Abstract
The purpose of this study was twofold: to evaluate the radiological and clinical results of 33 total knee arthroplasties (TKA) implanted between January 1993 and March 2005, to replace failed medial unicompartmental knee arthroplasty (UKA), and to develop a strategy to deal with bone defects in the tibial plateau. Failure was due to: tibial loosening (15 cases), femoral loosening (five cases), femoral and tibial loosening (two cases), polyethylene wear (five cases), lateral compartment osteoarthritis (two cases), patellofemoral osteoarthritis (two cases), laxity and PE dislocation (one case), and sepsis in one case. In 12 cases the tibial bone defect was filled with a metallic wedge, in seven we used an allograft (femoral head), and in one we used both. We report the results of 27 cases (five patients died and one was lost to follow-up). The mean follow-up was 73±41.7 months (range, 8–153) and the global IKS score was 166.72±21.3 points (range, 128–200). X-rays of the eight allografts showed osteointegration in all cases and no radiolucency was noted.
Résumé
Le propos de cette étude a deux objets, d’une part d’évaluer les résultats de 33 prothèses totales du genou, réalisées entre janvier 1993 et mars 2005, mises en place pour échec de prothèses uni-compartimentales, deuxièmement de développer une stratégie permettant de compenser les défects osseux des plateaux tibiaux. L’échec de ces prothèses était dû à un descellement tibial (15 cas), fémoral (5 cas), fémoral et tibial (2 cas), d’usure du polyéthylène (5 cas), d’arthrose du compartiment contro-latéral externe (2 cas), d’arthrose fémoro-patellaire (2 cas), un cas de laxité avec dislocation prothétique (1 cas), enfin un cas de sepsis. Dans 12 cas le défect tibial osseux a été compensé par une cale métallique et dans 7 cas nous avons utilisé une allogreffe de tête fémorale. Enfin dans un cas nous avons utilisé à la fois une cale et une greffe. Nous rapportons les résultats de 27 cas, 5 patients étant décédés et un perdu de vue. Le suivi moyen a été de 73+/- 41,7 mois, (8 à 153 mois), le score IKS global de 166,72,+/- 21,3 points (128 à 200). Les résultats radiographiques ont montré pour les 8 allogreffes qu’elles avaient été ostéointégrées sans liseré.
Introduction
Unicompartmental knee arthroplasty (UKA) is one of the main treatment alternatives for tibiofemoral osteoarthritis. The advantages of this implant include a faster and better functional recovery than total knee arthroplasty [15, 26] and less morbidity due, for the main part, to minimal postoperative blood loss. In addition, it seems logical to replace only the damaged compartment of the knee. Nowadays, the indications, contraindications, and surgical techniques for UKA seem well-codified [2, 11, 19], and failure to comply with these guidelines results in early wear and loosening [1, 11–13, 22].
Despite these facts, there remains an inevitable failure rate due to polyethylene (PE) wear [3, 6, 17], loosening, and extended osteoarthritis. The usual mechanisms of failure include misalignment [8], bad indications [24], weakness of the implant or faulty manufacture [18], difficulties with implant extraction, bone defect management, and the implant to be used.
The purpose of this study was to present the radiological and clinical results of 33 revisions from medial UKA to total knee arthroplasty (TKA) and compare them to those of the literature. A technical strategy for the revisions is also presented, especially for dealing with tibial bone defects (Fig. 1).
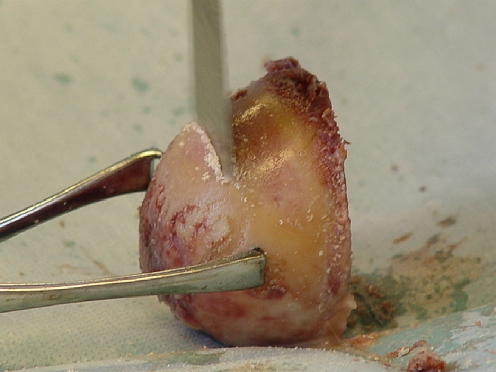
Fig. 1.
Severe bone loss at the level of the tibial plateau
Material and methods
Our series included 33 patients, treated in our department (mostly by the senior author, 31 out of 33) between January 1993 and March 2005, with 16 right and 17 left knees, on 23 female and ten male patients. The mean age was 71.76±8.5 years (range, 49–93), the mean weight was 71.12±12.78 kg (range, 52–95), and the mean BMI was 27±4 kg/m2 (range, 21.67–34.24). Sixteen (48.5%) had their UKA implanted in our department, whereas the other 17 (51.5%) had it implanted elsewhere. Their mean age for UKA was 66.9±7.7 years (range, 44–80), and the mean survival of the UKA was 58.2±43 months (range, 5–180).
