Abstract
The aim of this study was to detect the accuracy of routine magnetic resonance imaging (MRI) done in different centres and its agreement with arthroscopy in meniscal and ligamentous injuries of the knee. We prospectively examined 70 patients ranging in age between 22 and 59 years. History taking, plain X-ray, clinical examination, routine MRI and arthroscopy were done for all patients. Sensitivity, specificity, accuracy, positive and negative predictive values, P value and kappa agreement measures were calculated. We found a sensitivity of 47 and 100%, specificity of 95 and 75% and accuracy of 73 and 78.5%, respectively, for the medial and lateral meniscus. A sensitivity of 77.8%, specificity of 100% and accuracy of 94% was noted for the anterior cruciate ligament (ACL). We found good kappa agreements (0.43 and 0.45) for both menisci and excellent agreement (0.84) for the ACL. MRI shows high accuracy and should be used as the primary diagnostic tool for selection of candidates for arthroscopy. Level of evidence: 4.
Résumé
Le but de cette étude est de détecter un examen de routine l’IRM et la bonne correspondance entre ces constatations et les constatations arthroscopiques des lésions méniscales ou des lésions ligamentaires du genou. Nous avons réalisé une étude prospective de 70 patients âgés de 22 à 59 ans avec analyse de l’histoire clinique, des radiographies, de l’examen clinique, de l’examen IRM et des constatations arthroscopiques. La sensitivité, la spécificité et l’exactitude des constatations ont été évaluées de manière statistique. Nous avons trouvé respectivement une sensitivité de 47% et 100%, une spécificité de 95% et 75% et une exactitude des constatations de 73% et 78,5%, pour les lésions du ménisque interne ou du ménisque latéral. En ce qui concerne les ligaments croisés, la sensitivité est de 77,8%, la spécificité de 100% et l’exactitude des constatations de 94% avec une bonne correspondance Kappa (0,43 et 0,45) pour les ménisques et 0,84 pour le ligament croisé antérieur. L’IRM peut donc être utilisée comme un élément tout à fait sûr et routinier concernant le diagnostic primaire des lésions miniscales ou des lésions ligamentaires chez les patients devant bénéficier d’une arthroscopie. Niveau d’évidence : 4.
Introduction
Magnetic resonance imaging (MRI) has an enormous impact on musculoskeletal imaging and the knee is the most frequently visualised. MRI of the knee is most commonly indicated in patients with suspected injuries of the menisci and cruciate ligaments. Plain radiographs have little value unless injury is due to direct impact [10].
Orthopaedic surgeons commonly examine patients with knee pain; however, precisely diagnosing an intra-articular cause of pain is difficult. MRI of the knee is used to diagnose disorders of the knee because the high soft tissue resolution allows precise imaging of intra-articular structures [3].
MRI of the menisci has proven useful for more than 10 years, with current sensitivity and specificity for meniscal tears ranging from 90 to 95% in most reports [1]. MRI has become a practical tool for the evaluation of anterior cruciate ligament (ACL) injuries, with its high levels of accuracy and sensitivity reported in the literature [15].
Previous imaging provided an accuracy of 90% for the medial meniscus, 82% for the lateral meniscus, 94% for the ACL and 96% for the posterior cruciate ligament. The sensitivity was 87% for the medial meniscus, 46% for the lateral meniscus, 92% for the ACL and 80% for the posterior cruciate ligament. The specificity was relatively high at 92, 91, 94 and 97%, respectively [17].
Intra-articular knee lesions are associated with significant morbidity and frequently need surgical treatment and rest. Although common, their correct diagnosis still is a challenge. Clinical tests may be confusing, and delay in diagnosis can result in socioeconomic problems and sometimes a worse prognosis. Therefore, complementary diagnostic tools are often necessary, mainly when suspecting multiple lesions [13].
The aim of this prospective study was to determine the accuracy of routine MRI study done in different centres in detecting meniscal and ligamentous injuries in comparison with arthroscopy as the gold standard.
Material and method
Patient population
We examined 70 patients ranging in age between 22 and 59 years (41 men and 29 women). Patients experienced pain, popping, locking, instability and swelling.
