Abstract
Between January 2000 and December 2003, a total of 83 patients (64 men and 19 women, average age: 56.4 years, range: 42–78 years) who underwent posterior laminectomy and instrumented fusion for ossification of the posterior longitudinal ligament (OPLL) were included in this study to investigate the long-term outcome of this surgical option and clarify which factors affect the prognosis. After an average 4.8-year follow-up, the mean Japanese Orthopaedic Association (JOA) score significantly increased from 9.2 ± 1.3 points before operation to 14.2 ± 0.9 points at the latest follow-up (P < 0.01). The improvement rate (IR) of neurological function ranged from 11.1 to 87.5%, with a mean of 62.4 ± 13.2%. Among 83 patients, 59 (71.1%) patients had a good prognosis (IR ≥ 50%), and the other 24 (28.9%) patients had a poor prognosis (IR < 50%). Postoperative nerve root palsy was the main complication in this series. Radiographic study showed that whilst improving cervical lordosis could provide a better decompression effect and good prognosis, it could have simultaneously contributed to the high incidence of postoperative nerve root palsy.
Résumé
Entre janvier 2000 et décembre 2003, 83 patients (64 hommes et 19 femmes) dont la moyenne d’âge était de 56,4 ans (42 – 78) ont bénéficié d’une laminectomie supérieure avec instrumentation et greffe pour une opération visant une OPLL avec évaluation du pronostic à long terme et détermination des facteurs pouvant le modifier. Après un suivi de 4 à 8 ans, le score de la JOA a été nettement amélioré passant de 9,2 (± 1,3) avant l’opération à 14,2 (± 0,9), au dernier suivi (p < 0,01). Le taux d’amélioration neurologique (IR) est passé de 11,1% à 87,5% avec une moyenne de 62,4% ± 13,2%. Parmi ces 83 patients, 59 (71,1%) avaient un bon pronostic (IR 50%) et les autres, 24 (28,9%) avaient un mauvais pronostic (IR < 50%). La paralysie des fibres nerveuses est la complication la plus importante dans cette série. L’étude radiographique montre que l’amélioration de la lordose cervicale permet un effet de décompression plus important et un meilleur pronostic mais a contribué de façon simultanée à un taux important de paralysie des racines nerveuses en post-opérartoire.
Introduction
The surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament (OPLL) can be divided into the anterior approach and posterior approach. The anterior approach seems to be a radical surgical option, owing to resection of OPLL and direct decompression [4, 14]. However, when it comes to multilevel or severe OPLL, anterior decompression becomes more technically demanding and risky, and the posterior approach becomes an alternative option. Cervical laminoplasty has been one of the most widely used surgical treatments since the 1970s, and good results of laminoplasty have been published in many reports. However, several studies on long-term follow-up of laminoplasty revealed that cervical kyphosis and ossification progression were responsible for late neurological deterioration [8, 9, 12, 13, 15]. To provide stability of the decompressed levels and prevent progressive kyphosis, laminectomy and instrumented fusion were performed for multilevel severe OPLL in our hospital. The concerns of this study included the clinical outcome of this surgical option over a long-term follow-up period and which factors affect the clinical prognosis.
Materials and methods
Patient selection
Between January 2000 and December 2003, a total of 134 consecutive patients underwent laminectomy and instrumented fusion for cervical OPLL. The posterior approach was the first choice when (1) OPLL extended more than three levels, (2) OPLL occupied more than 50% diameter of the spinal canal or (3) OPLL was located above C2 or below C7. To evaluate the clinical outcome of this surgical option for the treatment of cervical OPLL, cases were excluded from this study with (1) associated ossification of the ligamenta flava (OLF) in the cervical spine, (2) ectopic ossification in the thoracic spine and (3) spinal cord injury due to trauma. This study included 83 patients (64 men and 19 women) who underwent laminectomy and instrumented fusion. The mean age at operation was 56.4 years, ranging from 42 to 78 years.