The mean IKS (International Knee Society) scores at the time of the revision were 43±14.66 points (range, 0–70) for function score, 57±13.62 points (range, 0–70) for knee score, and 99±23.76 points (range, 0–130) for global score.
Failure was evident on plain X-rays in 22 cases, and a technetium 99 bone scan was used in 11 cases to confirm loosening. These were positive in all cases with increased uptake under the tibial plateau in six patients and under both the tibia and femur in the remaining five.
Indications for the initial UKA were medial compartment osteoarthritis (MCOA) in 26, medial femoral condyle osteonecrosis in six, and MCOA following knee dislocation in one. The implants used in these initial procedures included: the Search Uni (B-Braun-Aesculap, Germany) in nine cases, the mobile bearing Oxford (Biomet, USA) in nine cases, and the Miller-Gallante (Zimmer, USA) in four cases, with other designs for the rest.
Reasons for failure were as follows. Early failures (less than five years) included nine from tibial loosening, three femoral loosening, two patellofemoral osteoarthritis, two PE dislocations on Oxford prosthesis, and one sepsis (history of operated knee dislocation). Intermediate failures (five to ten years) included seven from tibial loosening, three PE fractures, two cases of extension of the osteoarthritis, and one bipolar (tibial and femoral) loosening. Late failures (over ten years) included two cases of PE wear and one tibial and femoral loosening.
Our strategy for dealing with these revisions was that all failed UKA were replaced by TKA. We used the PCL retaining Search LC (B-Braun-Aesculap) in 14 cases, the posterior stabilised Search PS (B-Braun-Aesculap) in 17 cases, the Maxim prosthesis (Biomet) in one case, and the varus valgus constraint Dual Articular prosthesis (Biomet) in one case. We added a long tibial stem in 18 cases and a femoral stem in two cases. In one of the patients we had to perform an osteotomy of the tibial tuberosity to avoid damaging the patellar ligament.