History taking, plain X-ray and clinical examination included presence of effusion, range of motion, joint line tenderness, three plane stability as well as the McMurray, squat, Apley, anterior drawer, Lachmann, posterior drawer and quadriceps active tests.
Patients with joint disease, e.g. rheumatoid arthritis or previous knee operations, were excluded.
All patients were subjected to MRI and arthroscopy. The study was approved by the Ethics Committee of Cairo University.
MRI protocol
Due to the economic burden of MRI, we could not force patients to go to a single radiology centre nor did we want to. Most of them were sent to centres of their own choice taking into consideration that all centres had a 0.5-T MRI machine (commonly available in Egypt). The standard imaging protocol was sagittal spin echo T1-weighted images (T1WIs) [repetition time (TR): 500, echo time (TE): 22], T2-weighted images (T2WIs) (TR: 3600, TR: 100) and proton density images (TR: 2200, TE: 17), coronal short τ inversion recovery (STIR) (TR: 2300, TE: 60) and axial T2WIs (TR: 3600, TR: 100). We used 4- mm slice thickness with 0.5-mm interslice gap and 18 × 18 cm field of view (FOV) with a 256 × 512 or 192 × 256 imaging matrix. No contrast media were given.
The MRI findings were reviewed by two radiologists. Meniscal and ligamentous injuries were evaluated and graded. Absence of an intrameniscal high signal was considered as a normal meniscus. Presence of an intrameniscal high signal not extending to the articular surface was considered grade 1 and 2 degeneration of the menisci, while intrameniscal high signal intensity reaching the articular surface was regarded as a tear.
The ACL was considered normal when it appeared as a band of fibres of low or intermediate signal intensity on both sagittal and coronal images. It was considered partially torn when it appeared fuzzy with ill-defined outline and abnormal signal intensity within, and as completely torn if there was disruption of all fibres, discontinuity or avulsion from its attachment.
Arthroscopy
The surgeons were aware of the MRI results, as we thought it was better to emphasise MRI findings to decrease the time needed to revise the videotapes in cases of contradictory results.
Arthroscopies were done in a hospital environment with complete preoperative care, all in the outpatient surgery. A Stryker 3 CCD video camera was used with a 4-mm Karl Storz arthroscope and a 30° angle. Standard portals were used: superomedial portal for outflow, inferolateral for the arthroscope and inferomedial for instrumentation. During arthroscopy, a systematic examination was performed with a complete evaluation of the joint. Arthroscopies were done within 2 months of MRI after the patients had provided signed consent.
Menisci were considered degenerated when fibrillation was present and trimming was done. A meniscal tear was diagnosed when there was discontinuity of its cartilage and the surgeon proceeded to partial meniscectomy according to the size and shape of the tear.
A complete tear of the ACL was diagnosed if the ligament was absent in the notch region, or if there was loss of ligament continuity with only ligament remnants at each end and the surgeon proceeded directly to reconstructive surgery in the same setting. In cases where continuity of one or both bundles for the ligament was present and laxity of the ligament was noted by probing, this was defined as a partial tear.
Statistical analysis
Structures included in the study were medial and lateral menisci and anterior and posterior cruciate ligaments. We considered meniscal tear and degeneration as one group compared against the normal menisci. We studied the ACL twice; once we considered the complete and partially torn ACLs as one group compared against the normal and the other time we studied the complete tear as one group compared against the normal and partially torn ACLs.
Data were coded and entered using the Statistical Package for the Social Sciences (SPSS) version 12. Data were summarised using percent for qualitative data. Comparisons between qualitative variables were done using the chi-square test. P values < 0.05 were considered as statistically significant. Sensitivity, specificity, positive and negative predictive values, accuracy, P value and kappa agreement measures were calculated to test validity of MRI compared against arthroscopy.
Results
The study included 70 patients ranging in age between 22 and 59 years (41 men and 29 women). All were subjected to examination, X-ray, MRI study and arthroscopy (Figs. 1, 2, 3, 4 and 5).
