Abstract
Degeneration of the meniscus and the articular cartilage in unicompartmental osteoarthritis of the knee results in progressive deformity of the leg axis. It is the aim of this study to evaluate if a leg axis correction can be achieved by implanting a customised metallic interpositional device for the knee (ConforMIS iForma™). Before and after implanting a ConforMIS iForma™ knee implant, a radiological analysis of the leg axis deviation in the frontal plane was performed prospectively in 27 patients by evaluating anteroposterior single-leg stance radiographs. We achieved a sufficient leg axis correction with an average correction of 3.8° and an averaged small under-adjustment of 0.9° by inserting the ConforMIS iForma™ interpositional knee implant. Apart from the primary treatment objective of articular surface restitution the ConforMIS iForma™ knee implant can be reliably used to correct axis deformity occurring with unicompartmental osteoarthritis of the knee.
Résumé
La déformation progressive du membre inférieur entraîne lorsqu’existe une arthrose mono-compartimentale un dégénérescence du ménisque et du cartilage articulaire homolatéral. Le but de cette étude est d’évaluer la correction d’axe par un implant métallique d’interposition au niveau du genou(ConforMIS iForma™). avant et après implantation de l’implant ConforMIS iForma™ une analyse radiologique prospective de la déviation des membres dans le plan frontal a été réalisée, chez 27 patients avec radiographies de face et de profil. il est possible grâce à ce matériel d’avoir une correction moyenne de 3,8° avec une hypo correction de 0,9°. compte-tenu de l’objectif que nous nous étions fixés, l’utilisation de cet implant (ConforMIS iForma™) au niveau du genou, permet d’avoir une correction fiable de l’axe lorsque l’on traite des athroses mono-compartimentales.
Introduction
Unicompartmental osteoarthritis in younger and active patients often requires the patient and the surgeon to decide whether to perform an osteotomy or whether to perform a unicompartmental joint replacement in spite of the patient’s age and activity level.
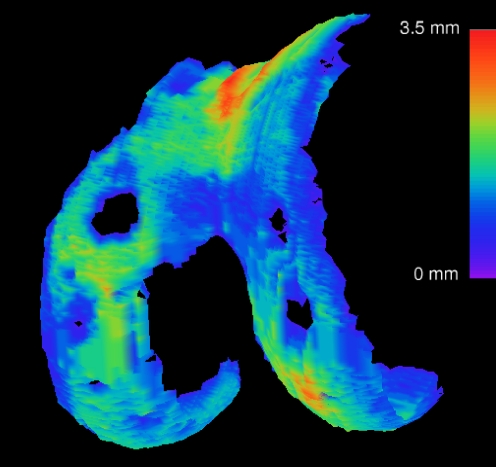
As an alternative to the established procedures, a new technique using a customised metallic interpositional device preserving the natural bone stock is available. The iForma™ implant is a minimally invasive, self-fixating version of metallic hemiarthroplasty as described by MacIntosh [15], McKeever [16] and Campbell [2]. By using a three-dimensional (3-D) sizing software, an individual medial or lateral interpositional implant can be generated based on the magnetic resonance imaging (MRI) data of the affected knee joint (Fig. 1). The device can be implanted using a minimally invasive technique with a 5-cm incision size. It is characterised by a highly constraining undersurface exactly mirroring the tibial plateau with resultant self-fixation on the tibia. The implant’s individual adaptation to each patient’s respective surface geometry guarantees a functionally stable fit of the implant. This is substantially different from the UniSpacer™ (Zimmer, Inc., Warsaw, IN, USA), which was designed to be free floating with anteroposterior (AP) motion of the implant and rotation during flexion and extension. The lack of fixation of the UniSpacer™ resulted in a high degree of dislocations based on its non-existent adaptation to the contours of the joint [6, 21, 22].
Fig. 1.
ConforMIS iForma™: example of medial implant
The aim of this paper was to determine if appropriate leg axis correction can be achieved by implanting a customised interpositional device for the knee and to examine the accuracy of the preoperative planning procedure.
Patients and methods
A prospective study with 27 patients presenting with early to moderate stage unicompartmental osteoarthritis of the knee (Kellgren-Lawrence grade 3 or below) [10] was approved by the local authorities and ethics commissions (No. 04/075) to be conducted from June 2005 to April 2007 in our department. In this study, a single surgeon implanted a total of 27 individual ConforMIS iForma™ (23 medially, 4 laterally; 20 left, 7 right). The implant was approved by the US Food and Drug Administration (FDA) in 2004 and CE certified in 2006. All sequential cases were included. The average age of the patients (15 women and 12 men) at the time of surgery was 55.3 years (38–67 years). Prior to enrollment in the trial, all patients had undergone at least one preliminary arthroscopic procedure with a partial and/or subtotal meniscus resection. In one case, the study was preceded by failed matrix-associated chondrocyte transplantation (MACI).
