Abstract
The pilon fracture is a complex injury. The purpose of this study was to evaluate the outcome of minimally invasive techniques in management of these injuries. This was a prospective study of closed AO type C2 and C3 fractures managed by early (<36 hours) minimally invasive surgical intervention and physiotherapist led rehabilitation. Thirty patients with 32 intra-articular distal tibial fractures were treated by the senior surgeon (GK). Our aim was to record the outcome and all complications with a minimum two year follow-up. There were two superficial wound infections. One patient developed a non-union which required a formal open procedure. Another patient was symptomatic from a palpable plate inferiorly. An excellent AOFAS result was obtained in 83% (20/24) of the patients. Early minimally invasive reduction and fixation of complex high velocity pilon fractures gave very satisfactory results at a minimum of two years follow-up.
Résumé
Les fractures du pilon tibial sont toujours des fractures avec traumatisme complexe. Le but de cette étude est d’évaluer le devenir du traitement de ces fractures après utilisation de techniques dites mini-invasives. Matériel et méthode: une étude prospective portant sur des fractures de ce type fermées C2 et C3 dans la classification AO et traitées précocement (moins de 36 heures après le traumatisme) ont été inclues dans cette étude avec abord mini-invasif et rééducation rapide. 30 patients présentaient 32 fractures intra-articulaires, les patients ayant été traités par un chirurgien senior (GK). Le suivi de cette étude est de rapporter les complications et le devenir avec un suivi minimum de deux ans. Résultats, il faut déplorer deux infections superficielles, un patient présentant une pseudarthrose nécessitant un nouveau traitement chirurgical, un patient présentait des douleurs symptomatiques au niveau de la partie inférieure de la plaque d’ostéosynthèse. Un résultat excellent selon les critères de l’AOFAS a été obtenu dans 83% des cas (20/24). Conclusion: une réduction précoce par technique mini-invasive avec fixation permet d’avoir des résultats satisfaisants après un suivi minimum de deux ans dans ces fractures graves du pilon tibial.
Introduction
The pilon fracture extending from the distal tibial metaphysis into the ankle is a complex injury often associated with severe soft tissue damage. This combination of osseous and soft tissue trauma has long challenged surgeons.
In 1969, Reudi and Allgower reported a series of 82 patients with 84 fractures treated with a standard open protocol within six hours of injury; 74% of their patients reported good to excellent function, and 90% returned to their pre morbid occupation [22]. Prior to this calcaneal traction had been the treatment of choice [18]. Following the publication of this landmark paper open reduction and internal fixation was widely adopted; however, subsequent studies showed less favourable results, particularly when evaluating the more severe types of pilon fractures [17]. The authors of these later papers strongly advised that the soft tissue management was as important as the bony reconstruction [17].
A number of ‘newer’ surgical techniques have since been described in the literature and vary from percutaneous techniques, to limited open reduction, to treatment with external fixators (spanning, articulated, hybrid, etc.) alone or in combination with internal fixation [15, 20, 21, 25]. In spite of these advances the optimal technique for treating the more complicated pilon fracture remains controversial [18, 22].
In June 2003 we began treating intra-articular pilon fractures by a minimally invasive techniques. This change in practice was based on increasing experience with the techniques of minimally invasive fracture fixation, and the prospect of fewer soft tissue complications.
Our aims were to analyse the rate and type of complications associated with this technique as well as the overall outcome for patients in the longer term.
Patients and methods
Between June 2003 and July 2005, 30 patients with 32 intra-articular distal tibial fractures were treated by minimally invasive techniques.
Inclusion criteria consisted of a closed, displaced, comminuted pilon fracture (AO classification type C2 and C3) which had occurred as a result of high velocity trauma. Exclusion criteria consisted of open fractures and any previous bony injury to the foot or ankle. During the study period 16 cases of open pilon fractures had been treated in this practice. Treatment in this group consisted of external fixation of different types, for variable periods of time, with subsequent conversion to internal fixation in most cases.
This timescale was chosen to ensure a minimum two-year follow-up with completion of the study in July 2007.
The mean interval between injury and definitive surgical fixation by the method described was 28 hours (range, 6–36).
All fractures were evaluated with standard antero-posterior (AP) and lateral radiographs and computed tomography (CT). Classification of the bony injury was then undertaken using the AO comprehensive classification of distal tibial fractures [19].