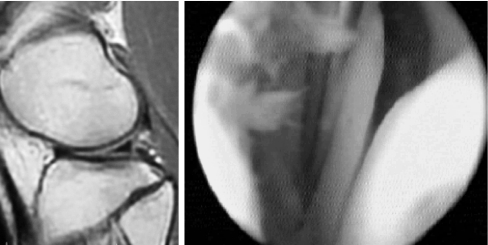
Fig. 1.
Sagittal MRI showed normal lateral meniscus while arthroscopy detected a lateral meniscal tear (tool is seen within the tear)
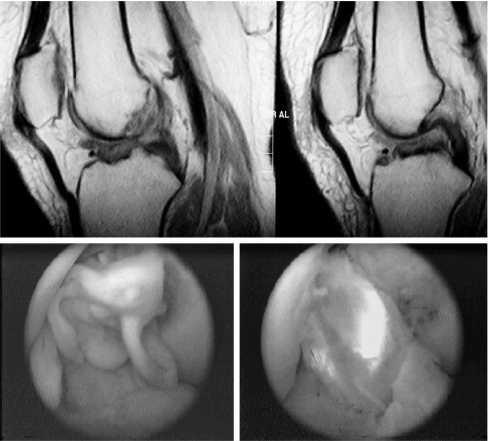
Fig. 2.
MRI diagnosed complete ACL tear, arthroscopy confirmed the diagnosis showing buckling of the ACL with detached femoral attachment and reconstruction was performed
Fig. 3.
MRI showed degeneration of the posterior horn of the medial meniscus, while arthroscopy showed a normal medial meniscus
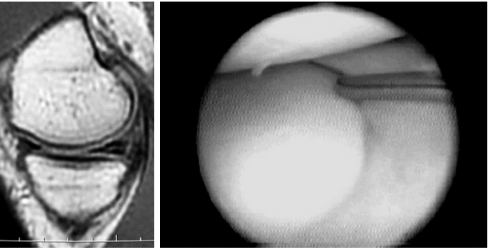
Fig. 4.
MRI diagnosed a partial tear of the ACL; however, arthroscopy showed a normal ACL
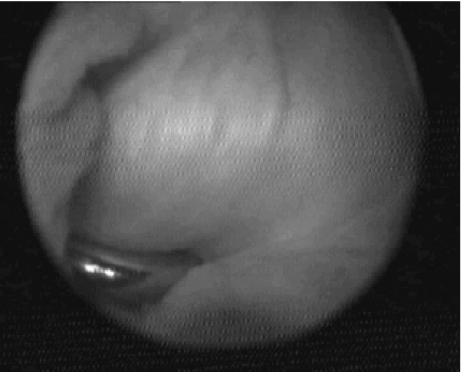
Fig. 5.
MRI showed posterior horn medial meniscal tear which was confirmed by arthroscopy
We diagnosed 36 cases of medial meniscal tear (mostly posterior horn), 17 cases of meniscal degeneration and 17 normal medial menisci by MRI. Arthroscopy diagnosed 28 cases of meniscal tear, 10 cases of degeneration and 32 normal menisci.
Of 36 meniscal tears diagnosed by MRI only 22 (61%) were confirmed by arthroscopy: 2 (5.6%) were degeneration and 12 (33%) were found to be normal menisci.
Of the 17 diagnosed as meniscal degeneration, arthroscopy diagnosed 8 as degeneration, 4 as tears and 5 as normal menisci. Of the 17 diagnosed as normal menisci by MRI, 15 were confirmed by arthroscopy while 2 were diagnosed as meniscal tears. Two of the tears were bucket handle based on arthroscopy while MRI only detected one.
Regarding the lateral meniscus MRI diagnosed only 4 tears and 6 degenerations with 60 normal menisci. However, arthroscopy diagnosed 13 tears, 12 degenerations and 45 normal menisci. Of the four diagnosed as a tear by MRI, two were confirmed as a tear and two as degeneration by arthroscopy. Of the six diagnosed as degeneration, four were confirmed by arthroscopy while two were considered tears. Seventy-five per cent of the cases found to be normal by MRI were also normal according to arthroscopy while 10% showed degeneration and 15% showed meniscal tears.
