Abstract
The purpose of this study was to describe soft tissue injury patterns and report the clinical results of primary ligament repair with use of protected early mobilisation in unstable elbow dislocations with pure capsulo-ligamentous injuries. Twenty-four patients who presented with traumatic unstable elbow dislocation without associated intra-articular fracture were reviewed. Anatomical repair was performed using metal anchor screws and the bone tunnel method. Ligament avulsion was noted in 55% for the medial collateral ligament, 80% for the lateral collateral ligament, 60% for the flexor tendon and 80% for the extensor tendon. The overall mean Mayo Elbow Performance Score was 93.2. Brachial artery injuries occurred in two elbows. Heterotopic calcification was noted in 14 patients and there was one severe traumatic arthrosis. This study showed a high incidence of reattachable avulsion injuries to ligaments, tendon/muscle and capsule in unstable elbow dislocations. Primary ligament repair coupled with early rehabilitation provided satisfactory outcomes at two to four years postoperatively.
Résumé
Le but de cette étude est de décrire les lésions et de rapporter les résultats chez les patients présentant une luxation du coude avec lésion ligamentaire traitée par réparation ligamentaire et mobilisation précoce. Matériel et méthode: 24 patients présentant ce type de traumatisme sans lésion fracturaire intra articulaire ont été revus. Les lésions anatomiques ont été réparées avec soit une ancre soit une fixation ligamentaire par tunnels trans-osseux. Résultats: l’avulsion ligamentaire est notée dans 55% des cas pour le MCL, dans 80% pour le LCL, dans 60% pour le tendon fléchisseur et dans 80% dans le tendon extenseur. En tout état de cause, le score MEPS a été de 93,2. Une lésion de l’artère humérale a été observée sur deux coudes et des lésions de calcifications hétérotypiques ont été observées chez 14 patients avec, dans un cas, une arthrose sévère. Conclusion: cette étude montre l’influence que peut avoir la réinsertion ligamentaire dans ces lésions secondaires à une luxation du coude. Les réparations précoces associées à une réhabilitation également précoce permettent d’avoir des résultats satisfaisants après deux mois de suivi post-opératoire.
Introduction
Elbow dislocations are categorised anatomically as simple (with no associated fracture) or complex (with associated fracture) [22]. Simple dislocations are much more common than complex dislocations and the risk of recurrent or chronic instability is increased significantly with complex dislocations [13]. Most unstable elbow dislocations are associated with intra-articular fractures such as radial head or coronoid process fractures, and it is apparent that elbow dislocations associated with intra-articular fracture often result in poor results with conservative treatment [5, 11, 12, 17].
However, the management of acute simple elbow dislocation which has been redislocated after closed reduction remains a challenge because of its rarity and limited knowledge in the literature of the soft tissue injury pattern and treatment protocol with respect to which anatomical structure should be repaired for a successful outcome [7, 20].
The purpose of this study was to evaluate the injured anatomical structure of this type of acute unstable elbow dislocation with pure capsulo-ligamentous injuries which had been redislocated after closed reduction and to assess the clinical outcomes of a treatment protocol that included surgical treatment within two weeks addressing all injured ligaments and early protected postoperative rehabilitation.
Materials and methods
Patients
Twenty consecutive patients treated by a single surgeon were evaluated in one tertiary trauma centre between January 2003 and December 2005.
We defined acute surgical treatment as that performed within the first three weeks after the injury [6]. Surgical indications of the unstable elbow were subluxation or non-congruent elbow joint on the radiographs following closed reduction. Elbow dislocation which required an extension block splint over 45° to maintain reduction was considered as an unstable elbow dislocation as previously described by Morrey and O’Driscoll [15, 21].
Patients with associated fracture in the elbow joint such as radial head or coronoid process, delayed presentation more than three weeks after the initial trauma and any dislocations with an open wound were excluded from this study.
There were 18 men and two women with an average age of 34 years (range: 18–72 years). The cause of injury was a fall from a height in 11, road traffic accident in five and sports injury in four. The mean time from injury to operation was 3.5 days (range: 1–14 days).
The injured structure was identified on plain radiographs in all and magnetic resonance imaging (MRI) in 15 patients at the time of the operation. When there was a difference between MRI and intraoperative findings, the findings at surgery were those recorded, as MRI does not necessarily differentiate between severe strain and discontinuity of ligamentous structure [16]. An attempt was made to visualise all structures identified at MRI as being injured at the time of surgery. The definitions of sites of injury are modified from Twaddle et al. [24] and outlined in Table 1.
Table 1.