The degree of soft-tissue injury was assessed and classified according to the system described by Tscherne and Gotzen [25]. This was done immediately prior to surgery, with the patient anaesthetised with full exposure of the injured limb.
All patients underwent regular out-patient review following hospital discharge until clinical and radiological union was confirmed. Plain radiographs of AP and lateral views were obtained at each visit, and any loss of reduction or hardware problems were recorded under complications. Subsequent follow-up was carried out in clinics specifically arranged for the purposes of the study. Six patients were lost to follow-up, leaving a total of 24 patients with 26 pilon fractures. There were 19 men and five women, with a mean age of 31 years (range, 18–45). The most common mechanism of injury was road traffic accidents, followed by falls from height.
At review clinics all bony and soft tissue complications were recorded. A specific assessment of foot and ankle outcome was undertaken using the American Orthopaedic Foot and Ankle score (AOFAS) [13]. This scale grades the ankle, subtalar, and talonavicular joints, with a maximum score of 100, where 50 points are given for function, 40 for pain, and ten for alignment. A score of 80–100 is excellent, 60–80 good, 40–60 satisfactory, and <40 poor. Scoring was undertaken on two separate occasions at a mean of nine and 24 months post operatively.
For the minimally invasive operative technique, patients were placed supine with the hip on the injured side at approximately 60° of flexion and the knee at 90°, with the foot firmly secured to the traction table. The uninjured limb was flexed at both the hip and knee to 90° and then internally rotated at the hip and supported in that position so as not to obscure the image intensifier. Intravenous antibiotic prophylaxsis was administered at induction (cefuroxime 1.5 g). No tourniquet was used.
The operation was carried out in four steps, all under radiological control.
Increasing traction was applied in the long axis line of the tibia. Manipulation of the foot and ankle while on traction with alternating rotation, varus/valgus, and pro/recurvatum movements allowed for disimpaction of the main fractures fragments and gross realignment. Sufficient traction was kept on to maintain the reduction and the image obtained compared with AP and lateral radiographs of the contralateral ankle, displayed in operating room, to ensure the re-establishment of the normal distal tibiofibular relationship. This then defined the level of tibial reconstruction.
The second step involved the anatomical reduction of the main fracture fragments. This was undertaken through small 5-mm stab incisions and manipulation of the fragments into place with a spiked bone probe. Where tendons were encountered they were mobilised sufficiently to ensure no injury. These fragments were then provisionally stabilised with K wires or large AO reduction clamps.
The third step following provisional reduction and stabilisation involved the insertion of an ankle arthroscope through medial and or lateral portals. Constant suction was used in the ankle joint through a wide bore cannula for all arthroscopies. The quality of the articular reduction was then checked, and any minor alterations undertaken. Small articular fragments not amenable to reconstruction were then removed from the joint.
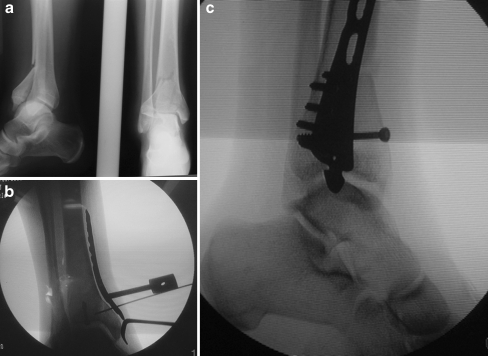
In the fourth and final step small fragment lag screws were inserted to compress the main fragments together. The arthroscope was re-introduced to assess the final reduction. A 1–2 cm vertical incision was then made immediately distal to the medial malleolus. An extraperiosteal corridor was created through this incision by sliding a long curved forceps up the medial side of the tibial shaft. A distal tibial locking plate (AO, Synthes, Solothurn, Switzerland) of sufficient length to provide three holes proximal to the most proximal extent of the fracture was then inserted. A combination of locking and nonlocking screws were used. The plate was sized under image control prior to insertion (Fig. 1a, b, c). No fibular fixation was necessary in any case following reduction and stabilisation with the medial locking plate
Fig. 1.
a Plain radiographs of a 19-year-old male who sustained this injury in a road traffic accident. b Intraoperative image of the sizing of a medial locking plate following reduction with traction and probe. An antero-posterior screw has already been inserted. c Final intraoperative image showing restoration of articular surface
Postoperatively a posterior slab was applied to the ankle in the neutral position, and the extremity was elevated. After 48 hours the slab was removed and a soft ankle brace applied, which allowed a full range of movement but prevented a resting equines position. Daily physiotherapy was prescribed commencing 48 hours post-op, and the foot was kept elevated for the first two weeks (bed to toilet). Partial weight bearing with crutches was commenced six weeks post-op, with full weight bearing at ten weeks.