Pre-surgery MRI examination was done with cartilage-sensitive sequences (two-dimensional fast spin echo and 3-D spoiled gradient echo) according to the prescribed protocol.
With novel 3-D software, the extent of the cartilage loss as well as the thickness, curvature and topography of the residual cartilage can be determined from the extracted MRI data (Fig. 2). The implants were manufactured by taking the patient’s individual anatomy and the loss of cartilage substance in the affected compartment into consideration. The thickness of the implant results from the space offset between the implant’s surface and undersurface. This space is derived based on an estimate of the tibial and femoral cartilage loss calculated with the help of algorithms that compare the thickness of the anterior and posterior tibial and femoral cartilage.
Fig. 2.
Analysis of femoral cartilage thickness distribution
On average, the central and, at the same time, minimum implant thickness (offset) for the patients examined amounted to 3.3 mm (SD: 0.61; range: 2.0 to 4.1 mm).
The radiological examination was performed before surgery and 6 weeks postoperatively with the help of an AP single-leg stance image. Great care was taken to ensure that the femoral condyles were parallel to the frontal plane, which corresponded to the centre of the film. This was achieved by frontally aligning the patella while neutrally extending both knee joints. In the run-up of the study, the X-ray technicians received special training in this technique.
Surgical procedure
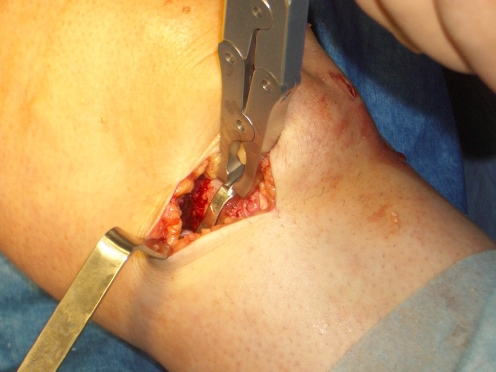
The surgical procedure always started with an arthroscopy. An arthroscopic resection of the posterior horn and body of the affected meniscus was performed down to the meniscus base (red zone). After removal of the arthroscope, a short parapatellar skin incision including the arthroscopy portal was made. The remaining anterior meniscal horn was resected with the meniscotome. If required, prominent femoral and tibial osteophytes were trimmed around the margins, and cartilage steps in transitional stages, from defective zones to the mostly intact surface of the dorsal femoral condyle, were smoothed out. In no case was any bone cut performed. Based on a specific production algorithm for each patient, only a unique implant with predetermined thickness was provided. With moderate valgus stress, the medial iFormas™ were inserted with a special grasper from an anterior and slightly medial position with light tilting and rolling movements (Fig. 3). At the same time, the knee joint was extended from a medium flexed position of about 45°. The insertion of the lateral iForma™ was performed from a lateral direction with the implant tilted to 45°. By using this technique all implants could be placed without serious problems. After placing the implant, the stable and optimal position of the implant was tested visually, by palpation and fluoroscopically.
Fig. 3.
iForma™: medial implantation with the grasper
Statistical analysis
With standardised pre- and postoperative long leg views, the deviation from the load axis of the surgically treated knee joint under stress was determined twice by two independent orthopaedic surgeons in separate readings on different days. The Kolmogorov-Smirnov test [12] was used to evaluate whether the distribution of the leg axis deviation followed a normal distribution (Gaussian distribution). This analysis demonstrated that none of the examiners produced results that represented a significant deviation from a normal distribution. The axis alignment between the two groups was determined with the non-paired t-test with a significance level of p < 0.05.
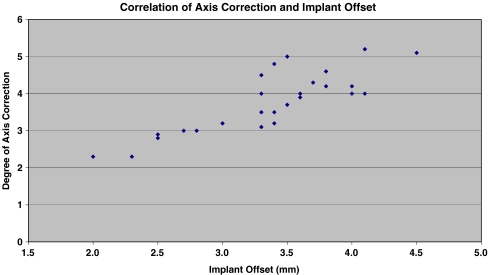
The correlation between axis correction and the respective minimum and central implant thickness (offset) was calculated with the Pearson product-moment correlation. The standard deviation for the achieved correction was also determined.
