Abstract
Humeral shaft fractures respond well to conservative treatment and unite without much problem. Since it is uncommon, there is not much discussion regarding the management of nonunion in the literature, and hence this is a challenge to the treating orthopaedic surgeon. Osteoporosis of the fractured bone and stiffness of the surrounding joints compounds the situation further. The Ilizarov fixator, locking compression plate, and vascularised fibular graft are viable options in this scenario but are technically demanding. We used a fibular strut graft for bridging the fracture site in order to enhance the pull-out strength of the screws of the dynamic compression plate. Six patients in the study had successful uneventful union of the fracture at the last follow-up. The fibula is easy to harvest and produces less graft site morbidity. None of the study patients needed additional iliac crest bone grafting. This is the largest reported series of patients with osteoporotic atrophic nonunion of humerus successfully treated solely using the combination of an intramedullary fibular strut graft and dynamic compression plate.
Résumé
Les fractures de l’humérus répondent bien au traitement conservateur avec une bonne consolidation. Concernant les pseudarthroses, la littérature est assez controversée et ceci reste un traitement difficile pour les chirurgiens orthopédistes, notamment en ce qui concerne l’ostéoporose et la raideur des articulations adjacentes. Le fixateur externe d’Ilizarov, les plaques en compression, les greffes vascularisées sont des possibilités techniques et thérapeutiques. Nous avons utilisé des fragments de péroné pontant le foyer de fractures associés à une plaque dynamique en compression. Les patients dans cette étude ont eu un bon résultat avec consolidation de la fracture au dernier suivi. Le péroné est un site intéressant pour le prélèvement des greffons, avec peu de morbidité. Aucun patient n’a nécessité un complément de greffes iliaques. Cette étude est la plus importante concernant une série de patients présentant une pseudarthrose athrophique avec ostéoporose au niveau de l’humérus traités avec succès par l’utilisation combinée de greffes de péroné intra médullaire et d’une plaque dynamique en compression.
Introduction
Nonunion of the humerus is an uncommon complication of diaphyseal fractures. Its reported rate in the literature is quite variable, ranging from 1 to 10% [3, 11]. It can be successfully managed by various surgical methods with the principles being open reduction, freshening of edges and stabilisation using plate and screws, interlocking nails, or an external fixator [4, 5, 8, 9]. Supplementing fixation with cancellous bone graft has been found to achieve union reliably. Osteoporosis is a common factor confounding longstanding nonunion of humerus due to disuse, old age, or following multiple surgeries. It is a challenge to successfully achieve osteosynthesis with plates in such ununited osteoporotic bones [1, 10]—hence, the evolution of polymethyl methacrylate with screws [2, 12] and locking compression plates (LCP). LCPs are advantageous in this situation but high cost and availability are concerns in developing countries. Interlocking nails or external fixators are not viable options in these elderly patients as the adjacent joints may already be stiff at the time of presentation. We treated six patients with nonunion of osteoporotic humerus shaft successfully using a combination of an intramedullary fibular strut graft and dynamic compression plate and screws. This is the consecutive experience of two medical centres.
Patients and methods
Six patients with nonunion of osteoporotic humeral shafts were treated prospectively at two tertiary referral centres from 2005 to 2007 using an intramedullary fibular strut graft and dynamic compression plate (DCP). Indication for osteosynthesis using the fibular strut and DCP in this study was a diaphyseal fracture of the humerus which had remained ununited for at least four months and was associated with severe osteoporosis and pencil-thin cortices. Patients with an excessively scarred, indurated soft-tissue envelope or with a poor blood supply were excluded and treated by a vascularised fibular transfer and hence excluded from the study. Because of the rarity and complexity of this specific problem it was not possible to include a control group.
Average age of the patients was 65.33 years (range, 54–84). There were four females and two males (Table 1). Five patients had involvement of left humerus and only one on the right side. Three patients each had fractures of mid-shaft and junction of middle and proximal thirds. Five were closed fractures and one open fracture had eventual atrophic nonunion upon presentation. All patients had mild pain, tenderness and gross abnormal mobility at the nonunion site, and limitation of activities of daily living. All patients had stiffness of shoulder and elbow to varying degrees. Average delay at presentation from the time of injury was 13.33 months (range, 7–26 months). Preoperative DASH score averaged 84±5 (range, 77–97). Two patients each had diabetes mellitus and ischemic heart disease and three had hypertension. None of the patients were smokers. Five patients with closed fractures had nonunion following conservative treatment.
Table 1.