Results
Mean follow-up was 28 months (range, 24–34).
A satisfactory reduction was obtained in all cases; this was based on no/minimal articular step-off evident on arthroscopy and fluroscopy after final fixation and anatomical realignment of the metaphyseal/diaphyseal components.
There were two superficial wound infections which resolved with daily dressings and oral antibiotics. One patient developed a non-union which required a formal open procedure with bone grafting and exchange plating. Another patient was symptomatic from a proud palpable plate inferiorly; this was removed at six months following union.
An excellent AOFAS result was obtained in 83% (20/24) of the patients (Table 1).
Table 1.
Patient data
| Gender | Age (y) | MOI | AO fracture type | T&G soft tissue | AOFAS | |
|---|---|---|---|---|---|---|
| (9) | (24) | |||||
| Male | 30 | RTA | C2 | II | 85 | 86 |
| Male | 19 | RTA | C3 | I | 86 | 88 |
| Female | 28 | RTA | C2 | II | 87 | 86 |
| Male | 43 | Fall | C3 | II | 82 | 84 |
| Male | 35 | RTA | C2 | II | 75 | 76 |
| Female | 44 | Fall | C3 | II | 86 | 88 |
| C3 | II | 84 | 84 | |||
| Male | 23 | RTA | C2 | III | 84 | 84 |
| Male | 27 | RTA | C2 | II | 86 | 88 |
| Female | 32 | RTA | C3 | I | 88 | 86 |
| Male | 25 | RTA | C2 | II | 88 | 88 |
| Female | 23 | RTA | C3 | II | 87 | 88 |
| Male | 23 | RTA | C2 | I | 88 | 86 |
| C3 | II | 82 | 84 | |||
| Male | 34 | Fall | C2 | II | 88 | 86 |
| Male | 23 | RTA | C3 | I | 86 | 86 |
| Male | 25 | Fall | C2 | III | 78 | 76 |
| Male | 29 | Fall | C3 | III | 86 | 88 |
| Male | 24 | RTA | C2 | II | 74 | 76 |
| Female | 33 | RTA | C2 | I | 83 | 84 |
| Male | 41 | Fall | C2 | II | 86 | 88 |
| Male | 34 | RTA | C3 | II | 88 | 86 |
| Male | 45 | RTA | C3 | III | 86 | 86 |
| Male | 39 | Fall | C2 | II | 78 | 76 |
| Male | 31 | RTA | C3 | I | 86 | 86 |
| Male | 34 | RTA | C2 | II | 84 | 86 |
MOI mechanism of injury, RTA road traffic accident, AO fracture type AO comprehensive classification of distal tibial fractures, T&G soft tissue Tscherne and Gotzen classification of soft tissue injury in closed fractures, AOFAS American Orthopaedic Foot and Ankle score recorded at a mean of 9 months (9), and 24 months (24) postoperatively
There was no overall difference seen in outcome in patients with C2 or C3 fractures or increasing grades of soft tissue injury when treated by this method.
Discussion
Historically fractures of the lower end of the tibia into the ankle joint were regarded as ‘not being amenable to internal fixation’. Skeletal traction through the os calcis was the standard treatment and post-traumatic osteoarthritis and stiffness the rule [18].
Despite the fact that it is now over 30 years since the landmark paper by Reudi and Algower, the treatment of these injuries remains controversial [18, 22, 23].
What has been made definitively clear in the literature is that minimising soft tissue damage is essential to prevent potentially severe complications such as wound breakdown, osteomyelitis, infected non unions, and amputations [4, 6, 10, 17].