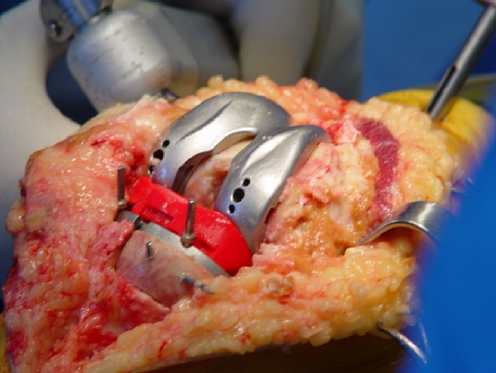
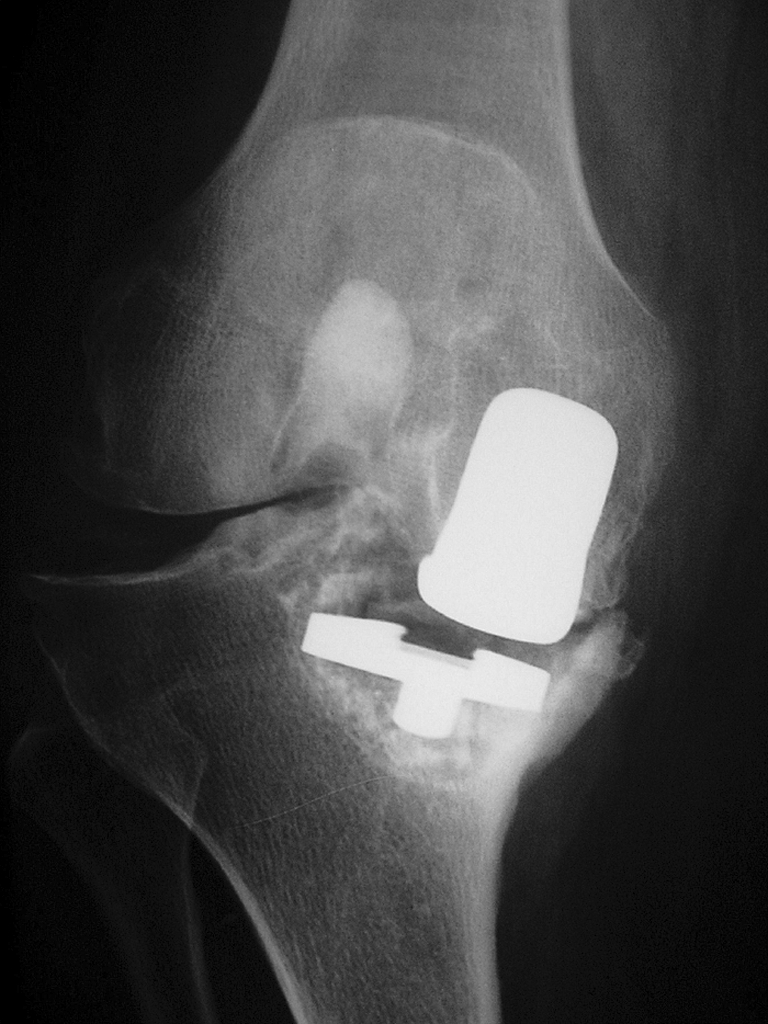
We had to fill a bone defect in two femurs (6%) and 20 tibial plateaux (60.6%). These defects were filled with morselised bone graft in the femur (cavitary defect) and with metal wedges and/or allograft in the tibia (Figs. 2, 3, 4, 5, 6). In cases of moderate segmental defects (less than 8 mm of defect underneath the resection level of the intact tibial plateau), we used metal wedges; this was the case in 12 revisions (two wedges of 4 mm, three of 6 mm, and seven of 8 mm). In cases of severe bone defect (more than 8 mm of defect underneath the resection level of the intact tibial plateau), we used either frozen femoral head allograft (seven cases) or a metal wedge plus frozen femoral head (one case). A long tibial stem was used in all the cases with allografts, and in ten out of 12 cases with metal wedges.
Fig. 2.
Step resection of the medial tibial plateau
Fig. 3.
Preparation of the femoral head for bone grafting
Fig. 4.
Temporary fixation of the bone graft in its proper position using Kirschner wires
Fig. 5.
Placing the trial prosthesis on top of the reconstructed tibial plateau
Fig. 6.
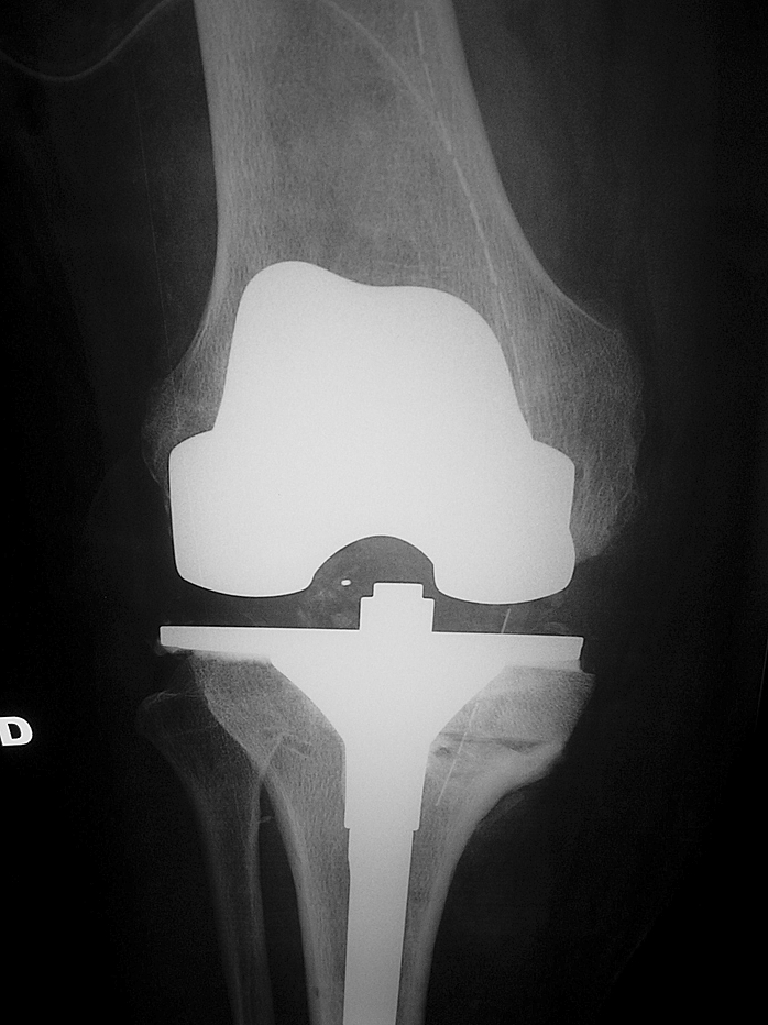
Postoperative X-ray to check the prosthesis and the bone graft
Most of the patients (n = 23) were reviewed, clinically and radiologically, by an independent observer. Others (n = 4) responded via phone calls and sent us their X-rays by mail. Added functional disabilities were classified according to Charnley’s categories (A, B, C). We used the IKS score to evaluate the functional results. The radiological results were evaluated using weight bearing AP and lateral views as well as skyline views. Besides evident loosening, we screened for radiolucencies, PE wear, and osteointegration or lysis of the allograft. Alignment was evaluated on weight bearing X-rays taken three months postoperatively. These long-leg X-rays were not renewed for the revision.
