pain from the patient’s perspective. It is a joint-specific questionnaire developed and validated for use in patients undergoing THR. The OHS consists of 12 questions about pain and physical limitations experienced over the past 4 weeks because of the hip. Each question has five response categories, giving a score of between 1 and 5 (low disability to high disability). Scoring involves summating the total for each item to produce a final score between 12 and 60, with a higher score indicating a greater level of functional disability. The frequency of limping was assessed using a question from the OHS, which asks respondents to indicate how often they limp by choosing one of the following response categories: never/rarely, sometimes/just at first, often/not just at first, most of the time or all of the time.
To determine if anatomical LLD was present in those patients who perceived an LLD, radiographs of a random sample of 74 patients who reported LLD were analysed. Leg length was assessed by measuring the vertical distance from the transischial line to the bottom of the lesser trochanter bilaterally. Leg length discrepancy was defined as a leg length difference of ≥ 5 mm. The same radiographic analysis was performed on a sample of 74 patients who did not perceive an LLD to determine the prevalence of unperceived anatomical LLD.
Statistics
Non-parametric tests were used in the statistical analysis because the assumptions of normality were not met when the data were tested with a Kolmogorov-Smirnov test. Mann-Whitney U tests were used to determine if there were significant differences in the OHS or age between unpaired groups. A Kruskal-Wallis test was used to determine if there was significant differences in the OHS with different femoral stem prostheses. Chi-squared tests were used to compare each item on the OHS between patients with and without a perceived LLD.
Results
Between April 1993 and April 1996, 1,704 patients had a primary unilateral THR at one elective orthopaedic centre. Of these patients, 169 had died by the time of follow-up and therefore questionnaires were sent to the remaining 1,535 patients. After the initial mail-out and two reminder mail-outs, completed questionnaires were received from 1,114 THR patients, giving an overall response rate of 73%.
The demographics of patients with and without a perceived LLD are presented in Table 1. There was no significant difference in the age of patients with and without a perceived LLD (p = 0.53). Three hundred and twenty-nine THR patients (30%) reported that they thought their legs were different lengths. Of those patients with a perceived LLD, 161 patients (49%) were bothered by the difference, 101 patients (31%) used a shoe raise and 13 patients (4%) thought that the surgery had not been worthwhile. In comparison, no patients who perceived their legs to be of equal length thought the operation had not been worthwhile. Although patient perception of LLD was high, radiographic analysis of the leg length of 74 patients who reported LLD revealed that only 27 (36%) patients had an anatomical LLD. The radiographic analysis of unperceived anatomical LLD revealed that 11 (17%) patients who reported no perceived LLD had anatomical LLD.
Table 1.
Patient demographics
| No LLD | LLD | |
|---|---|---|
| (n = 785) | (n = 329) | |
| Age (years) | ||
| Median | 69 | 68 |
| Side of surgery (%) | ||
| Left | 57 | 51 |
| Right | 43 | 49 |
| Gender (%) | ||
| Male | 38 | 32 |
| Female | 62 | 68 |
LLD leg length discrepancy
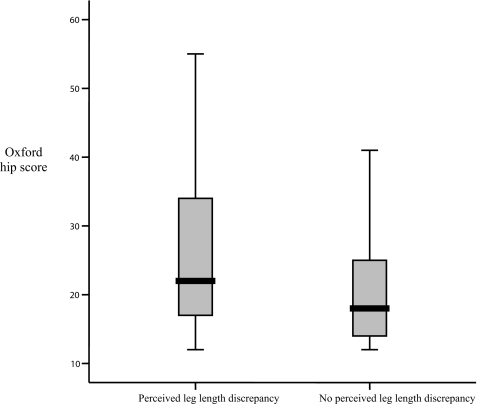
The median OHS for patients with a perceived LLD was 22 (range: 12–55), which was significantly worse that the median OHS of 18 (range: 12–53) for patients who thought their legs were the same length (p < 0.001), indicating that patients with a perceived leg length inequality experienced a poorer functional outcome (Fig. 1). All items on the OHS were significantly different between patients with and without a perceived LLD (p < 0.001). The frequency of limping among patients with and without a perceived LLD is displayed in Table 2. Limping was more prevalent in patients who perceived an LLD, with 31% of patients limping most or all of the time, compared to only 9% of patients without a perceived LLD.
Fig. 1.
Box plot of the median Oxford hip score in patients with and without perceived leg length discrepancy
Table 2.