Surgical technique
Under general anaesthesia, patients were placed prone in a plaster bed. Before operation, proper position of the cervical spine was confirmed by intraoperative radiography. After exposure of the posterior elements, holes were drilled in the lateral masses bilaterally from C3 to C7 using the technique described by Magerl. The decompression level extended to C2 according to the spinal cord compression on magnetic resonance imaging (MRI), and if C2 was included in the fusion, holes were placed in the pedicles. A fixation system of screws and rods (Cervifix, Synthes, Switzerland, or CD Horizon M6, Medtronic Sofamor Danek, Memphis, TN, USA) was installed and the axis rods were bent to match the cervical curvature. The posterior elements including spinous processes and laminae were removed medially to either lateral mass. The facet joints at the involved levels were fused with the bone grafts taken from the spinous processes and laminae. After operation, all patients were given a Philadelphia collar for two to four weeks.
Radiological evaluation
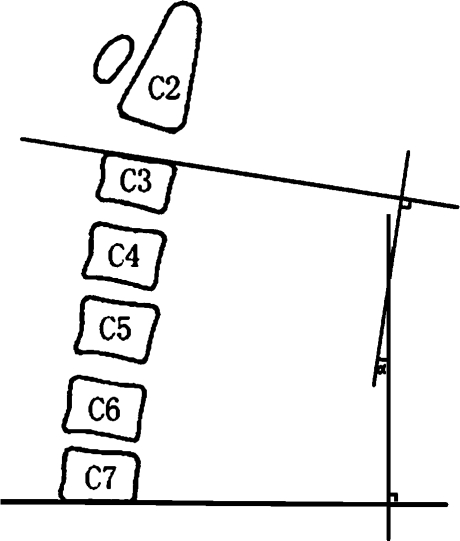
The parameters of plain radiographs, computed tomography (CT) and MRI described as follows were investigated: (1) cervical lordosis: measured as the angle between a line vertical to the superior aspect of the C3 vertebral body and the inferior aspect of the C7 body (Fig. 1); (2) occupying rate: defined as the thickness of OPLL divided by the anteroposterior diameter of the bony spinal canal on the axial CT image; (3) type of OPLL: classified as local, segmental, continuous or mixed-type; (4) extent of OPLL: number of involved vertebrae; and (5) snake-eye sign: presence of high signal intensity of the spinal cord on a T2-weighted MR image.
Fig. 1.
Cervical lordosis: Cobb angle of C3-7
Clinical assessment
The Japanese Orthopaedic Association (JOA) scoring system was used to evaluate the neurological status. An improvement rate (IR) was calculated as IR = (postoperative JOA score − preoperative JOA score/17 − preoperative JOA score)×100%. The neurological status of the patients at the final follow-up was used for defining clinical prognosis. Good prognosis was defined as IR ≥ 50% and poor prognosis was defined as IR < 50%.
Statistical analysis
For statistical analysis of the results, the Mann-Whitney U test and Pearson’s χ2 test were done using SPSS, version 11.0. The results were considered significant when the P value was less than 0.05.
Results
Clinical outcome
The whole follow-up period lasted 4.0–6.5 years, with an average of 4.8 years. Neurological status of all patients was assessed before operation, after operation and every year until to the last follow-up. The mean JOA score increased from 9.2 ± 1.3 points to 12.8 ± 1.1 points after operation and was 14.2 ± 0.9 points at the last follow-up. The neurological status was significantly improved at the last follow-up (P < 0.01), and the IR of neurological function ranged from 11.1 to 87.5%, with a mean of 62.4 ± 13.2%. Among 83 patients, 59 (71.1%) patients had a good prognosis (IR ≥ 50%), and the other 24 (28.9%) patients had a poor prognosis (IR < 50%). According to the results of this series, clinical characteristics including age, gender, duration of symptoms, preoperative JOA score and diabetes mellitus did not significantly influence neurological prognosis (Table 1).
Table 1.
