Abstract
A Bristow-Latarjet procedure with specific instrumentation was performed for recurrent dislocation or subluxation of the glenohumeral joint in 34 patients. The procedure was performed through a subscapularis splitting approach with three specific instruments and a special screw. The clinical outcome was assessed by the Duplay and the Constant scores. Radiographic study was conducted on 23 patients and CT scan in 11 patients. Of the 27 patients interviewed 92% were satisfied. Of the 23 patients examined, 15 had an excellent Duplay score, four a good score, three a medium score, and only one had a bad score. One patient had subluxation episodes, and one patient was revised after a redislocation following violent trauma. On the standard radiographs, all bone blocks were in the correct position. A pseudarthrosis was diagnosed in the patient with subluxation episodes. This device simplifies the surgical technique and provides reproducibility to the procedure.
Résumé
Le procédé de Bristow-Latarjet avec une instrumentation spécifique a été utilisé dans les luxations ou les sub-luxations récidivantes de l'épaule sur 34 patients en utilisant un abord suscaplulaire à l'aide d'instruments spécifiques et d'une vis spéciale. Le suivi clinique a été évalué selon le score de Duplay et de Constant. L'évaluation radiologique réalisée sur 23 patients avec un scanner chez 11 patients. Sur les 27 patients interrogés, 92% étaient satisfaits. Sur les 23 patients examinés 15 avaient un excellent score de Duplay, 4 un bon score, 3 un score moyen et un seul un mauvais score. Un patient présentait des épisodes de subluxations résiduelles et un patient a été réopéré après une récidive de la luxation secondaire à un violent traumatisme. Sur les radiographies standard, toutes les butées osseuses sont en position correcte. Une pseudarthrose a été diagnostiquée chez le patient présentant des épisodes de subluxations. Ce matériel simplifie la technique chirurgicale et permet d'avoir une technique reproductible.
Introduction
Despite the development of arthroscopic techniques, the Bristow-Latarjet procedure remains widely used in Europe as first-line treatment for recurring dislocation of the shoulder or in cases of failure of the Bankart repair [13]. The difficulty in the procedure is to accurately position the coracoid bone block by a surgical approach which spares the subscapularis muscle [5, 14, 24]. The deleterious consequences of bone block malpositioning and nonunion are well documented in the literature [1, 3, 7, 9, 12, 17, 18, 20, 21, 24], in particular recurrent instability if the bone block is too medial or is pseudarthrosed, or arthritis if the bone block is overhanging. This is why we have developed specific instrumentation for the optimal preparation, positioning, and fixation of the bone block. The objective of this study is to report outcomes in 34 cases of patients treated with this technique.
Materials and methods
From March 1999 to January 2005, 34 patients underwent surgery by the senior author using this technique. There were 31 men and three women. The mean age was 32 years (range 20–58 years). The dominant side was involved in 95% of the cases. The average interval between the first shoulder dislocation and surgery was 5.2 years (range 0.5–30). Thirty patients had had at least two true anteromedial dislocations, four patients had subluxations. Ten patients had chronic pain. No patient had previous surgery to the affected shoulder. Only one of the 34 patients had hyperlaxity. Preoperatively, the patients underwent a complete clinical examination performed by the same examiner, a standard radiographic examination, and a CT scan examination in 45% of the cases. There were 28 cases of glenoid wear, five cases of glenoid fracture, and one patient with no bony glenoid lesion. A Hill-Sachs lesion was present in 31 patients. There was no preoperative arthritis. Eleven patients practised a throwing sport, six practised a resisted-throwing sport, and ten practised a zero-risk sport (e.g. jogging, diving).
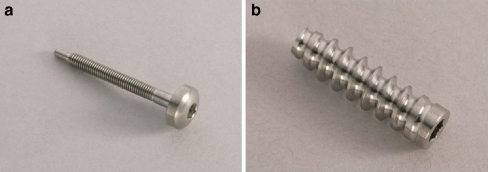
The device includes an implant and an instrumentation tool. The implant is a titanium special screw; it consists of a glenoid anchor screw and a bone block compression screw (Orthomed S.A., St Jeannet, France) (Fig. 1).