Frequency of limping over the past 4 weeks
| No perceived | Perceived | |
|---|---|---|
| LLD | LLD | |
| (n = 785) | (n = 329) | |
| Rarely/never | 59% | 32% |
| Sometimes/just at first | 28% | 28% |
| Often/not just at first | 4% | 9% |
| Most of the time | 6% | 14% |
| All of the time | 3% | 17% |
LLD leg length discrepancy
The impact of the femoral stem prosthesis on the OHS and frequency of LLD and limping was analysed. In total, 985 patients (88%) had one of three femoral stems: 740 patients received a CPT (Zimmer), 133 received an Exeter (Stryker) and 112 received a Charnley (DePuy). There was no significant difference in the overall OHS (p = 0.7), frequency of LLD (p = 0.36) or frequency of limping (p = 0.54) between the three prostheses (Table 3).
Table 3.
Median Oxford hip score (OHS), percentage of patients with perceived leg length discrepancy (LLD) and a limp by femoral stem prosthesis
| CPT | Charnley | Exeter | p value | |
|---|---|---|---|---|
| Median OHS (range) | 19 (12–53) | 18.5 (12–51) | 20 (12–51) | 0.70 |
| % Patients with perceived LLD | 31 | 26 | 26 | 0.36 |
| % Patients with limpa | 16 | 12 | 16 | 0.54 |
aDefined as patients who indicated that they limped most or all of the time on the OHS
Discussion
This large-scale postal audit survey found the prevalence of patient-perceived LLD after THR to be 30%. This is in agreement with previous research findings that approximately a third of patients are aware of an LLD after THR [7, 12]. Although nearly a third of patients perceived an LLD, only half of these patients reported that they were bothered by the discrepancy. This finding is again in agreement with previous research which reported that half of patients with LLD were disturbed by the inequality [12]. A possible reason why only half of patients felt they were affected by the LLD is that the LLD was minimal in these patients and therefore had little impact upon their lives. Because no measure of the magnitude of LLD was included in this study it is not possible to test this hypothesis, although the extent of LLD has been found to correlate with the awareness of the problem, abnormal gait and the use of a shoe raise [12]. A shoe raise may be one device patients use to minimise the impact of LLD upon their functional ability. In this study, the use of a shoe raise was common, with a third of patients with perceived LLD reporting that they used a shoe raise.
Although the prevalence of patient-perceived LLD was high, radiographic analysis of a random sample of patients who reported LLD found that only 36% of patients had anatomical LLD. Therefore, the perception of LLD is higher than actual LLD. This could be due to several reasons, including pelvic obliquity, alteration in proprioception around the hip or a manifestation of general dissatisfaction. However, even though in many cases LLD is not anatomical LLD, the patient perception of LLD is high, and it is therefore important that patients are counselled pre-operatively about the risk of perceived LLD.
This study found that the OHS and the frequency of LLD and limping were not significantly different with the CPT, Exeter and Charnley, suggesting that patients had similar outcomes after THR, irrespective of the femoral stem prosthesis. When LLD was present, it had a significant negative impact on functional outcome after primary THR. Patients who reported a perceived LLD had a significantly worse OHS than those patients who thought their legs were the same length. Also limping was more prevalent among patients with perceived LLD, compared to patients without LLD. Although the results suggest an association between LLD and poorer functional outcome, a causal relationship between LLD and outcome cannot be assumed, as other factors could have resulted in the poorer OHS for patients with an LLD.
Similar to our study, Konyves and Bannister [7], found that patients with a lengthening of the operative leg had a poorer OHS that those patients with a shorter or equal leg length. In contrast, another study that assessed 200 patients undergoing THR found that radiographic evidence of LLD did not correlate with patient function [10]. In this study, the lack of correlation between LLD and functional outcome could be due to the use of the Harris Hip Score [13] and the SF-36 [14] to assess outcome. The Harris Hip Score is a surgeon-based tool and there is considerable evidence demonstrating a lack of agreement between surgeon and patient assessment of health status, particularly in subjective domains such as pain [15]. The SF-36 is a generic tool and as such lacks the specificity and sensitivity of other disease-specific or joint-specific questionnaires [16]. Therefore, the lack of correlation between LLD and functional outcome in the study by White and colleagues [10] could be a result of the questionnaires used to measure outcomes. A strength of our study was the use of the OHS which is a joint-specific outcome measure and more sensitive to change than both generic and disease-specific measures of health [17].
The limitations of our study need to be acknowledged when interpreting the results. A lack of a clinical or radiographic assessment for all patients who reported an LLD means that the aetiology of the LLD could not be determined in all cases. Another limitation of this study is that the survey questions did not ask patients to specify whether their operative leg was longer or shorter than the contralateral leg. Therefore, the prevalence of shortened and lengthened legs after THR cannot be determined although previous research has found that patients were significantly more likely to detect an LLD if the leg was over-lengthened on the operative side [7].