Clinical characteristics of the patients with different prognoses
| Good prognosis | Poor prognosis | Sum total | P value | |
|---|---|---|---|---|
| Age at operation (years) | 55.6 ± 6.4 | 58.2 ± 7.6 | 56.4 ± 7.2 | 0.212 |
| Gender (n) | ||||
| Male | 45 | 19 | 64 | 0.334 |
| Female | 14 | 5 | 19 | |
| Duration of symptoms (years) | 3.4 ± 1.1 | 4.2 ± 1.3 | 3.7 ± 0.9 | 0.182 |
| Preoperative JOA score (points) | 9.8 ± 1.4 | 7.9 ± 1.5 | 9.2 ± 1.3 | 0.102 |
| Diabetes mellitus (n) | ||||
| Yes | 34 | 12 | 46 | 0.072 |
| No | 25 | 12 | 37 |
Radiological findings
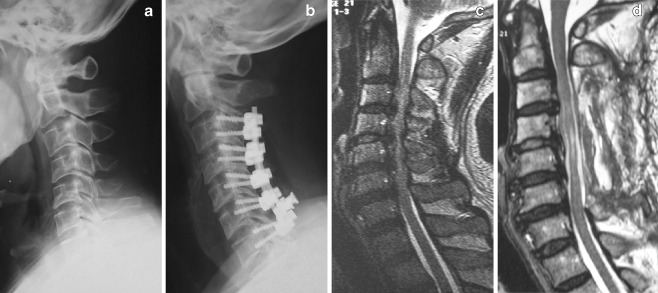
The results of preoperative radiological evaluation showed that preoperative cervical lordosis averaged 8.6 ± 2.4°. The mean occupying rate reached 43.5 ± 8.2% in the axial CT image. The sagittal type of OPLL was distributed as follows: local type n = 11, segmental type n = 17, continuous type n = 24 and mixed type n = 31. The ossification lesion extended an average of 3.7 ± 0.4 vertebrae. The snake-eye sign appeared in a total of 65 (78.3%) patients. The results grouped by neurological prognosis are detailed in Table 2, and no significant difference was observed when preoperative radiological evaluation was compared between the two groups. However, the clinical prognosis was significantly related to postoperative cervical lordosis (16.1 ± 1.5° vs 10.4 ± 1.3°, P < 0.01). Postoperative MR images showed that the patients with lordotic cervical alignment could expect a better decompressive effect of the spinal cord (Fig. 2).
Table 2.
Radiological findings of the patients with different prognoses
| Good prognosis | Poor prognosis | Sum total | P value | |
|---|---|---|---|---|
| Cervical lordosis (°) | ||||
| Before operation | 8.5 ± 2.6 | 8.9 ± 2.1 | 8.6 ± 2.4 | 0.273 |
| After operation | 16.1 ± 1.5 | 10.4 ± 1.3 | 14.2 ± 1.1 | < 0.01 |
| Occupying rate (%) | 42.6 ± 8.5 | 45.7 ± 10.1 | 43.5 ± 8.2 | 0.114 |
| Type of OPLL (n) | ||||
| Local type | 7 | 4 | 11 | 0.143 |
| Segmental type | 12 | 5 | 17 | |
| Continuous type | 17 | 7 | 24 | |
| Mixed type | 22 | 9 | 31 | |
| Extent of OPLL (vertebrae) | 3.6 ± 0.5 | 3.9 ± 0.7 | 3.7 ± 0.4 | 0.294 |
| Snake-eye sign (n) | ||||
| Yes | 22 | 16 | 65 | 0.082 |
| No | 18 | 8 | 18 |
Fig. 2.
Preoperative and postoperative radiographs showed that cervical lordosis was significantly increased after operation (a, b). Preoperative and postoperative MR images showed that the spinal cord shifted posteriorly to provide sufficient decompression (c, d)
Complications
There were no patients with iatrogenic neurological deterioration after operation. Complications after posterior laminectomy and instrumented fusion included postoperative nerve root palsy in ten cases (seven C5 palsy, two C6 palsy and one C7 palsy), haematoma in three cases and screw pull-out in two cases (Table 3). The time of nerve root palsy development ranged from six to 48 hours postoperatively, and the strength of paralysed muscles decreased to grade 1–2 on the manual muscle test (MMT). Conservative treatment only was used for all of the patients, including neurotrophy drugs, high-pressure oxygen therapy and functional exercises. The strength of the involved muscles recovered to 3–4 on the MMT after six months to one year. The three patients who developed haematoma recovered neurological function after an emergency operation. There was no instance of rod breakage in this series, but three screws pulled out from the lateral masses in two asymptomatic patients and no further surgery was required.