The rate of superficial wound infection following open reduction and internal fixation (ORIF) has been reported in the range of 27–36% [8]. Terry et al. reported that superficial wound problems increased the risk for deep infection six-fold [23]. McFerran et al. reviewed 52 pilon fractures treated by ORIF and reported a major local complication rate in 40% of his patients necessitating 77 additional procedures [17].
Recognition of the soft tissue problems has led surgeons to use alternative techniques in the management of these complex injuries. Minimally invasive techniques have been described by a number of authors with reduced incidence of soft tissue complications [1, 11]. In these studies the fracture was initially stabilised by external fixation and, when the soft tissues had recovered, reduced and fixed through minimal incisions based on ‘fracture corridors’, percutaneous screws, and tunnelled plates.
The timing of operative intervention is also controversial with advocates for both immediate and delayed surgery [3, 12, 14, 16]. We attempted to perform definitive reduction and stabilisation as soon as the patient was medically fit, and all patients had surgery within 36 hours.
A large part of our reduction was dependent on ligamentotaxis through traction and manipulation, and we felt that this would be most effective if done on the ‘fresh’ fracture. Pai et al., using indirect reduction techniques and minimally invasive plate fixation, reported good to excellent results in all 26 of their patients [20]. Treatment regimens for pilon fractures which wait for the soft tissue injury to recover before definitive operative fixation report latency periods of seven to 21 days [2, 5, 9]. There is also evidence in the literature to suggest that delayed intervention makes accurate surgical reduction of these fractures more difficult [16].
Our second reason for favouring early intervention was the potential benefit for the soft tissues with stabilisation of the bony injury. In high velocity injuries early bony stabilisation has been shown to limit further soft tissue damage, decrease the risk of further bacterial spread, improve the blood flow and venous return in the limb, and reduce post-traumatic oedema, pain, and stiffness [21]. We had two superficial wound infections in this series which compares very favourably to other reports on minimally invasive fixation of pilon fractures [1, 11]. Lau et al., in their study of 48 cases of minimally invasive fixation of distal tibial fractures, reported an infection rate of 15%; however, overall they reported a good clinical outcome with this technique [15].
A major concern when using minimally invasive techniques, particularly in intra-articular fractures, is the quality of the reduction, with poor reduction predisposing to post-traumatic joint degeneration [24]. Heather et al. reported a low early complication rate in their series of 19 pilon fractures fixed by minimally invasive techniques; however, their follow up was for six months only, and they have recognised this as a shortcoming of their study [6]. Our mean follow-up was over two years. By evaluating function, pain, and alignment with the use of the American Orthopaedic Foot and Ankle score (AOFAS), we feel a realistic picture of the longer term outcome of this technique has been obtained.
This study is unique for a number of reasons. Previous studies evaluating minimally invasive treatment of pilon fractures have generally consisted of a mixed group of high and low velocity fracture types. Treatment has also varied with some patients in these studies being managed with a temporary period of external fixation and/or initial fibular fixation with delayed tibial fixation. All of our patients sustained high velocity injuries, and all were treated by early definitive internal fixation and early rehabilitation as described.
We would like to acknowledge the limitations in this study, predominantly, the small patient number and the lack of a control group.
Another major potential drawback with our treatment regime is the surgical skill and experience required to carry it out accurately. This study was undertaken in a busy regional trauma orthopaedic centre surrounded by a large number of major roads; thus we see and treat a significant number of patients who have been exposed to high velocity trauma. Generally however pilon fractures are relatively rare injuries representing 5–7% of all tibial fractures [7]. All operations in this study were carried out by the senior surgeon. The general orthopaedic surgeon who only treats one or two of these complex injuries per year may be better served by using more standard techniques.
In conclusion we have found that early minimally invasive reduction and fixation of complex high velocity pilon fractures combined with early rehabilitation gave an excellent result in 83% of our patients at a minimum of two-year follow-up, with comparable early complications. However, these are severe injuries and each should be treated individually based on the complexity of the fracture, extent of the soft tissue trauma, and perhaps most importantly on the skill, experience, and resources of the surgical team.