Results
The mean duration of the operation (incision to suture) was 47 min (34–102 min). The extended operating room (OR) time in some cases was the result of a difficult meniscectomy and the need for careful removal of osteophytes, especially in one case with 102 min OR time, where a dorsal osteophyte had to be removed. The incision was on average 5.2 cm (3.8–7.2 cm) long. There were no incidents of intra- or postoperative dislocations of the implant.
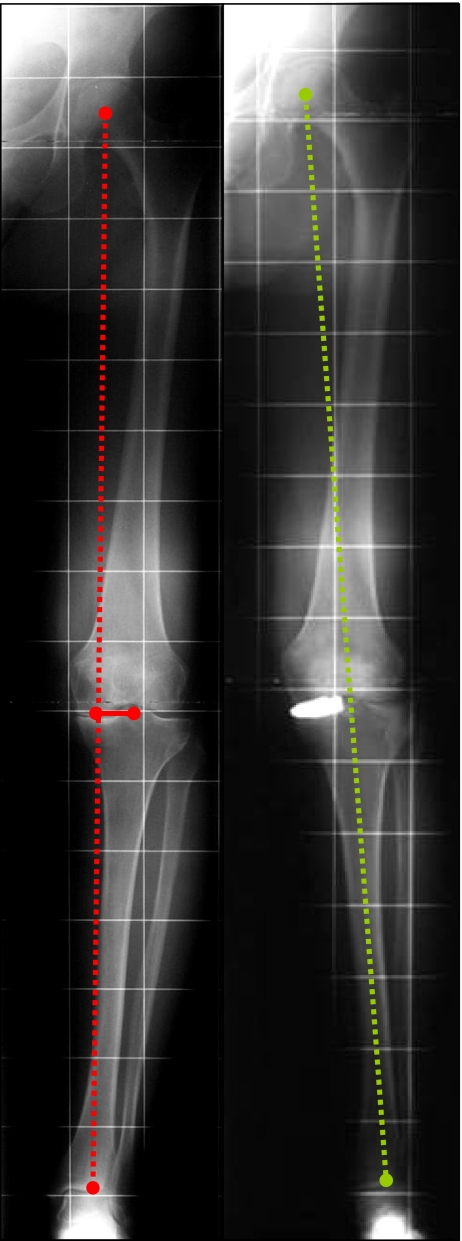
The objective was to correct the leg axis to 0° and/or to a slight under-correction up to 2°. It was reached in 23 of 27 cases (Fig. 4).
Fig. 4.
Mechanical axis before and after iForma™ implantation
In four cases (15%) the result was a slight over-correction (0.2°, 0.5°, two patients with 0.9°). The leg axis was corrected postoperatively from a preoperative average of −4.4° to a postoperative average of −0.9° (SD: 1.12°). The average extent of the correction was 3.8° (SD: 0.81°).
The correlation coefficient (r) between the implant offset and the extent of the axis correction amounted to 0.838, whereby according to Lienert [14] a correlation value of more than 0.8 can be deemed good (Fig. 5). The significance level for the accuracy with which the axis correction related to the implant thickness was achieved was p < 0.0001.
Fig. 5.
Correlation of axis correction and implant offset
In four cases in which new axis images were produced during random check-up a low correction loss average of 0.5° (0–1°) could be observed during a further period of up to 12–22 months.
Discussion
In recent years there has been a resurgence of interest in doing unicompartmental knee replacement [13]. Nevertheless high tibial osteotomy (HTO) is an established therapy for the treatment of symptomatic varus malaligned knees [3, 7]. For these methods good long-term results have been reported, but both are associated with certain problems for the patient over time. The HTO leads to an alteration of the ligament tensions and the kinematics of the joint which impedes component orientation and ligament balancing for the surgeon in subsequent total knee arthroplasty (TKA), which carries a higher rate of complications [19]. An additional consideration is progression of contralateral osteoarthritis as a result of HTO which has been described after 5 years in 60% of the patients [1, 9]. Unicondylar knee replacement is naturally associated with bone loss on the medial side which requires bone graft or metal wedge augmentation in cases of conversion to TKA [23]. In revision TKA in most cases it is wise to use a posterior stabilised design to deal with the danger of secondary PCL loosening [17]. The progression of the osteoarthritis in the contralateral compartment following unicondylar knee replacement could be detected in only 4% of patients after 8 years [4].