Definition of sites of injury
| Site of injury | Definition |
|---|---|
| Ligament injury—proximal avulsion | Avulsion with piece of bone or periosteum |
| Ligament injury—midsubstance tear | No bone or periosteum attached |
| Ligament avulsion—distal avulsion | Avulsion with piece of bone or periosteum |
| Capsular injury—proximal capsular side | Capsular injury—humeral side |
| Capsular injury—distal capsular side | Capsular injury—ulnar side |
| Tendon injury/avulsion | Pure tendon rupture or avulsion with piece of bone or periosteum |
| Tendon injury—musculotendinous junction | Separation at musculotendinous junction |
| Muscle belly | Rupture of belly of muscle |
Surgical management
Skin incision was determined by the pattern of injury. For combined injuries of the medial and lateral collateral ligaments, a 5- to 6-cm lateral incision (modified Kocher’s posterolateral approach) was used centred over the lateral epicondyle. Torn lateral collateral ligament complex and joint capsule were repaired with metal anchor screws (Twinfix, Smith & Nephew, Memphis, TN, USA) and common extensor tendon with use of non-absorbable sutures (5-0 Ethibond, Ethicon, Johnson & Johnson, Somerville, NJ, USA) using the bone tunnel method. Then the medial collateral ligament and flexor tendon were addressed. The final fixation of the soft tissue structure was performed with elbow flexion at 30°. After surgery addressed both the medial and lateral structures, if there was persistent anterior subluxation at full extension, then the anterior capsule and brachialis muscle attachments were repaired.
To protect the repaired soft tissue structure, the elbow was placed in a postoperative brace at resting state that was locked in 30° of flexion for the first three weeks. Passive flexion and extension exercise with use of gravity was initiated at three days postoperatively. A hinged plastic brace was applied afterwards and protected for eight weeks postoperatively.
All patients were followed up clinically and radiologically at a mean time of 20.5 months (range: 14–36 months) after operation. The Mayo Elbow Performance Score (MEPS) [14] was used for clinical outcome and post-traumatic degenerative changes were assessed on the radiographs using the scale described by Broberg and Morrey [1].
Results
The incidence of associated injuries and details of the patients are given in Table 2. Associated injuries were recorded in 13 patients (70%).
Table 2.
Details of the patients with unstable elbow dislocation
| No. | Gender | Age | Mechanism | Side | Associated injury | Surgical indicationa | MCL | Flexor | LCL | Extensor | Capsule | Brachialis muscle | ROM | MEPS | Arthrosis | HO | Cx | FU |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 22 | Triathlon | R | 2 | X | X | X | Y | 0–135 | 100 | 0 | M | 28 | ||||
| 2 | M | 27 | Fall | L | 1 | Y | X | X | 10–135 | 85 | 0 | MCL laxity | 32 | |||||
| 3 | M | 46 | Fall | R | Spine fx | 1 | X | X | X | 15–110 | 80 | 1 | M/L | 38 | ||||
| Brachial a. injury | ||||||||||||||||||
| 4 | M | 40 | RTA | R | ICH | 1 | X | X | X | X | X | Y | 20–120 | 100 | 0 | M/L/A/P | 32 | |
| 5 | M | 25 | Fall | R | 1 | Y | Y | X | X | 15–130 | 100 | 0 | L | 31 | ||||
| 6 | M | 27 | RTA | R | 1 | X | X | 10–130 | 100 | 0 | 35 | |||||||
| 7 | M | 18 | Judo | R | UN | 2 | X | X | X | Y | 0–135 | 100 | 0 | M | 28 | |||
| 8 | M | 23 | Fall | L | 1 | Y | Y | X | X | 15–130 | 100 | 0 | M | MCL laxity | 35 | |||
| 9 | M | 23 | Fall | R | UN | 1 | X | X | 15–130 | 100 | 1 | L | Open arthrolysis | 28 | ||||