Fig. 1.
The special screw (Orthomed S.A., St Jeannet, France). a Bone block compression screw. b Glenoid anchor screw
The instrumentation consists of three instruments. A sizer for measuring the diameter (10 or 12 mm) of the coracoid process and a guide to cut to fit the desired diameter. A cannulated square awl (Fig. 2) is used to position the coracoid and hold its position with a guide pin fitted through the instrument. A double-barrel cannulated drill bit (10 or 12 mm in diameter), which is used in one manoeuvre, prepares the housing of the glenoid anchor screw and produces a cylindrical pit which will receive the base of the coracoid bone block. Bone block fixation is effected by the special screw. The glenoid anchor screw (length 17 mm, diameter 5.8 mm) acts as a plug in the glenoid, and receives the compression screw (length 30 or 35 mm, diameter 3 mm) which fixes and compresses the coracoid.
Fig. 2.
The cannulated square awl
Operative procedure
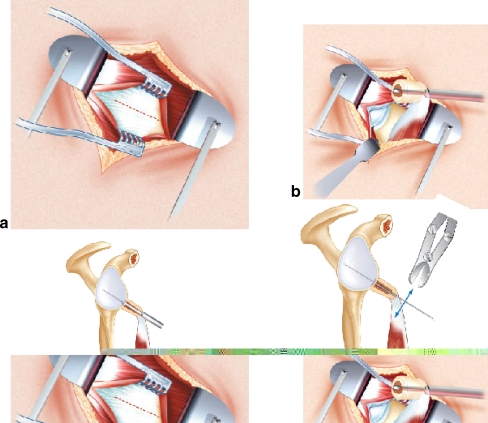
After a deltopectoral approach, the coracoid bone block is harvested and its base is shaped into a calibrated cylinder. The prepared bone block should pass through one of the holes of the sizer (10 or 12 mm in diameter). A 3.2 mm diameter hole is drilled through the bone block for the compression screw. Next, the subscapularis muscle is incised in line with its fibres at the junction of the inferior one-third and superior two-thirds. After performing a horizontal capsulotomy, the anterior inferior part of the glenoid is exposed. The bone block is fitted to the end of the cannulated square awl and positioned at the anterior inferior rim of the glenoid. Once the bone block site has been determined, the square awl is hammered into the bone. The core of the square hole is unscrewed and removed. A guide pin is passed through the square hole and is power-driven about 3 cm into the glenoid. The cannulated square awl is removed, and the guide pin is cut flush with the bone block. Thus, the bone block site is accurately maintained throughout the operation (Figs. 3 and 4).
Fig. 3.
a Articular capsule exposed through a subscapularis splitting approach. b The prepared coracoid process is fitted to the end of the cannulated square awl. c The core of the square hole is removed and a guide pin is passed through the square hole and driven into the glenoid. d The cannulated square awl is removed, and the guide pin is cut flush with the bone block
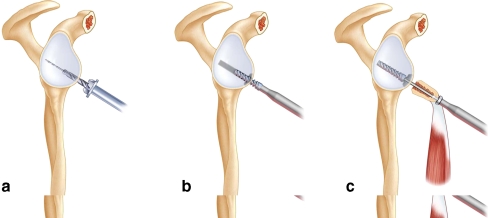
Fig. 4.
a The double-barrel cannulated drill bit is centred with the guide pin to perform a dual action: drill the hole for the glenoid anchor screw, then, at the end of travel, drill a small cylindrical pit which will accommodate the bone block. b The glenoid anchor screw is fully buried into the glenoid. c The coracoid screw loads the bone block and screws into the anchor screw
The motor-mounted double-barrel cannulated drill bit is centred with the guide pin to perform a dual action: drill the hole for the glenoid anchor screw, then, at the end of travel, drill a small cylindrical pit which will accommodate the bone block. The glenoid anchor screw is fully buried into the glenoid. The coracoid screw loads the bone block and screws into the anchor screw.