The literature dealing with the topic of totally unfixed interpositional knee devices is sparse. For the UniSpacer™ Sisto and Mitchell reported an increase of mean Knee Society function score from 60 preoperative to 69 postoperative and the mean Knee Society objective score from 62 points preoperative to 72 postoperative [22]. The reported data of axis correction with the UniSpacer™ device were based on 40 cm X-rays and thus not reliable [6]. The UniSpacer™ does not adapt to the shape of the joint and requires cartilage and bone removal. Unlike the McKeever device, the UniSpacer™ is not fixated on the tibia, but is designed to be free floating with AP motion and rotation. This implant resulted in a high rate of dislocations up to 16% and revisions up to 32% [6, 22]. Several authors therefore do not recommend its use [21, 22].
The ConforMIS iForma™ device follows the design rationale of the MacIntosh and McKeever devices: provides a functionally fixed tibial hemiarthroplasty. With the iForma™ device, functional fixation is achieved by adapting the device individually to the respective shape of the joint in the affected compartment in each patient while taking into account the difference in cartilage thickness from arthritic damage and the intact opposite compartment. The implant is highly constraining on the tibial surface and minimally constraining on the femoral surface, thereby functionally stabilising itself.
The optimal angle of correction is still under discussion for unicompartmental knee replacement [4, 20, 25]. For HTO an over-adjustment with a mechanical femorotibial axis between 2 and 5° valgus is desirable in medial varus gonarthritis [7, 18, 24]. For tibial hemiarthroplasty of the knee there is a complete lack of data.
Based on a series of 120 normal subjects of different gender and age Hsu et al. analysed the geometry of the knee joint using a full-length weight-bearing roentgenogram of the lower extremity. The mean femorotibial mechanical angle was 1.2° varus. Simulating a single-leg weight-bearing stance by shifting the upper body gravity closer to the knee joint in this study 75% of the knee joint load passed through the medial tibial plateau [8].
According to these results and the presupposition that a slight under-correction in regard to the neutral mechanical leg axis, as commonly recommended in unicondylar knee replacement [4], may avoid stress on the opposite untreated knee compartment we predetermined a target range of between 0 and 2° varus. A small under-correction amounted to an average of about 0.9° according to the ConforMIS iForma™ implantations performed in this study. In 23 of 27 cases, the intended leg axis correction in the target range was achieved.
Our data show that even without considering the preoperative axis deviation, the required minimum central thickness (offset) of the ConforMIS iForma™ implant can be reliably calculated solely on the basis of the specific algorithm of the ConforMIS 3-D sizing tool by means of the MRI-derived thickness of the cartilage in the arthritic knee compartment, thus providing a means for correcting the leg axis. Based on our data the amount of correction can approximately be determined following the linear regression formula: -0.0529 + (1.139 × offset) (p > 0.001).
Conclusion
The planning procedure for the ConforMIS iForma™ knee implant was shown to be reproducible and reliable. Despite the ongoing clinical trials with encouraging early results for this implant [11], long-term results are essential to evaluate the relevance of the iForma™ interpositional device compared to HTO and unicondylar knee replacement.
Acknowledgments
Conflict of interest statement The authors did not receive grants or outside funding in support of their research for or preparation of this manuscript. They did not receive payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, educational institution, or other charitable or nonprofit organisation with which the authors are affiliated or associated.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, University of Regensburg, Germany.