MRI detected 18 complete ACL tears, 8 partial tears and 44 normal ACL. Arthroscopy detected 14 complete tears, 10 partial tears and 46 normal ACL. Seventy-eight per cent of the complete tears diagnosed by MRI were also considered complete tears by arthroscopy while the rest (22%) were partial tears. Fifty per cent of the partial tears diagnosed by MRI were confirmed by arthroscopy while the other 50% were found to be normal.
We performed statistical analysis of the ACL two times, once with both partial and complete tears as one group compared against the normal and the other time with only the complete tears compared against the partial and normal ACLs (the method used in most of the previous studies). We found that sensitivity, specificity, negative and positive predictive values and accuracy were higher when considering complete and partial tears as one group compared against the normal ligaments (Table 1).
Table 1.
Validity of MRI findings using arthroscopy as the gold standard reference
| Structure | Medial meniscus | Lateral meniscus | ACL complete tears against others (partial + normal) | Anterior cruciate ligament (partial + complete as one group against normal) |
|---|---|---|---|---|
| Accuracy (%) | 73 | 78.5 | 94 | 97 |
| Sensitivity (%) | 47 | 100 | 77.8 | 92.3 |
| Specificity (%) | 95 | 75 | 100 | 100 |
| Negative predictive value | 88.2 | 100 | 100 | 95 |
| Positive predictive value | 68 | 40 | 93 | 100 |
| Kappa agreement | 0.43 | 0.46 | 0.84 | 0.9 |
| P value | 0.0001 | 0.001 | 0.001 | 0.001 |
Arthroscopy revealed 34 (48.5%) cases with concomitant injury. The predominant pattern was meniscal (mainly posterior horn of the medial meniscus) with ACL tear (19 cases) followed by combined medial and lateral meniscal injuries (15 cases).
MRI detected 28 (40%) cases of concomitant injuries. The predominant pattern was medial meniscal injury and ACL tears (24 cases), while only 2 showed combined medial and lateral meniscal injuries. Two other cases showed lateral and medial meniscal injuries plus ACL tear. Isolated injury of the ACL was only detected in five cases by arthroscopy and in four cases by MRI.
None of our cases showed any pathological findings within the posterior cruciate ligament, neither by MRI nor arthroscopy, showing total agreement in their results.
Our study showed good kappa agreement (0.43 and 0.46) for the medial and lateral menisci, respectively, and excellent agreement (0.84 and 0.9) for the ACL between MRI findings compared against the gold standard arthroscopic findings (Table 1).
Discussion
Although intra-articular knee lesions are common, their correct diagnosis still is a challenge [13].
MRI of the knee has become a reliable tool in the detection of knee injuries. Injuries to menisci and cruciate ligaments can be diagnosed on MRI with a high degree of sensitivity and specificity, but accuracy of MRI decreases in patients with multiple injuries [12, 7].
We detected a sensitivity of 47% for the medial meniscus and accuracy of 73%, which are lower than most of those reported in the literature [3, 13, 8]. However, the specificity was 95% which was in agreement with previous studies [13, 8].
The lateral meniscus showed a higher sensitivity in our study than reported in most of the literature and slightly lower specificity [13, 8, 16].
The approach taken with an ACL injury depends a great deal on the severity of the lesion. Complete ACL tears usually cause considerable knee joint instability and reconstructive surgery is typically recommended. In contrast, a partial ACL tear can be treated with physical rehabilitation. Since reconstructive surgery involves significant remodelling, confirmation of the diagnosis is desirable before undertaking unnecessary surgery on patients with incomplete ACL tears. Arthroscopic examination allows the diagnosis to be confirmed through direct visualisation and probing. Unfortunately, arthroscopies are invasive and require a skilled surgeon. MRI has become a popular and practical tool for the evaluation of ACL injuries with its high degree of accuracy and sensitivity as reported in the literature [4].
Our results were similar to those of Patrice et al. [16] concerning the sensitivity and specificity of ACL tears when we considered normal and partially torn ligaments as one group and complete tears as another group like they did [16]. Our results improved when we studied the complete and partial tears as a group compared against the normal anterior cruciate ligaments.