After screwing the bone block, it is checked for the absence of impingement between the capsule and coracoid in external rotation and between the head and bone block. Postoperatively, the patient is immobilised with the elbow against the body for ten days. Physiotherapy starts on the third day.
Evaluation
All of the patients (n = 34) were reviewed between the third and sixth months postoperatively and assessed for anatomical, radiographic, and functional outcome. Seven patients were lost to follow-up after this first evaluation. Second-look assessment was done in a longer term, at an average of 24.4 months (range 7–74 months) by an independent observer. This assessment was clinical and radiographic (n = 23) or by telephone (n = 4). The patients were questioned about instability, stiffness, sensation of loss of strength, and the activity and level of sport were indicated. The clinical outcome was assessed by the Duplay score [22] and by the Constant [4] score. Subscapularis muscle strength was measured using a spring balance.
The radiographic study was conducted on 23 patients with a frontal shoulder view, a lateral Lamy view, and a glenoid profile view. It was used to look for pseudarthrosis, lysis of the bone block, fracture, or migration. The vertical position of the bone block relative to the equator according to Hovelius et al. [9] was determined in the frontal view and the lateral Lamy view. The position of the bone block relative to the joint space was measured in millimetres on the glenoid profile view. The Samilson and Prieto [16] criteria were used to classify possible glenohumeral arthritis.
A CT scan of the operated shoulder without injection of contrast was taken in 11 patients. This CT study provided information as to union of the bone block, the existence of glenohumeral arthritis, and lysis of the bone block. The position of the bone block relative to the joint space was measured on the axial sections.
Results
Complications
We observed a superficial scar infection, which was treated topically, with no effect on the overall result. No neurovascular complications were observed in this series.
Clinical results
Of the 27 patients interviewed, 92% were satisfied. Of the 23 patients examined, 15 had an excellent Duplay score (between 90 and 100 points), four had a good score (between 76 and 90), three had a medium score (60), and only one had a bad score (50). The Constant score was 93.5% on average compared to the score of the untreated side (86–100%).
Of the 27 patients interviewed, one patient had subluxation episodes. One patient was revised after a new anteromedial dislocation following violent trauma (rugby) at three months. After revision surgery, this patient was satisfied and had a stable shoulder. Of the 23 patients reviewed clinically, only the patient complaining of subluxation was apprehensive about wind-up, and none complained of a sensation of instability (Table 1).
Table 1.
Results of apprehension test
| Apprehension test result | Number of patients (N = 23) |
|---|---|
| Negative | 22 |
| Positive | 1 |
On average, the loss of mobility in internal rotation was 0.9 vertebrae (range 0–7). The loss in external rotation was 7.1° (range 0–40°) on average (Table 2).
Table 2.
Average loss of external and internal rotation
| Type of rotation | Average loss of rotation |
|---|---|
| External | 7.1° (range 0–40°) |
| Internal | 0.9 vertebrae (range 0–7) |
Only three patients had a loss in external rotation of more than 20° relative to the unoperated side. The telephone interview did not reveal reduced mobility. On average, the patients had a reduction in subscapularis strength of 14% relative to the unoperated side (0–35%). Of the 27 patients questioned about their pain, 88% had no pain or minimal pain from heavy exertion.
On average, a return to sport was done at six months postoperative (range 3–12 months). Sixteen of the 22 patients (72%) practising a sport could return to sport at their former level. Ninety percent of the patients returned to sport after the operation.
Radiographic results
In this series of patients, followed according to a radiographic protocol (n = 23), we found only one case of stage I arthritis in a patient who had a very good functional outcome. On the standard radiographs, all the bone blocks were in a subequatorial position. On the glenoid profile view, all the bone blocks were located between 1 and 2 mm from the joint space.
A pseudarthrosis was diagnosed from the standard radiographs with unscrewing of the coracoid screw in a patient with subluxation episodes. This represents a pseudarthrosis rate of 4.3%. Five patients had lysis of the proximal one third of the bone block around the screw head, with no effect on the overall result. In one patient, the bone block completely disappeared at nine months, with an objective overall result assessed as good, and a stable, minimally painful shoulder (Table 2).