Results
We did not note any early complications, whether local or general. One patient underwent mobilisation under general anaesthesia for a limited flexion (70°) at two months. This patient had undergone four procedures on his knee, and we were able to restore 110° of flexion. Concerning late complications, two underwent revisions for tibial loosening and two for patellar loosening.
We report the results of 27 patients (five died and one was lost to follow-up) with a mean follow-up of 73±41.7 months (range, 8–153). For functional results, the mean knee score was 86.3±10.6 points (range, 63–100), the mean function score was 80.4±16 points (range, 40–100), and the global score was 166.72±21.3 points (range, 128–200). The mean flexion was 103.8°±19.2° (range, 45–130), including 13 patients between 110° and 130°, 11 between 90° and 110°, two between 75° and 90°, and one below 75°. No significant extension lag was noted. These results varied with the defect to be filled; patients with bone defects that did not require any filling had a mean global score of 155.25±22.8 points (range, 128–190). Those with defects that required filling with either allografts or metal wedges had a mean score of 172.66±18.47 points (range, 135–200). Charnley’s categories were used at revision: 54.5% were classified A, 39.39% B, and 6.02% C. For radiological results, the mean HKA was 179.6°±3° (range, 174°–185°) including 24 patients (88.9%) with an HKA of 180°±3°. We found only one incomplete radiolucency in zone 2 of the femur. We also found incomplete radiolucencies around the tibia on AP views with four in zones 1–2, three in zones 3–4, and two in zone 5; on lateral views, seven were in zone 1 and three in zone 2. In the latter eight radiolucencies, two seemed progressive. In addition, one tibial plateau was definitely loose and generated pain, which significantly affected the knee score. We also found evidence of PE wear in four knees: two on the medial side of the prosthesis (of 1 and 2 mm) and two on the lateral side of the prosthesis (both of 2 mm). We had osteointegration of all eight femoral head allografts and no radiological signs of osteolysis at 8–96 months of follow-up.
Discussion
We agree with other authors [8], that revision from medial UKA to TKA is a relatively simple procedure if planned thoroughly. This planning should take into consideration the possible difficulties with implant extraction and the bone defects that this might cause, as well as ligamentous balance which must be restored or eventually compensated by using a constrained prosthesis. A standard prosthesis should be made available, postero-stabilised or not, as was used in 13 cases of our series, or better, a prosthesis allowing addition of long tibial stems (used 18 times in our series) and also metal wedges to fill bone defects which are most frequently located under the tibial plateau (60.6% of cases). Allografts should also be made available (we prefer frozen femoral heads) because metal wedges are usually smaller than 8 mm and do not allow filling of big segmental defects (>8 mm below the resection level of the intact tibial plateau). Allografts also reconstitute bone stock around the prosthesis which is very useful in cases of re-revision (Fig. 6).
The results are globally satisfactory (global IKS score of 166.72±21.3 points) and comparable to other series in the literature [8, 10, 16, 17, 20, 21] where the global IKS score varied between 135 and 172 points (Table 1).
Table 1.