Isolated ACL tears are rare; Barry et al. [2] reported an incidence of 13%. Only 2% of ACL tears were isolated in our study, the rest being associated with meniscal tears.
The results show that diagnostic performance and accuracy is better for cruciate ligament tears than for meniscal tears. Regarding the menisci, our results demonstrate that the sensitivity and specificity differ significantly for the medial and the lateral meniscus. Those findings were also reported by Oei et al. [11]. However, they stated that MRI is more sensitive in the diagnosis of the medial meniscus and that the specificity is higher for the lateral meniscus [11]. Our results were contradictory with a higher sensitivity for the lateral meniscus and a higher specificity for the medial meniscus.
In the study by De Smet and Graph [7] the sensitivity for meniscal injuries decreased markedly in cases associated with ACL tears. This may be the cause of the low sensitivity detected in medial meniscal tears in our study as most of the cases had associated ACL injuries. However, the sensitivity of the lateral meniscus was not affected since the majority of our cases did not have associated ACL tears.
There are several other factors that may contribute to the discrepancy found between arthroscopic findings and MRI reports. The interpretation of MRI may be influenced by imaging techniques and subjective bias of the reading radiologists [15].
Some authors reported that specific imaging sequences improve the sensitivity and specificity for detecting meniscal and ligamentous tears [9]. However, our study was concerned with the routine MRI technique done in different centres so we did not introduce specific sequences but only used those done as a routine study in these different centres.
Most of the studies were done in big hospitals or medical centres where both arthroscopy and MRI were done in the same place and reported by highly trained radiologists specialised in musculoskeletal imaging. This may contribute to the higher accuracy rates reported in these studies, especially in the menisci.
The value of our work is that we studied the accuracy of MRI and its agreement with arthroscopy as it is actually done in our country without using a specific imaging protocol. Due to the cost of MRI most people have insurance that sends them to a specific radiology centre; we only tried to select centres that have the same field strength machine (0.5 T) which is most commonly used.
Another advantage of this study is that it is a prospective study, while most of the previous studies were retrospective. We had the advantage of concentrating on the MRI findings during arthroscopy, hence omitting the need for reevaluating the videotapes and MRI results in cases of discrepancy.
We were concerned that the use of 0.5-T MRI machines may cause lower results than high-field machines, but it was confirmed by previous studies that the level of diagnostic accuracy in ACL and meniscal tears is comparable for low- and high-field-strength MRI [5].
We noted a high negative predictive value rendering MRI most useful as a negative diagnostic tool.
Arthroscopies allow reliable assessment of injury, but are invasive, expensive and require hospitalisation, anaesthesia and an experienced surgeon [15, 13].
Thomas et al. [14] suggested that when symptoms and clinical findings support the presence of meniscal or ligamentous injuries and arthroscopic therapeutic intervention is contemplated MRI is not always beneficial. The current practice of requesting scans to confirm the diagnosis should be altered. Unnecessary MRI increases the financial burden and delays treatment [14].
However, we agree with Crawford et al. [6] who stated that MRI is the most appropriate screening tool before arthroscopy. It is preferable to diagnostic arthroscopy in most patients because it avoids the surgical risks [6]. Also concerning the economic burden especially in a country like Egypt, MRI may decrease unjustified arthroscopies.
Conclusion
We recommend MRI as the primary diagnostic tool for internal knee derangements; however, arthroscopy should be done in cases where MRI findings do not agree with the clinical findings of the patients or in cases clinically diagnosed as complete ACL tears where reconstruction surgery is indicated.