Table 3.
Complications in the patients who underwent laminectomy and instrumented fusion
| Complications | No. of patients |
|---|---|
| Neurological complications | |
| C5 palsy (complete recovery) | 5 |
| C5 palsy (incomplete recovery) | 2 |
| C6 palsy (complete recovery) | 2 |
| C7 palsy (complete recovery) | 1 |
| Haematoma paralysis (complete recovery) | 3 |
| Hardware failure | |
| Screw pull-out (asymptomatic) | 2 |
To clarify the pathogenic mechanism of segmental nerve root palsy, which was the main complication of this series and significantly influenced the short-term clinical outcome, we also investigated the radiological findings which could be associated with nerve root palsy. The results revealed that the patients with palsy tended to have increased cervical lordosis (13.5 ± 3.0° vs 3.9 ± 1.1°, P < 0.05), but there was no significant positive correlation with severity of OPLL (occupying rate) and presence of the snake-eye sign in MR images (Table 4).
Table 4.
Radiological findings of the patients with nerve root palsy
| Palsy | No palsy | P value | |
|---|---|---|---|
| Cervical lordosis (°) | |||
| Before operation | 5.2 ± 3.2 | 9.1 ± 1.6 | 0.087 |
| After operation | 18.9 ± 1.4 | 13.4 ± 1.7 | 0.116 |
| Increase | 13.5 ± 3.0 | 3.9 ± 1.1 | < 0.05 |
| Occupying rate (%) | 45.6 ± 10.8 | 43.1 ± 8.2 | 0.126 |
| Snake-eye sign (n) | |||
| Yes | 8 | 57 | 0.147 |
| No | 2 | 16 |
Discussion
Some controversies still exist over the surgical options for cervical myelopathy due to OPLL. In general, anterior decompression by cervical corpectomy and resection of OPLL seems to be an ideal surgical option, and posterior decompression (laminoplasty or laminectomy) is an alternative choice for multilevel severe OPLL, when the anterior approach is fraught with iatrogenic neurological dangers. In addition, multilevel vertebrectomies with anterior instrumentation for patients with OPLL is associated with a high incidence of graft dislodgement and instrument failure [5, 11, 19]. Although uninstrumented laminoplasty and laminectomy relieved cord compression, poor results were seen after these procedures when progressive kyphosis resulted in neurological deterioration [1, 12, 18]. Saruhashi et al. reported that 30% of patients developed kyphosis during a mean five-year follow-up after laminoplasty, and earlier uninstrumented laminectomy series reported higher rates of changes in alignment [17]. The nuchal musculature was important in stabilisation of the cervical spine in lordosis, and detachment of these muscles results in significant atrophy, which decreases the effect of the posterior tension band. Furthermore, uninstrumented laminoplasty does not address the dynamic forces in the pathogenesis of OPLL. If substantial segmental instability still remains after laminoplasty, it is possible that progression of OPLL will be accelerated and the damage to the injured spinal cord will continue. The incidence of progression of OPLL after laminoplasty has been reported at 70–73%, and this risk is greater with increasing length of follow-up [9, 13, 15]. Therefore, the authors considered that laminoplasty had limitations in terms of preventing the development of kyphosis and further increase in OPLL, which could have a deleterious effect on long-term outcome.
On the other hand, laminectomy with instrumented fusion produces immediate and long-term stability of the decompressed levels [6, 7, 10]. There was no statistical change in the cervical alignment as measured by the Cobb angle, nor was there any individual patient in whom kyphotic deformity developed over at least four years of follow-up in this study. Although cervical laminectomy and fusion has been evaluated in a few studies, potential benefits of cervical stability for the treatment of OPLL have never been addressed. In this series, the neurological outcome of patients treated with laminectomy and instrumented fusion was comparable to that reported in series of patients with multilevel OPLL treated with laminoplasty. However, the neurological function of these patients achieved more improvement in the long-term follow-up, and no individual patient developed neurological deterioration. The authors considered that avoidance of cervical deformity and maintenance of alignment were the most important reasons for the excellent long-term outcomes reported here. In addition, segmental stability after instrumented fusion made significant progression of OPLL unlikely to occur.