Patients with osteoporotic humerus nonunion included in the study
| Case number | Age (y) | Gender | Side of fracture | Time since fracture (mo) | Prior treatment | Last follow-up (months) |
|---|---|---|---|---|---|---|
| 1 | 56 | F | L | 9 | Native | 15 |
| 2 | 67 | F | L | 7 | Conservative | 19 |
| 3 | 76 | F | R | 13 | Native | 11 |
| 4 | 55 | M | L | 26 | Two surgeries | 13 |
| 5 | 54 | F | L | 10 | Conservative | 24 |
| 6 | 84 | M | L | 15 | Native | 13 |
All patients underwent surgery under general anaesthesia after administration of prophylactic antibiotics. Mid-shaft fractures and fractures at the junction of middle and lower thirds were exposed through a posterior approach with care taken to identify and protect the radial nerves. Fractures at the junction of proximal and middle thirds were treated through an anterolateral approach. Fracture fragments were freshened off the devitalised bone and fibrous tissue up to the point of bleeding bone ends, and the medullary canal was opened using a drill. Both fragments were then reamed progressively using serial hand reamers up to the point of reaching the fairly healthy cortical bone.
The mid-shaft of fibula was then harvested under tourniquet control with care taken to identify and protect the superficial peroneal nerve. Fibular shaft of excess length was harvested so that it could be trimmed as necessary. Three sides of the fibula were trimmed so as to enable it to snugly telescope into the fracture fragments across the fracture site. If the thickness did not permit its use, it was conversely bevelled at two ends leaving behind the full thickness shaft in the middle which later would bridge the nonunion site or bone defect more effectively. The strut was pushed into one of the fracture fragments and the exact length of graft that needed trimming was assessed. Once the final shaping of the graft was done, the fracture was reduced with the intramedullary fibular graft spanning the fracture site.
Osteosynthesis across the fracture site was achieved using a dynamic compression plate and screws in compression mode. An additional Muller’s compression device was used at one end of the plate to achieve intraoperative compression at the fracture site in all patients. At least three screws on each side of the fracture with three or four cortical purchase for each of the screws were attempted. The remaining excess pieces of fibular graft were packed longitudinally bridging the fracture site. None of the patients had iliac crest bone grafting. Patients with elbow and shoulder stiffness underwent passive joint manipulation at the end of surgery. All patients were protected in an arm sling for a period of three weeks after the surgery. Elbow and shoulder mobilisation was initiated aggressively after three weeks. Lifting of weights using the operated limb was deferred for a period of three months or until osseointegration of the fibular ends or fracture healing.
At final follow-up, the patients were examined by an independent observer clinically and radiologically. Symptoms of pain, instability, or dysfunction were recorded, and the movement of adjacent joints was measured. Intra- and postoperative complications were documented. Radiographs of the humerus in two orthogonal planes were examined for the presence of bridging bony trabeculae, indicating union, as well as for evidence of loosening or breakage of the implants. Fractures were considered united if at least three of the cortices on radiographs showed evidence of bony trabeculae crossing the fracture site.
Results
All fractures had solid clinico-radiologically evident fracture union by the three-month follow-up, and patients were very satisfied with the treatment (see examples in Figs. 1, 2, 3). There were no wound problems. The average arm shortening was 1.56±1.1 cm (range, 0.5–2.6 cm). The patient with radial nerve injury required a tendon transfer surgery six months after nonunion surgery. Patients were followed-up for an average of 15.83 months (range, 11–24 months). None had pain over the fracture site and the DASH score at the last follow-up averaged 28 ±13 (range, 9–43). Although three patients had some discomfort over the fibular graft harvest site, none had any pain or problems at the last follow-up.
Fig. 1.
Seven-month-old nonunion fracture midshaft humerus in a 67-year-old woman treated with intramedullary strut fibular graft and DCP fixation showing good osseointegration of fibula at 19-month follow-up
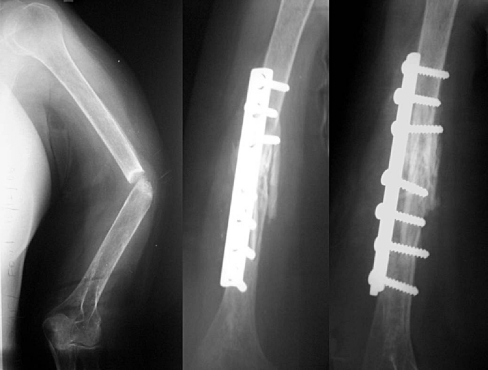
Fig. 2.
13-month-old fracture proximal third humerus in a 76-year-old woman treated with anterolateral plating in addition to fibular strut grafting with excellent radiological union at 11-month follow-up
Fig. 3.