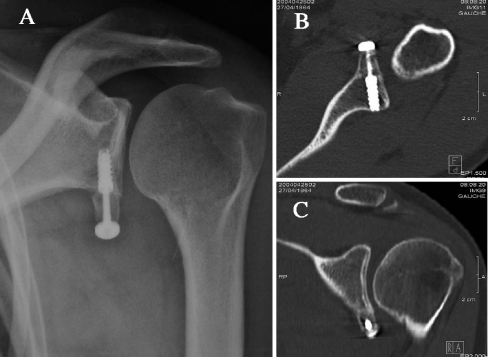
CT results
The CT study (n = 11) revealed arthritic lesions in another patient whose radiographs seemed normal. A humeral osteophytosis and anterior narrowing of the glenohumeral space were found in the patient reviewed at 40 months who had the most limited external rotation of the series. With regard to the bone block position, CT scan confirmed the subequatorial position of the eleven bone blocks. It showed that eight bone blocks were flush with the anterior inferior rim of the glenoid between 1 and 2 mm, only one was more medial at 4 mm with a good result on stability, and three were at less than 1 mm from the surface with no visible arthritic lesion (Fig. 5).
Fig. 5.
Example of a case: 40-year-old male, six months post op. a AP view. b Axial CT scan. c Coronal CT scan
The eleven bone blocks were in a subequatorial position. The pseudarthrosis diagnosed on a standard radiograph was confirmed by the CT scan with the coracoid screw unscrewing without dismantling the device.
Discussion
Bone block positioning
In the conventional horizontal approach to the subscapularis muscle, bone block positioning is difficult [14, 24]. The cannulated square awl and the guide pin make it easy to localise the final position of the graft throughout the operation. There can be no involuntary change since everything will be performed along this guide pin.
Many authors have studied the bone block position on the radiographs. In 56 patients operated by the Latarjet technique, Allain et al. [1] observed 53% too lateral bone blocks and 5% too medial bone blocks, with the others considered as perfect. In the series by Cassagnaud et al. [3], more than 10% of the bone blocks were found overhanging on the CT scans. Hovelius et al. [9] found 36% of bone blocks malpositioned above the equator and 6% too medially placed bone blocks. Huguet et al. [12] found 45% of the grafts overhanging in the joint. All of these works stressed the importance of the graft position, which is directly related to the final result. That is, a too lateral or overhanging bone block leads to arthritis in the more or less long term [3, 7, 9, 12, 14, 20, 21, 24] and limits internal rotation through head-coracoid impingement [12]. A too medial bone block will result in postoperative recurrent instability [9, 12, 23], and a bone block located above the equator also exposes the joint to recurrent dislocation [9]. The optimum position is difficult to define but it is recognised that it should be below the equator, neither too medial nor too lateral (less than 10 mm from the cartilage for some [9], less than 2 mm for others [12]). For some, the bone block should really be flush to increase the articular surface of the glenoid, reduced by passage lesions. In our series, no bone block was overhanging on the standard radiographs. The CT study showed that eight bone blocks were flush with the anterior inferior rim of the glenoid fossa between 1 and 2 mm, only one was more medial at 4 mm with a good result on stability, and three bone blocks were less than 1 mm from the surface without visible arthritic lesion. The patient with glenohumeral arthritis had a bone block positioned between 1 and 2 mm from the joint space.
In addition, the analysis of the CT scans revealed that some bone blocks which seemed to be very close to the joint space on the radiographs were actually quite a distance from the cartilage. As regards the obliqueness of the graft relative to the joint space, the measurements were so disparate that we could draw no conclusions. It can be imagined, however, that it may play a role in possible impingement between the humeral head and bone block. It would be interesting to perform a CT scan on a greater scale and over a longer period to study the relation between bone block obliqueness and the occurrence of glenohumeral arthritis.