| 10 | M | 21 | Fall | R | 2 | X | X | X | Y | 15–135 | 100 | 0 | L | 28 | ||||
| 11 | F | 50 | Fall | L | Calcaneus fx | 2 | X | X | 5–130 | 100 | 0 | 48 | ||||||
| 12 | M | 50 | RTA | R | Pelvic bone fx | 1 | X | X | Y | 20–130 | 85 | 1 | 36 | |||||
| 13 | M | 37 | Fall | L | UN | 2 | X | X | X | X | X | Y | 5–130 | 100 | 0 | 24 | ||
| 14 | M | 46 | RTA | L | Mandible, spine fx | 1 | X | X | 10–130 | 100 | 0 | L | 34 | |||||
| ICH | ||||||||||||||||||
| 15 | M | 43 | Fall | R | Spine fx | 2 | X | X | X | X | X | X | 15–135 | 100 | 0 | M/L | 38 | |
| UN | ||||||||||||||||||
| 16 | M | 24 | Judo | R | 2 | X | X | X | Y | 20–120 | 80 | 1 | M | 27 | ||||
| 17 | M | 35 | Fall | R | Brachial a. injury | 2 | X | X | X | X | X | X | 45–90 | 50 | 3 | M/L/A/P | Open arthroslysis | 37 |
| UN | ||||||||||||||||||
| Distal radius fx | UN decomp. | |||||||||||||||||
| 18 | M | 29 | RTA | R | Tibia fx | 1 | X | X | 10–135 | 100 | 0 | L | 34 | |||||
| 19 | M | 21 | Judo | L | Mandible fx | 2 | X | X | X | X | X | X | 20–130 | 100 | 0 | 24 | ||
| 20 | F | 72 | Fall | L | Distal radius fx | 1 | X | X | 20–130 | 85 | 1 | 32 | ||||||
| Av | 34 | 14.25–127.5 | 93.2 | 32.45 |
a1 subluxation of a non-congruent elbow joint on the radiograph following closed reduction, 2 extension block splint over 45° to maintain a reduction
M male, F female, RTA road traffic accident, R right, L left, ICH intracranial haemorrhage, fx fracture, Brachial a. injury brachial artery injury, UN ulnar nerve symptoms, MCL medial collateral ligament, Flexor flexor tendon, LCL lateral collateral ligament complex, Extensor extensor tendon, HO heterotopic ossification, M medial, L lateral, A anterior, P posterior, X complete rupture, Y partial rupture, ROM range of motion, MEPS Mayo Elbow Performance Score, FU follow up, Av average
Operative findings
The number of ligaments injured in each elbow and patterns are shown in Table 3. All ligament injuries were of the proximal avulsion type apart from two partial injuries of the medial collateral ligament. Partial tears were often identified by preoperative MRI which showed a high signal intensity lesion, but examination at the time of surgery was still significant for an end point to valgus/varus and pivot shift test or at the time of surgery, they were still in continuity.
Table 3.
Frequency of collateral ligament injury in study elbows
| Soft tissue | Frequency of injury (%) | Proximal avulsion (n) | Distal avulsion (n) | Midsubstance (n) | Partial injury (n) | Total |
|---|---|---|---|---|---|---|
| MCL | 55 | 7 | – | 2 | 2 | 11 |
| LCL | 80 | 16 | – | – | – | 16 |
MCL medial collateral ligament, LCL lateral collateral ligament
Associated tendon and anterior capsule injuries are outlined in Table 4. This shows some comparison between the flexor and extensor tendon injury patterns. Extensor tendons are exclusively avulsed with collateral ligaments (Fig. 1), whereas some flexor tendons (four elbows) are torn at the musculotendinous junction (Fig. 2). Brachialis injuries were closely associated with capsular injury.
Table 4.
Frequency of anterior capsule, tendon and muscle injury in study elbows
| Soft tissue | Frequency of injury (%) | Avulsion (n) | Musculotendinous junction (n) | Proximal capsular injury (n) | Distal capsular injury (n) | Total |
|---|---|---|---|---|---|---|
| Flexor tendon | 60 | 8 | 4 | – | – | 12 |
| Extensor tendon | 80 | 16 | 0 | – | – | 16 |
| Brachialis muscle | 45 | 0 | 9 | – | – | 9 |
| Anterior capsule | 55 | – | – | 6 | 5 | 11 |
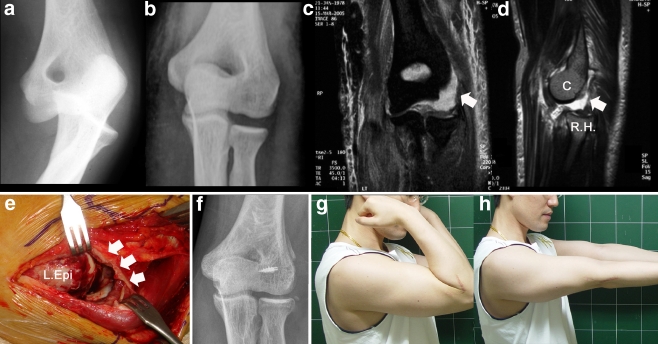
Fig. 1.