References
- 1.Aglietti P, Buzzi R, Vena LM, Baldini A, Mondaini A. High tibial valgus osteotomy for medial gonarthrosis: a 10- to 21-year study. J Knee Surg. 2003;16:21–26. [PubMed] [Google Scholar]
- 2.Campbell WC. Interposition of vitalium plates in arthroplasties of the knee: preliminary report. Am J Surg. 1940;47:639–641. doi: 10.1016/S0002-9610(40)90176-3. [DOI] [Google Scholar]
- 3.Coventry MB. Upper tibial osteotomy for gonarthrosis. The evolution of the operation in the last 18 years and long term results. Orthop Clin North Am. 1979;10:191–210. [PubMed] [Google Scholar]
- 4.Deshmukh RV, Scott RD. Unicompartmental knee arthroplasty: long-term results. Clin Orthop. 2001;392:272–278. doi: 10.1097/00003086-200111000-00035. [DOI] [PubMed] [Google Scholar]
- 5.Griffin T, Rowden N, Morgan D, Atkinson R, Woodruff P, Maddern G. Unicompartmental knee arthroplasty for the treatment of unicompartmental osteoarthritis: a systematic study. ANZ J Surg. 2007;77:214–221. doi: 10.1111/j.1445-2197.2007.04021.x. [DOI] [PubMed] [Google Scholar]
- 6.Hallock RH, Fell BM. Unicompartmental tibial hemiarthroplasty: early results of the UniSpacer knee. Clin Orthop Relat Res. 2003;416:154–163. doi: 10.1097/01.blo.0000093031.56370.90. [DOI] [PubMed] [Google Scholar]
- 7.Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69:332–354. [PubMed] [Google Scholar]
- 8.Hsu RWW, Himeno S, Coventry MB, Chao EYS. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed] [Google Scholar]
- 9.Insall JN, Joseph DM, Msika C. High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Joint Surg Am. 1984;66:1040–1048. [PubMed] [Google Scholar]
- 10.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koeck FX, Linhardt O, Perlick L, Anders S, Grifka J (2006) First experience with ConforMIS knee interpositional device. Presented at 52nd Annual Meeting of the Orthopaedic Research Society, Chicago, IL, 18–22 March 2006
- 12.Kolmogorov AN. Grundbegriffe der Wahrscheinlichkeitsrechnung. Berlin: Springer; 1933. [Google Scholar]
- 13.Laskin RS. Unicompartmental knee replacement: some unanswered questions. Clin Orthop Relat Res. 2001;392:267–271. doi: 10.1097/00003086-200111000-00034. [DOI] [PubMed] [Google Scholar]
- 14.Lienert GA. Testaufbau und Testanalyse. Weinheim: Beltz; 1969. [Google Scholar]
- 15.MacIntosh DL. Hemiarthroplasty of the knee using a space occupying prosthesis for painful varus and valgus deformities. In: Proceedings of the Joint Meeting of the Orthopaedic Associations of the English-Speaking World. J Bone Joint Surg Am. 1958;40:1431. [Google Scholar]
- 16.McKeever DC. Tibial plateau prosthesis. Clin Orthop Relat Res. 1960;18:86–95. doi: 10.1097/01.blo.0000187336.17627.ea. [DOI] [PubMed] [Google Scholar]
- 17.Miller M, Benjamin JB, Marson B, Hollstien S. The effect of implant constraint on results of conversion of unicompartmental knee arthroplasty to total knee arthroplasty. Orthopedics. 2002;25:1353–1357. doi: 10.3928/0147-7447-20021201-12. [DOI] [PubMed] [Google Scholar]
- 18.Paley D. Principles of deformity correction. Berlin: Springer; 2002. [Google Scholar]
- 19.Parvizi J, Hanssen AD, Spangehl MJ. Total knee arthroplasty following proximal tibial osteotomy: risk factors for failure. J Bone Joint Surg Am. 2004;86:474–479. doi: 10.2106/00004623-200403000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Perlick L, Baethis H, Tingart M, Perlick C, Luering C, Grifka J. Minimally invasive unicompartmental knee replacement with a nonimage-based navigation system. Int Orthop. 2004;28:193–197. doi: 10.1007/s00264-004-0549-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scott RD, Deshmukh R. Metallic hemiarthroplasty of the knee. Curr Opin Orthop. 2005;16:35–37. doi: 10.1097/01.bco.0000152814.36045.66. [DOI] [Google Scholar]
- 22.Sisto DJ, Mitchell IL. UniSpacer arthroplasty of the knee. J Bone Joint Surg Am. 2005;87:1706–1711. doi: 10.2106/JBJS.D.02339. [DOI] [PubMed] [Google Scholar]
- 23.Springer BD, Scott RD, Thornhill TS. Conversion of failed unicompartmental knee arthroplasty to TKA. Clin Orthop Relat Res. 2006;446:214–220. doi: 10.1097/01.blo.0000214431.19033.fa. [DOI] [PubMed] [Google Scholar]
- 24.Strecker W. Planning analysis of knee-adjacent deformities. Oper Orthop Traumatol. 2006;18:259–272. doi: 10.1007/s00064-006-1175-1. [DOI] [PubMed] [Google Scholar]
- 25.Whiteside LA. Making your next unicompartmental knee arthroplasty last: three keys to success. J Arthroplasty. 2005;20(4 Suppl 2):2–3. doi: 10.1016/j.arth.2005.03.029. [DOI] [PubMed] [Google Scholar]