As to position in the vertical plane, all the bone blocks in the series were positioned below the equator, and the supplementary CT study confirmed the radiographic findings.
Pseudarthrosis
In our series, admittedly of small size, only one out of the 23 radiographed bone blocks did not heal. In the literature [1, 2, 6, 9–12, 14, 15, 17–19, 24, 25], this rate is highly variable, from 0 to 50%. Many authors demonstrated that nonunion of the bone block had an impact of the final result. For Cassagnaud et al. [3], the existence of pseudarthrosis impairs all the revision parameters; for Hovelius et al. [9–11], it increases the rate of postoperative instability; for Guity et al. [8], it causes pain; and for Wymenga and Morshuis [25] it impairs the mobility outcome.
The sturdiness of the set-up is related to the freshening of the anterior inferior rim of the glenoid and synthesis of the bone block. The coracoid bone block position varies with the surgeon. Fixing the bone block with two screws would be less prone to pseudarthrosis, while the vertical bone block would be more so, although there are no references on this matter. It seems likely, however, that the vertical bone block is more stressed by the short head of the biceps brachii, and it is certain that it offers less bone contact with the glenoid and can accept only one screw. By using a double system including a glenoid anchor screw and coracoid screw, compression screwing is ensured. The conventional fixation described in the literature uses either a 3.5-mm diameter bicortical screw or a 4.5-mm diameter malleolar screw. Several problems have been described in the literature about this mode of fixation. For Huguet et al. [12], Walch et al. [22], and Vander Maren et al. [21], fixation with a 3.5-mm screw can be held responsible for a large number of complete lyses. As regards the 4.5-mm screws, they may be the source of fractures because of their size. Therefore a compromise should be found between a bulky screw showing strong fixation and a smaller diameter screw which does not weaken the bone block. We propose a screw with a small proximal diameter (3 mm) which anchors into a larger-diameter plug to provide strong fixation by compression screwing. Only one complete lysis of the bone block was found in our series.
Overall, this specific instrumentation simplifies the surgical technique and provides some reproducibility to the procedure which is not easily achieved using conventional instruments.
References
- 1.Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998;80(6):841–852. doi: 10.2106/00004623-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Barry TP, Lombardo SJ, Kerlan RK, Jobe FW, Carter VS, Shields CL, Jr, Yocum LA, Tibone JE. The coracoid transfer for recurrent anterior instability of the shoulder in adolescents. J Bone Joint Surg Am. 1985;67(3):383–387. [PubMed] [Google Scholar]
- 3.Cassagnaud X, Maynou C, Mestdagh H. Clinical and computed tomography results of 106 Latarjet-Patte procedures at mean 7.5 year follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2003;89(8):683–692. [PubMed] [Google Scholar]
- 4.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop. 1987;214:160–164. [PubMed] [Google Scholar]
- 5.Decker MJ, Tokish JM, Ellis HB, Torry MR, Hawkins RJ. Subscapularis muscle activity during selected rehabilitation exercises. Am J Sports Med. 2003;31(1):126–134. doi: 10.1177/03635465030310010601. [DOI] [PubMed] [Google Scholar]
- 6.Gazielly D. Results of anterior coracoid abutments performed in 1995: apropos of 89 cases. Rev Chir Orthop Reparatrice Appar Mot. 2000;86(Suppl 1):103–106. [PubMed] [Google Scholar]
- 7.Glorion C. Résultats radiographiques des butées dans les luxations antérieures récidivantes de l’épaule. Rev Chir Orthop Reparatrice Appar Mot. 1991;77(Suppl 1):186–190. [Google Scholar]