This study also has several strengths. To the authors’ knowledge, this is the largest reported postal survey determining the prevalence of patient-perceived LLD after THR. Because the survey assessed perceived LLD at 5–8 years post-operative, this eliminated transient, short-term LLD from being included in the prevalence estimates. Sampling was not influenced by patient selection bias because all consecutive patients operated upon over a 3-year period were included in the survey. Also the use of a validated joint-specific questionnaire to determine the impact of LLD on functional outcome lends sensitivity to the study. The results suggest that patient self-report of perceived leg length inequality can be a useful method for obtaining large-scale data on LLD and could be an effective tool to be used in place of labour-intensive radiographic analysis and unreliable clinical measurements of LLD [9].
In conclusion, perceived LLD is highly prevalent at 5–8 years after primary THR, affecting 30% of patients, although not all these patients will have anatomical LLD. Of the patients with perceived LLD, half were bothered by the LLD and over a third used a shoe raise to equalise leg lengths. Patients with perceived LLD experienced a significantly poorer functional outcome and reported more limping than those patients without LLD. This study highlights the importance of informing patients pre-operatively of the high risk of perceived LLD after primary THR and the associated negative impact this may have on their outcome.
References
- 1.Ulf L. The Danish Hip Arthroplasty Register. Acta Orthop Scand. 2000;71:433–439. doi: 10.1080/000164700317381081. [DOI] [PubMed] [Google Scholar]
- 2.Nikolajsen L, Brandsborg B, Lucht U, Jensen TS, Kehlet H. Chronic pain following total hip arthroplasty: a nationwide questionnaire study. Acta Anaesthesiol Scand. 2006;50:495–500. doi: 10.1111/j.1399-6576.2006.00976.x. [DOI] [PubMed] [Google Scholar]
- 3.Barrack RL, Paprosky W, Butler RA, Palafox A, Szuszczewicz E, Myers L. Patients’ perception of pain after total hip arthroplasty. J Arthroplasty. 2000;15:590–596. doi: 10.1054/arth.2000.6634. [DOI] [PubMed] [Google Scholar]
- 4.Boutron I, Poiraudeau S, Ravaud JF, Baron G, Revel M, Nizard R, Dougados M, Ravaud P. Disability in adults with hip and knee arthroplasty: a French national community based survey. Ann Rheum Dis. 2003;62:748–754. doi: 10.1136/ard.62.8.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nilsdotter AK, Petersson IF, Roos EM, Lohmander LS. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study. Ann Rheum Dis. 2003;62:923–930. doi: 10.1136/ard.62.10.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MacWilliam CH, Yood MU, Verner JJ, McCarthy BD, Ward RE. Patient-related risk factors that predict poor outcome after total hip replacement. Health Serv Res. 1996;31:623–638. [PMC free article] [PubMed] [Google Scholar]
- 7.Konyves A, Bannister GC. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005;87:155–157. doi: 10.1302/0301-620X.87B2.14878. [DOI] [PubMed] [Google Scholar]
- 8.Austin MS, Hozack WJ, Sharkey PF, Rothman RH. Stability and leg length equality in total hip arthroplasty. J Arthroplasty. 2003;18:88–90. doi: 10.1054/arth.2003.50073. [DOI] [PubMed] [Google Scholar]
- 9.Turula KB, Friberg O, Lindholm TS, Tallroth K, Vankka E. Leg length inequality after total hip arthroplasty. Clin Orthop Relat Res. 1986;202:163–168. [PubMed] [Google Scholar]
- 10.White TO, Dougall TW. Arthroplasty of the hip. Leg length is not important. J Bone Joint Surg Br. 2002;84:335–338. doi: 10.1302/0301-620X.84B3.12460. [DOI] [PubMed] [Google Scholar]
- 11.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–190. [PubMed] [Google Scholar]
- 12.Edeen J, Sharkey PF, Alexander AH. Clinical significance of leg-length inequality after total hip arthroplasty. Am J Orthop. 1995;24:347–351. [PubMed] [Google Scholar]
- 13.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 14.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Mantyselka P, Kumpusalo E, Ahonen R, Takala J. Patients’ versus general practitioners’ assessments of pain intensity in primary care patients with non-cancer pain. Br J Gen Pract. 2001;51:995–997. [PMC free article] [PubMed] [Google Scholar]
- 16.Fitzpatrick R, Dawson J. Health-related quality of life and the assessment of outcomes of total hip replacement surgery. Psychol Health. 1997;12:793–803. doi: 10.1080/08870449708406740. [DOI] [Google Scholar]
- 17.Ostendorf M, Stel HF, Buskens E, Schrijvers AJ, Marting LN, Verbout AJ, Dhert WJ. Patient-reported outcome in total hip replacement. A comparison of five instruments of health status. J Bone Joint Surg Br. 2004;86:801–808. doi: 10.1302/0301-620X.86B6.14950. [DOI] [PubMed] [Google Scholar]