A 45-year-old male patient with type IIIA open fracture shaft of humerus and radial nerve injury had undergone plate fixation. When infected nonunion was diagnosed at three months, plate removal was performed. After the infection settled at six weeks, revision surgery using unicortical fibular graft and limb reconstruction system application was performed. The fibular graft resorbed and the patient had nonunion with loosening of the external fixator two years after the fracture. The fixator was removed and antibiotics were administered for six weeks prior to definitive index surgery. There was good incorporation of fibula at the 13-month follow-up
There was an average loss of ten degrees abduction and 15 degrees flexion of the shoulder. There was no change in shoulder rotations following surgery. All patients with preoperative fixed flexion deformity of elbow to varying degrees had persistence of similar deformity at the last follow-up. Range of motion of the elbow had improved by 15 degrees following surgery. All patients had gone back to their near normal pre-injury activity levels at the last follow-up.
One of the patients had intraoperative splintering of the distal fracture fragment at the tip of the plate which healed in the ‘U’ plaster slab over a period of six weeks without affecting the outcome. None of the implants had loosening or breakage at the last follow-up. Two patients had developed superficial wound infections postoperatively, but delayed suture removal and oral antibiotics were sufficient to resolve these problems. One patient had transient common peroneal nerve palsy which recovered spontaneously at six-weeks follow-up. At the last follow-up, none of the patients had any morbidity due to fibular graft harvest.
Discussion
The incidence of nonunion after humeral shaft fractures is generally reported as low because of the favourable results of nonoperative and, on strict indication, surgical treatment. Hence there is little literature on the results of repair of nonunion of the humeral shaft [3, 11]; nonunion is likely to be related to the severity of initial injury, transverse pattern of fracture, or soft-tissue interposition. Failure to unite after surgical treatment may be due to poor contact between the bone ends, inadequate stabilisation, devitalisation of bone, osteopenia, and bone defects. Obesity, alcoholism, and method of treatment may also be contributory factors.
Osteoporosis, either as a result of disuse or due to generalised metabolic causes, compounds the choice of surgical treatment in these patients. It significantly reduces the pullout strength of the screws thus increasing the chance of implant failure. Humeral nonunion in osteoporotic bone presents a reconstructive challenge for the treating orthopaedic surgeon [1, 10]. While a number of methods of managing atrophic fracture nonunion have been suggested, each has its drawbacks. Most surgeons favour the use of an interlocking nail, Ilizarov external fixator, or LCP for stabilisation and vascularised fibular graft or cancellous iliac crest bone graft for enhancement of fracture union [9].
Interlocking nails require an image intensifier and are technically demanding. Their use is also known to hinder the shoulder movements in the short term, although the long term results are comparable with that of plating. Patients with nonunion of the humerus usually present with some stiffness of the adjacent joints and nailing may in fact worsen it. But, nailing has the advantages of being a load sharing device and affords stable fixation of the nonunion site even in osteoporotic bones. Bone transport using distraction histogenesis in the treatment of complex post-traumatic problems has a certain appeal, but enthusiasm for the Ilizarov technique has been tempered by its complexity and technical difficulty, the commitment of time and resources required for a good result, and the potential for numerous complications [4, 6, 8].
Locking compression plates are very promising, especially in this clinical scenario, but their use is limited due to problems with cost and availability. The dynamic compression plate is a familiar implant and easy to use by all surgeons. It is also more economical for patients. Plate fixation for nonunion humerus has been widely described in the literature. The main complications with this method include screw back-outs, radial paralysis, and infection. Dynamic compression plates fixed with screws having six or eight cortical purchases on either side of the fracture are often sufficient provided the bone quality is adequate to hold the plate and screws in place until fracture union [7]. Some authors have tried the use of methyl methacrylate bone cement along with the cortical screws to enhance the pull-out strength successfully; but it adds to the cost and has the potential for cardio toxicity.
Iliac crest cancellous bone graft has no mechanical strength to withstand stresses prior to solid union of the fracture site and also is associated with quite significant graft harvest site morbidity. The fibula transmits one eighth of body weight and can be as useful as vascularised or nonvascularised graft in reconstruction of bony defects. Vascularised bone grafting requires surgical experience and equipment not readily available in every hospital. The technique is demanding of time and resources, and vascular thrombosis may compromise the result [5]. Nonvascularised fibula is easy bone to harvest with the least possible tissue trauma. When harvesting the fibula transplant, a few centimetres of the epiphyseal portions have to be left in place so as not to interfere with the joints involved. The portion harvested is therefore almost completely cortical in character. The cortical bone affords immediate structural continuity and stability at the fracture site. It also has some osteogenic potential in addition to acting like a strut across the fracture site when used as an intramedullary bone graft. Fibula is probably the most suitable donor bone for reconstruction of defects in a long bone because of its length, geometrical shape, and mechanical strength. Grafts of cortical bone revascularise slowly and incompletely. There is a substantial risk of infection, delayed union and nonunion, and fractures through the graft are common. Although it is believed that skeletal reconstruction with bone grafts frequently fails because the surrounding soft tissue cannot provide adequate vascularity for graft incorporation and, even if successful, only results in slow revascularisation of the dead graft by creeping substitution, we did not find any graft being resorbed or failing. The fibular graft harvest has also been reported to have a high potential for peroneal nerve paralysis but if adequate care is taken to identify and protect the nerve during exposure, this complication can well be prevented. There is a moderate cost of fibular harvest regarding operating time, hospital stay, nursing cost, walking problems, crutches, etc.