Comparative results of UKA revisions
Numerous other authors [3, 4, 7, 10, 16, 17, 24] stress the importance of bone defects in the tibia with rates varying from 33–77% (Table 2). Materials used to fill the defects varied among the authors. These included cement, metal wedges, autografts, allografts, and screws (Table 2). Evaluating bone defects also varied among authors, whereby some used the volume [7, 8] and others the thickness. We did not use either of these methods but chose Engh and Ammeen’s method [9] for classification of bone defects according to type. We thus differentiated cavitary defects filled with morselised bone chips or cement from segmental defects which, as stated above, were filled with either metal wedges or allografts. This evaluation was made after resection of the intact tibial plateau with two scenarios: either the cortex under the extracted implant is intact with defects in the cancellous bed (cavitary defects) or it is damaged (segmental defects requiring more extensive resection under the extracted implant and thus creating a step below the intact plateau). Considering that this more extensive resection is performed in an area with low mechanical resistance, it is safer to fill this defect with a metal wedge or a structural allograft than to rely solely on a long stem to avoid tilting of the implant by progressive sinking of the medial plateau. In our series, results were better in the group with bone defects (172.66±18.47 points) than in the group without defects (155.25±22.8 points). But it is hazardous to jump to conclusions because the series were not comparable. In fact, in the latter series, we found one tibial loosening, patellar complication, and one supracondylar fracture that occurred several years after the revision.
Table 2.
Bone defects and methods of reconstruction
| Number of cases with tibial bone loss | Management of bone loss | |
|---|---|---|
| Barrett and Scott (1987) [3] | 33% | Graft, cement and screws, metallic wedge |
| Padgett et al. (1991) [24] | 76% | Cement, autograft |
| Lai and Rand (1993) [16] | 50% | Cement |
| Gill et al. (1995) [10] | 77% | Autograft, allograft, metallic wedge |
| Levine et al. (1996) [17] | 33% | Allograft |
| Chakrabarty et al. (1998) [7] | 60% | Autograft, cement |
| Böhm and Landsiedl (2000) [4] | 39% | Autograft |
| Our series (2005) | 60% segmental | Metallic wedge, allograft, autograft |
It seemed important for us to compare the results of UKA revisions with those of high tibial osteotomy (HTO) revisions. Although it was difficult to compare different series, it seems that HTO revisions were equivalent to UKA revisions [14, 25], even superior for Gill et al. [10]; however, Jackson et al. [14] found a higher rate of complications (30% more) following HTO revisions. Each revision has its own set of problems: tibial bone defects for UKA revisions; difficulties in patellar dislocation with resultant extensor mechanism lesions and difficulties with ligamentous balance leading sometimes to de-osteotomy-prosthesis [23] or to using constraint prosthesis in HTO revisions. The results in TKA revisions are worse than those of UKA revisions as shown by Bonnin et al. [5] because bone defects were both femoral, tibial, and sometimes patellar, accounting for difficulties in reconstruction and in finding the appropriate joint line level.
Conclusion
Changing UKA to TKA gives good results, similar to those of HTO revisions and better than those of TKA revisions. The major problem is managing tibial bone defects which we found in 60.6% of the cases. This can be perfectly controlled by using metal wedges and femoral head allografts, while avoiding the use of constraint prostheses. Proper indications and a rigorous surgical technique should give UKA similar survival rates to that of TKA and decrease the rate of revisions.
References
- 1.Argenson JN, Komistek RD, Aubaniac JM, Dennis DA, Northcut EJ, Anderson T, Agostini S. In vivo determination of knee kinematics for subjects implanted with a unicompartmental knee arthroplasty. J Arthroplasty. 2002;17:1049–1054. doi: 10.1054/arth.2002.34527. [DOI] [PubMed] [Google Scholar]
- 2.Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM. Modern unicompartmental knee arthroplasty with cement: a three to ten year follow-up study. J Bone Joint Surg Am. 2002;84:2235–2239. [PubMed] [Google Scholar]
- 3.Barrett WP, Scott RD. Revision of failed unicondylar knee arthroplasty. J Bone Joint Surg Am. 1987;69:1328–1335. [PubMed] [Google Scholar]