Several factors affecting the prognosis after anterior decompression and laminoplasty have already been reported by some researchers, but little is known about the factors affecting prognosis after laminectomy and instrumented fusion for the treatment of OPLL. Choi et al. reviewed 47 patients who underwent anterior corpectomy and fusion for OPLL and confirmed diabetes mellitus as a potential risk factor [3]. Another series of 47 patients with OPLL who underwent laminoplasty were followed up for 5–11 years by Baba et al. and late results were poor in patients who had greater than 50% compromise of the spinal canal by the ossified lesion [2]. In this retrospective study, the authors included a relatively large number of cases and analysed clinical and radiological variables to obtain a prognostic overview of patients with OPLL after this procedure. Among all of the variables, the results of this study clearly indicated that postoperative cervical alignment significantly influenced the prognosis of these patients. In the patients with kyphotic angulation of the cervical spine, the decompressed spinal cord may move backless and still be bowstringed against anterior OPLL. Yamazaki et al. concluded that posterior laminoplasty has no decompression effect when cervical lordosis was less than 10° [20]. In this series, in order to increase cervical lordosis and improve the decompression effect, proper position of the cervical spine was confirmed by radiography before operation and axis rods of the posterior fixation were bent to restore the cervical curvature during operation. However, there were still a minority of patients in whom the cervical lordosis did not significantly improve, resulting in poor prognosis. The stiffness of the cervical spine of these patients with OPLL was possibly responsible for this result.
Postoperative nerve root palsy was among the most common complications of the patients undergoing cervical surgery, and the mean incidence has been reported to be 8.3% (range: 3.2–28.6%) in those with OPLL [16]. The pathogenesis of this complication still remains to be clarified and no risk factors have been confirmed as yet. In this study, the radiographic analyses revealed that postoperative nerve root palsy was associated with increased cervical lordosis, which was probably because increased cervical lordosis increased the spinal cord shift together with tethering effect on the nerve roots. Therefore, while improving the cervical lordosis to achieve a greater decompression effect, we should be cautious of the high incidence of nerve root palsy as observed.
Based on the results of this study, posterior laminectomy and instrumented fusion represented an effective alternative surgical option for multilevel severe OPLL and can provide a long-term stable outcome. Radiographic study showed that improving cervical lordosis whilst providing a better decompression effect and good prognosis, simultaneously contributed to the high incidence of postoperative nerve root palsy.
References
- 1.Albert TJ, Vaccaro A. Postlaminectomy kyphosis. Spine. 1998;23:2738–2745. doi: 10.1097/00007632-199812150-00014. [DOI] [PubMed] [Google Scholar]
- 2.Baba H, Imura S, Kawahara N, et al. Osteoplastic laminoplasty for cervical myeloradiculopathy secondary to ossification of the posterior longitudinal ligament. Int Orthop. 1995;19:40–45. doi: 10.1007/BF00184913. [DOI] [PubMed] [Google Scholar]
- 3.Choi S, Lee SH, Lee JY, et al. Factors affecting prognosis of patients who underwent corpectomy and fusion for treatment of cervical ossification of the posterior longitudinal ligament: analysis of 47 patients. J Spinal Disord Tech. 2005;18:309–314. doi: 10.1097/01.bsd.0000161236.94894.fc. [DOI] [PubMed] [Google Scholar]
- 4.Epstein N. Anterior approaches to cervical spondylosis and ossification of the posterior longitudinal ligament: review of operative technique and assessment of 65 multilevel circumferential procedures. Surg Neurol. 2001;55:313–324. doi: 10.1016/S0090-3019(01)00464-5. [DOI] [PubMed] [Google Scholar]