References
- 1.Blauth M, Bastian L, Krettek C, et al. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001;15:153–160. doi: 10.1097/00005131-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Bonar SK, Marsh JL. Unilateral external fixation for severe pilon fractures. Foot Ankle. 1993;14:57–64. doi: 10.1177/107110079301400201. [DOI] [PubMed] [Google Scholar]
- 3.Bone LB. Fractures of the tibial plafond: the pilon fracture. Orthop Clin North Am. 1987;18:93–104. [PubMed] [Google Scholar]
- 4.Borrelli J, Jr, Ellis E. Pilon fractures: assessment and treatment. Orthop Clin North Am. 2002;33:231–245. doi: 10.1016/S0030-5898(03)00082-8. [DOI] [PubMed] [Google Scholar]
- 5.Borrelli J, Jr, Catalano L. Open reduction and internal fixation of pilon fractures. J Orthop Trauma. 1999;13:573–582. doi: 10.1097/00005131-199911000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Bourne RB, Horabeck CH, MacNab BA. Intra-articular fractures of the distal tibia: the pilon fracture. J Trauma. 1983;23:591–596. doi: 10.1097/00005373-198307000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Bourne RB, Rorabeck CH, McNab J. Intra-articular fracture of the distal tibia: the pilon fracture. J Trauma. 1983;23:591–595. doi: 10.1097/00005373-198307000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Dillin L, Land P, Slabaugh P. Delayed wound healing, infection, and nonunion following open reduction and internal fixation of tibial plafond fractures. J Trauma. 1986;26:1116–1119. doi: 10.1097/00005373-198612000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Egol K, Wolinsky P, Koval KJ. Open reduction and internal fixation of tibial pilon fractures. Foot Ankle Clin. 2000;5:873–885. [PubMed] [Google Scholar]
- 10.Etter C, Ganz R. Long-term results of tibial plafond fractures treated with open reduction and internal fixation. Arch Orthop Trauma Surg. 1991;110:277–283. doi: 10.1007/BF00443458. [DOI] [PubMed] [Google Scholar]
- 11.Helfet DL, Shonnard PY, Levine D, et al. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997;28(suppl 1):SA42–SA48. doi: 10.1016/s0020-1383(97)90114-5. [DOI] [PubMed] [Google Scholar]
- 12.Jergesen F. Fractures of the ankle. Am J Surg. 1959;98:136–145. doi: 10.1016/0002-9610(59)90057-1. [DOI] [PubMed] [Google Scholar]
- 13.Kitaoka HB, Alexander IJ, Adelaar RS. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 14.Leone VJ, Ruland RT, Meinhard BP. The management of the soft tissues in pilon fractures. Clin Orthop Relat Res. 1993;292:315–320. [PubMed] [Google Scholar]
- 15.Lau TW, Leung F, Chan CF, et al. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2007;16(4):491. doi: 10.1007/s00264-007-0384-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mandracchia VJ, Evans RD, Nelson SC, et al. Pilon fractures of the distal tibia. Foot Ankle Trauma. 1999;16:743–767. [PubMed] [Google Scholar]
- 17.McFerran MA, Smith SW, Boulas HJ, et al. Complications encountered in the treatment of pilon fractures. J Orthop Trauma. 1992;6:195–200. doi: 10.1097/00005131-199206000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Metcalfe BP. Pilon fractures of the tibia. Curr Orthop. 2003;17(3):190–199. doi: 10.1016/S0268-0890(03)00044-6. [DOI] [Google Scholar]
- 19.Müller ME, Nazarian S, Koch P et al (eds) (1994) The comprehensive classification of fractures of long bones. Springer, Berlin
- 20.Pai V, Coulter G, Pai V. Minimally invasive plate fixation of the tibia. Int Orthop. 2007;31(4):491–496. doi: 10.1007/s00264-006-0228-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma. 1999;13:85–91. doi: 10.1097/00005131-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Ruëdi T, Allgöwer M. Fractures of the lower end of the tibia into the ankle joint. Injury. 1969;1:92–99. doi: 10.1016/S0020-1383(69)80066-5. [DOI] [Google Scholar]
- 23.Teery SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Clin Orthop. 1993;292:108–117. [PubMed] [Google Scholar]
- 24.Thordarson DB. Complications after treatment of tibial pilon fractures: prevention and management strategies. J Am Acad Orthop Surg. 2000;8(4):253–265. doi: 10.5435/00124635-200007000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Tscherne H, Gotzen L (eds) (1984) Fractures with soft tissue injury. Springer, Berlin