Abbreviations
- MRI
magnetic resonance imaging
- ACL
anterior cruciate ligament
References
- 1.Barnett MJ. MR diagnosis of internal derangements of the knee: effect of field strength on efficacy. AJR Am J Roentgenol. 1993;161:115–118. doi: 10.2214/ajr.161.1.8517288. [DOI] [PubMed] [Google Scholar]
- 2.Barry KP, Mesgarzadeh M, Triolo J, et al. Accuracy of MRI patterns in evaluating anterior cruciate ligament tears. Skeletal Radiol. 1996;25(4):365–370. doi: 10.1007/s002560050096. [DOI] [PubMed] [Google Scholar]
- 3.Ben-Galim P, Steinberg EL, Amir H, et al. Accuracy of magnetic resonance imaging of the knee and unjustified surgery. Clin Orthop Relat Res. 2006;447:100–104. doi: 10.1097/01.blo.0000203471.50808.b7. [DOI] [PubMed] [Google Scholar]
- 4.Boeree NR, Watkinson AF, Ackroyd CE, et al. Magnetic resonance imaging of meniscal and cruciate injuries of the knee. J Bone Joint Surg Br. 1991;73:452–457. doi: 10.1302/0301-620X.73B3.1670448. [DOI] [PubMed] [Google Scholar]
- 5.Cotten A, Delfaut E, Demondion X, et al. MR imaging of the knee at 0.2 and 1.5 T: correlation with surgery. AJR Am J Roentgenol. 2000;174:1093–1097. doi: 10.2214/ajr.174.4.1741093. [DOI] [PubMed] [Google Scholar]
- 6.Crawford R, Walley G, Bridgman S, et al. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;84:5–23. doi: 10.1093/bmb/ldm022. [DOI] [PubMed] [Google Scholar]
- 7.Smet AA, Graf BK. Meniscal tears missed on MR imaging: relationship to meniscal tear patterns and anterior cruciate ligament tears. AJR Am J Roentgenol. 1994;162:905–911. doi: 10.2214/ajr.162.4.8141016. [DOI] [PubMed] [Google Scholar]
- 8.Esmaili Jah AA, Keyhani S, Zarei R, et al. Accuracy of MRI in comparison with clinical and arthroscopic findings in ligamentous and meniscal injuries of the knee. Acta Orthop Belg. 2005;71:189–196. [PubMed] [Google Scholar]
- 9.Helms CA. The meniscus: Recent advances in MR imaging of the knee. AJR Am J Roentgenol. 2002;179:1115–1122. doi: 10.2214/ajr.179.5.1791115. [DOI] [PubMed] [Google Scholar]
- 10.McNally EG. Magnetic resonance imaging of the knee is accurate and helps in making therapeutic decisions. BMJ. 2002;325(7356):115–116. doi: 10.1136/bmj.325.7356.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oei E, Nikken J, Verstijnen AC, et al. MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology. 2003;226:837–848. doi: 10.1148/radiol.2263011892. [DOI] [PubMed] [Google Scholar]
- 12.Rubin DA, Kettering JM, Towers JD, et al. MR imaging of knees having isolated and combined ligament injuries. AJR Am J Roentgenol. 1998;170:1207–1213. doi: 10.2214/ajr.170.5.9574586. [DOI] [PubMed] [Google Scholar]
- 13.Sanches Vas CE, Camargo O, Santana P, et al. Accuracy of magnetic resonance in identifying traumatic intraarticular knee lesions. Clinics (Sao Paulo) 2005;60(6):445–450. [PubMed] [Google Scholar]
- 14.Thomas S, Pullagura M, Robinson E, et al. The value of magnetic resonance imaging in our current management of ACL and meniscal injuries. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):533–536. doi: 10.1007/s00167-006-0259-7. [DOI] [PubMed] [Google Scholar]
- 15.Tsai KJ, Chiang H, Jiang CC. Magnetic resonance imaging of anterior cruciate ligament rupture. BMC Musculoskelet Disord. 2004;5:21. doi: 10.1186/1471-2474-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vincken PWL, Braak BP, Erkell AR, et al. Effectiveness of MR imaging in selection of patients for arthroscopy of the knee. Radiology. 2002;223:739–746. doi: 10.1148/radiol.2233010849. [DOI] [PubMed] [Google Scholar]
- 17.Winters K, Tregonning R. Reliability of magnetic resonance imaging of the traumatic knee determined by arthroscopy. N Z Med J. 2005;118(1209):U1301. [PubMed] [Google Scholar]