- 5.Hee HT, Majd ME, Holt RT, et al. Complications of multilevel cervical corpectomies and reconstruction with titanium cages and anterior plating. J Spinal Disord Tech. 2003;16:1–9. doi: 10.1097/00024720-200302000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Heller JG, Edwards CC, II, Murakami H, et al. Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: an independent matched cohort analysis. Spine. 2001;26:1330–1336. doi: 10.1097/00007632-200106150-00013. [DOI] [PubMed] [Google Scholar]
- 7.Houten JK, Cooper PR. Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: effects on cervical alignment, spinal cord compression and neurological outcome. Neurosurgery. 2003;52:1081–1088. doi: 10.1227/01.NEU.0000057746.74779.55. [DOI] [PubMed] [Google Scholar]
- 8.Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: clinical results and limitations of laminoplasty. Spine. 2007;32:647–653. doi: 10.1097/01.brs.0000257560.91147.86. [DOI] [PubMed] [Google Scholar]
- 9.Kawagchi Y, Kanamori M, Ishihara H, et al. Progression of ossification of the posterior longitudinal ligament following en bloc cervical laminoplasty. J Bone Joint Surg Am. 2001;83-A:1798–1802. doi: 10.2106/00004623-200112000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Kumar VG, Rea GL, Mervis LJ, et al. Cervical spondylotic myelopathy: functional and radiographic long-term outcome after laminectomy and posterior fusion. Neurosurgery. 1999;44:771–778. doi: 10.1097/00006123-199904000-00046. [DOI] [PubMed] [Google Scholar]
- 11.Macdonald RL, Fehlings MG, Tator CH, et al. Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg. 1997;86:990–997. doi: 10.3171/jns.1997.86.6.0990. [DOI] [PubMed] [Google Scholar]
- 12.Masaki Y, Yamazaki M, Okawa A, et al. An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament: anterior decompression with spinal fusion versus laminoplasty. J Spinal Disord Tech. 2007;20:7–13. doi: 10.1097/01.bsd.0000211260.28497.35. [DOI] [PubMed] [Google Scholar]
- 13.Matsunaga S, Sakou T, Taketomi E, et al. Clinical course of patients with ossification of the posterior longitudinal ligament: a minimum 10-year cohort study. J Neurosurg. 2004;100(Suppl 3):245–248. doi: 10.3171/spi.2004.100.3.0245. [DOI] [PubMed] [Google Scholar]
- 14.Mizuno J, Nakagawa H. Ossified posterior longitudinal ligament: management strategies and outcomes. Spine J. 2006;6:282–288. doi: 10.1016/j.spinee.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 15.Ogawa Y, Toyama Y, Chiba K, et al. Long-term results of expansive open-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine. 2004;1:168–174. doi: 10.3171/spi.2004.1.2.0168. [DOI] [PubMed] [Google Scholar]
- 16.Sakaura H, Hosono N, Mukai Y, et al. C5 palsy after decompression surgery for cervical myelopathy: review of the literature. Spine. 2003;28:2447–2451. doi: 10.1097/01.BRS.0000090833.96168.3F. [DOI] [PubMed] [Google Scholar]
- 17.Saruhashi Y, Hukuda S, Katsuura A, et al. A long-term follow-up study of cervical spondylotic myelopathy treated by “French window” laminoplasty. J Spinal Disord. 1999;12:99–101. [PubMed] [Google Scholar]
- 18.Tani T, Ushida T, Ishida K, et al. Relative safety of anterior microsurgical decompression versus laminoplasty for cervical myelopathy with a massive ossified posterior longitudinal ligament. Spine. 2002;27:2491–2498. doi: 10.1097/00007632-200211150-00013. [DOI] [PubMed] [Google Scholar]
- 19.Vaccro AR, Falatyn SP, Scuderi GJ, et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11:410–415. [PubMed] [Google Scholar]
- 20.Yamazaki A, Homma T, Uchiyama S, et al. Morphologic limitations of posterior decompression by midsagittal splitting method for myelopathy caused by ossification of the posterior longitudinal ligament in the cervical spine. Spine. 1999;24:32–34. doi: 10.1097/00007632-199901010-00008. [DOI] [PubMed] [Google Scholar]