- 4.Böhm I, Landsiedl F. Revision surgery after failed unicompartmental knee arthroplasty: a study of 35 cases. J Arthroplasty. 2000;15:982–989. doi: 10.1054/arth.2000.9841. [DOI] [PubMed] [Google Scholar]
- 5.Bonnin M, Deschamps G, Neyret P, Chambat P. Revision in non-infected total knee arthroplasty: an analysis of 69 consecutive cases. Rev Chir Orthop. 2000;86:694–706. [PubMed] [Google Scholar]
- 6.Cameron HU, Jung YB. Clinical results with an uncemented plastic tibial component in unicompartmental knee replacement. Can J Surg. 1988;31:256–258. [PubMed] [Google Scholar]
- 7.Chakrabarty G, Newman JH, Ackroyd CE. Revision of unicompartmental arthroplasty of the knee: clinical and technical considerations. J Arthroplasty. 1998;13:191–196. doi: 10.1016/S0883-5403(98)90098-5. [DOI] [PubMed] [Google Scholar]
- 8.Chatain F, Richard A, Deschamps G, Chambat P, Neyret P. Revision total knee arthroplasty after unicompartmental femorotibial prosthesis: 54 cases. Rev Chir Orthop. 2004;90:49–54. doi: 10.1016/s0035-1040(04)70006-9. [DOI] [PubMed] [Google Scholar]
- 9.Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999;48:167–175. [PubMed] [Google Scholar]
- 10.Gill T, Schemitsch EH, Brick GW, Thornhill TS. Revision total knee arthroplasty after failed unicompartmental knee arthroplasty or high tibial osteotomy. Clin Orthop Relat Res. 1995;321:10–18. [PubMed] [Google Scholar]
- 11.Hernigou P, Deschamps G. Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2004;423:161–164. doi: 10.1097/01.blo.0000128285.90459.12. [DOI] [PubMed] [Google Scholar]
- 12.Hernigou P, Deschamps G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am. 2004;86:506–511. doi: 10.2106/00004623-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Iorio R, Healy WL. Unicompartmental arthritis of the knee. J Bone Joint Surg Am. 2003;85:1351–1364. doi: 10.2106/00004623-200307000-00025. [DOI] [PubMed] [Google Scholar]
- 14.Jackson M, Sarangi PP, Newman JH. Revision total knee arthroplasty: comparison of outcome following primary proximal tibial osteotomy or unicompartmental arthroplasty. J Arthroplasty. 1994;9:539–542. doi: 10.1016/0883-5403(94)90102-3. [DOI] [PubMed] [Google Scholar]
- 15.Kozinn SC, Scott RD. Surgical treatment of unicompartmental degenerative arthritis of the knee. Rheum Dis Clin North Am. 1988;14:545–564. [PubMed] [Google Scholar]
- 16.Lai CH, Rand JA. Revision of failed unicompartmental total knee arthroplasty. Clin Orthop Relat Res. 1993;287:193–201. [PubMed] [Google Scholar]
- 17.Levine WN, Ozuna RM, Scott RD, Thornhill Conversion of failed modern unicompartmental arthroplasty to total knee arthroplasty. J Arthroplasty. 1996;11:797–801. doi: 10.1016/S0883-5403(96)80179-3. [DOI] [PubMed] [Google Scholar]
- 18.Lindstrand A, Stenstrom A, Lewold S. Multicenter study of unicompartmental knee revision. PCA, Marmor, and St Georg compared in 3777 cases of arthrosis. Acta Orthop Scand. 1992;63:256–259. doi: 10.3109/17453679209154777. [DOI] [PubMed] [Google Scholar]
- 19.Marmor L. Unicompartmental knee arthroplasty. Ten to 13 year follow up study. Clin Orthop Relat Res. 1988;226:14–20. [PubMed] [Google Scholar]
- 20.McAuley JP, Engh GA, Ammeen DJ. Revision of failed unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2001;392:279–282. doi: 10.1097/00003086-200111000-00036. [DOI] [PubMed] [Google Scholar]
- 21.Miller M, Benjamin JB, Marson B, Hollstein S. The effect of implant constraint on results of conversion of unicompartmental knee arthroplasty to total knee arthroplasty. Orthopaedics. 2002;25:1353–1357. doi: 10.3928/0147-7447-20021201-12. [DOI] [PubMed] [Google Scholar]
- 22.Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br. 1998;80:983–989. doi: 10.1302/0301-620X.80B6.8177. [DOI] [PubMed] [Google Scholar]
- 23.Neyret P, Deroche P, Deschamps G, Dejour H. Total knee replacement after valgus tibial osteotomy: technical problems. Rev Chir Orthop. 1992;78:438–448. [PubMed] [Google Scholar]
- 24.Padgett DE, Stern SH, Insall JN. Revision total knee arthroplasty for failed unicompartmental replacement. J Bone Joint Surg Am. 1991;73:186–190. [PubMed] [Google Scholar]
- 25.Parvizi J, Hanssen AD, Spangehl MJ. Total knee arthroplasty following proximal tibial osteotomy: risk factors for failure. J Bone Joint Surg Am. 2004;86:474–479. doi: 10.2106/00004623-200403000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Rougraff BT, Heck DA, Gibson AE. A comparison of tricompartmental and unicompartmental arthroplasty for the treatment of gonarthrosis. Clin Orthop. 1991;273:157–164. [PubMed] [Google Scholar]