- 8.Guity MR, Roques B, Mansat P, Bellumore Y, Mansat M. Painful or unstable shoulder after coracoid transfer: result of surgical treatment. Rev Chir Orthop Reparatrice Appar Mot. 2002;88(4):349–358. [PubMed] [Google Scholar]
- 9.Hovelius L, Korner L, Lundberg B, Akermark C, Herberts P, Wredmark T, Berg E. The coracoid transfer for recurrent dislocation of the shoulder. Technical aspects of the Bristow-Latarjet procedure. J Bone Joint Surg Am. 1983;65(7):926–934. [PubMed] [Google Scholar]
- 10.Hovelius L, Sandstrom B, Sundgren K, Saebo M. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study I–clinical results. J Shoulder Elbow Surg. 2004;13(5):509–516. doi: 10.1016/j.jse.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 11.Hovelius LK, Sandstrom BC, Rosmark DL, Saebo M, Sundgren KH, Malmqvist BG. Long-term results with the Bankart and Bristow-Latarjet procedures: recurrent shoulder instability and arthropathy. J Shoulder Elbow Surg. 2001;10(5):445–452. doi: 10.1067/mse.2001.117128. [DOI] [PubMed] [Google Scholar]
- 12.Huguet D, Pietu G, Bresson C, Potaux F, Letenneur J. Anterior instability of the shoulder in athletes: apropos of 51 cases of stabilization using the Latarjet-Patte intervention. Acta Orthop Belg. 1996;62(4):200–206. [PubMed] [Google Scholar]
- 13.Latarjet M. A propos du traitement des luxations récidivantes de l’épaule. Lyon Chir. 1954;495(8):994–997. [PubMed] [Google Scholar]
- 14.Matton D, Looy F, Geens S. Recurrent anterior dislocations of the shoulder joint treated by the Bristow-Latarjet procedure. Historical review, operative technique and results. Acta Orthop Belg. 1992;58(1):16–22. [PubMed] [Google Scholar]
- 15.Pihlajamäki H, Bötsman O, Rokkanen PA. Biodegradable expansion plug for fixation of the coracoid bone block in the Bristow-Latarjet operation. Int Orthop. 1994;18(2):66–71. doi: 10.1007/BF02484413. [DOI] [PubMed] [Google Scholar]
- 16.Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65(4):456–460. [PubMed] [Google Scholar]
- 17.Shively J, Johnson J. Results of modified Bristow procedure. Clin Orthop. 1984;187:150–153. [PubMed] [Google Scholar]
- 18.Singer GC, Kirkland PM, Emery RJ. Coracoid transposition for recurrent anterior instability of the shoulder. A 20-year follow-up study. J Bone Joint Surg Br. 1995;77(1):73–76. [PubMed] [Google Scholar]
- 19.Spoor AB, Wall Malefijt J. Long-term results and arthropathy following the modified Bristow-Latarjet procedure. Int Orthop. 2005;29(5):265–267. doi: 10.1007/s00264-005-0634-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Torg JS, Balduini FC, Bonci C, Lehman RC, Gregg JR, Esterhai JL, Hensal FJ. A modified Bristow-Helfet-May procedure for recurrent dislocation and subluxation of the shoulder. Report of two hundred and twelve cases. J Bone Joint Surg Am. 1987;69(6):904–913. [PubMed] [Google Scholar]
- 21.Vander Maren C, Geulette B, Lewalle J, Mullier J, Autrique JC, Thiery J, Deneufbourg J. Coracoid process abutment according to Latarjet versus the Bankart operation. A comparative study of the results in 50 cases. Acta Orthop Belg. 1993;59(2):147–155. [PubMed] [Google Scholar]
- 22.Walch G; the "Duplay" group (1987) Plaidoyer pour l’utilisation d’une fiche de cotation commune dans les instabilités de l’épaule. Communication au premier congrès pour la chirurgie de l’épaule et du coude, Paris
- 23.Walch G. La luxation récidivante antérieure d'épaule, table ronde SO.F.C.OT. Rev Chir Orthop Reparatrice Appar Mot. 1991;77(1):177–191. [Google Scholar]
- 24.Weaver JK, Derkash RS. Don't forget the Bristow-Latarjet procedure. Clin Orthop. 1994;308:102–110. [PubMed] [Google Scholar]
- 25.Wymenga AB, Morshuis WJ. Factors influencing the early results of the Bristow-Latarjet technique. Acta Orthop Belg. 1988;54(1):76–82. [PubMed] [Google Scholar]