We recommend dynamic compression screw plate fixation (six or eight cortices on either side of the nonunion) associated with an intramedullary fibular strut bone graft. The results in our series with almost no complications favour this easy and reliable option. Three or four cortical purchase of screws through the DCP enhances the pullout strength of the screws in osteoporotic patients. The fibula acts as a filler in the medullary cavity preventing abnormal movement. None of the screws backed out in this study as of the last follow-up. In this study, there was an attempt to achieve compression at the fracture site using the Muller’s compression device. Although some surgeons have studied enhanced pullout strength of screws in osteoporotic bones with addition of polymethyl methacrylate, we consider this option to be a nonbiological solution to the problem of osteoporosis and to add to the cost and duration of surgery [2, 12].
Conclusions
An intramedullary fibular strut graft across the fractured site in conjunction with compression plating successfully achieves union without the need for simultaneous or further cancellous iliac crest bone graft in osteoporotic atrophic nonunion humerus. The technique is easy, familiar, economical, and confronted with less bone graft harvest site morbidity. The fibula acts as an internal splint to the fracture site, aiding stability of osteosynthesis and also increasing the number of cortical purchase of the screws used in fixing the plate, thus increasing the pull-out strength of the screws. Intramedullary positioning in addition to load sharing, also helps bone ongrowth and osseointegration. Bone peg graft bevelled conversely at both ends and leaving full thickness fibula at the nonunion site adds to the limb length in addition to affording mechanical stability to the fixation construct. This technique may find future application in lower limb long bone fracture nonunion.
References
- 1.Ansell RH, Scales JT. A study of some factors which affect the strength of screws and their insertions and holding power in bone. J Biomechanics. 1968;1:279–302. doi: 10.1016/0021-9290(68)90023-7. [DOI] [PubMed] [Google Scholar]
- 2.Cameron HU, Jacob R, MacNab I, Pillar RM. Use of polymethylmethacrylate to enhance screw fixation in bone. J Bone Joint Surg [Am] 1975;57-A:655–656. [PubMed] [Google Scholar]
- 3.Epps CH, Jr, Grant RE. Fractures of the shaft of the humerus. In: Rockwood CA Jr, Green DP, Bucholz RW, editors. Rockwood and Green’s fractures in adults, vol 1. 3. Philadelphia, etc: J. B. Lippincott Co.; 1991. pp. 843–869. [Google Scholar]
- 4.Ilizarov GA. Transosseous osteosynthesis: theoretical and clinical aspects of the regeneration and growth of tissue. Berlin: Springer; 1992. [Google Scholar]
- 5.Jupiter JB. Complex non-union of the humeral diaphysis: treatment with a medial approach, an anterior plate, and a vascularized fibular graft. J Bone Joint Surg [Am] 1990;72-A:701–707. [PubMed] [Google Scholar]
- 6.Kocaoglu M, Eralp L, Tomak Y. Treatment of humerus shaft non-unions by the Ilizarov method. Int Orthop. 2001;25:396–400. doi: 10.1007/s002640100295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar A, Sadiq SA. Nonunion of the humerus shaft treated by internal fixation. Int Orthop. 2002;26:214–216. doi: 10.1007/s00264-002-0354-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paley D. Problems, obstacles and complications of limb lengthening by the Ilizarov technique. Clin Orthop. 1990;250:81–104. [PubMed] [Google Scholar]
- 9.Rosen H. The treatment of nonunions and pseudarthroses of the humeral shaft. Orthop Clin North Am. 1990;21:725–742. [PubMed] [Google Scholar]
- 10.Schatzker J, Sanderson R, Murnaghan JP. The holding power of orthopaedic screws in vivo. Clin Orthop. 1975;108:115–126. doi: 10.1097/00003086-197505000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Taylor JC. Delayed union and nonunion of fractures. In: Crenshaw AH, editor. Campbell’s operative orthopaedics, vol 2. 8. St Louis, etc: Mosby Year Book; 1992. pp. 1329–1332. [Google Scholar]
- 12.Trotter DH, Dobozi W. Nonunion of the humerus: rigid fixation, bone grafting and adjunctive bone cement. Clin Orthop. 1986;204:162–168. [PubMed] [Google Scholar]