Case 4: a 27-year-old man with injuries of the lateral collateral ligament and common extensor tendon. a Preoperative plain radiograph. b Post-reduction radiograph. c, d Post-reduction magnetic resonance image showing injuries of the lateral collateral ligament complex (white arrows) with posterolateral subluxation of the radial head (R.H.) from the capitellum (C). e Intraoperative photograph of the lateral epicondyle (L. Epi). Note the complete avulsion of the collateral ligament, common extensor tendon from the lateral epicondyle. f Postoperative radiograph. g, h Photographs at last follow-up
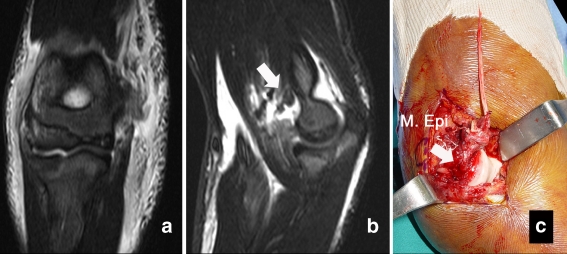
Fig. 2.
Case 5: an 18-year-old judo player. There was a palpable gap between the ruptured flexor tendon ends. a, b Magnetic resonance image showing injuries of the medial collateral ligament, flexor tendon and anterior capsule. Partial tear of the brachialis (white arrow) was noted. c Intraoperative photograph of the medial epicondyle (M. Epi) showing the complete avulsion of the collateral ligament from the medial epicondyle (white arrow) and flexor tendon at musculotendinous junction. The anterior capsule was avulsed from the humeral attachment
Two patients (10%) presented brachial artery injury which required a vein graft by vascular surgeons. One patient with combined brachial artery injury and comminuted intra-articular distal radius fracture required open arthrolysis for the stiff elbow, but the functional result was graded as poor at the last follow-up because of advanced traumatic arthrosis and stiffness of the elbow.
Ulnar nerve palsy occurred in four elbows preoperatively (20%). All presented mild ulnar nerve dysfunction (McGowan grade I) [10]. During the operation, there was no disruption of the nerve and mild stretching was noted. One patient with persistent ulnar nerve symptoms required a decompression procedure at six months postoperatively. When the nerve was explored, it was found to be entrapped by fibrotic scar tissue adhered to the flexor muscles and also behind the medial epicondyle. The symptoms were relieved six weeks after operation. The remaining two patients recovered completely without further surgical treatment in three months.
Clinical results
The overall mean functional MEPS was 93.2 (range: 50–100). The average extension loss was 14.3° (range: 0–45°) and the flexion averaged 127.5° (range: 90–135°).
Concentric stability was achieved in all patients measured clinically and radiographically. On examination of the elbow, 18 patients had a firm end point during the valgus stress test. Although no patient had subjective evidence of instability, two patients who had undergone repair of the lateral collateral ligament only revealed minor valgus laxity. Varus stress on pronation revealed mild laxity in three patients. None of the patients had a positive pivot shift test.
Complications
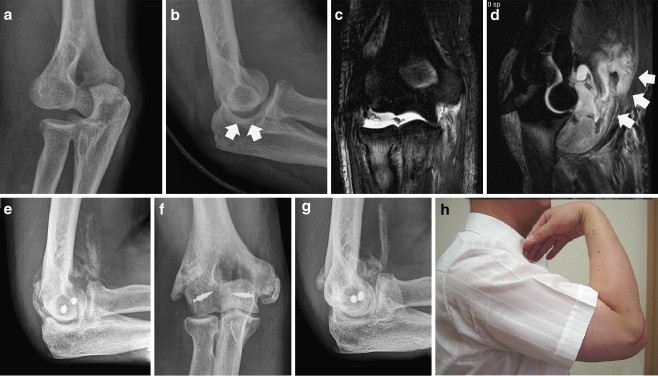
Heterotopic calcification of the joint capsule and collateral ligaments was noted in 13 patients (65%) during the follow-up period. In most patients, this was not clinically significant. One patient with brain injury presented massive calcification of the brachialis muscle with substantial loss of flexion and extension during the rehabilitation (45–90°). This huge calcification resolved radiographically in the ensuing six months; however, circumferential periarticular calcification remained until the last follow-up at 24 months. The patient refused further surgery because the range of motion at last follow-up was 20–120° with no signs of instability (Fig. 3). Spotty calcification around the lateral epicondyle and along the lateral collateral ligament complex was found in five patients (25%) and at the medial epicondyle and collateral ligament in four (20%) and at both the medial and lateral in four (20%).
Fig. 3.
Case 12: a 40-year-old man with injuries of both medial and lateral structures. a Initial plain radiograph. b Non-congruent ulnohumeral joint after closed reduction (white arrows). c, d Post-reduction magnetic resonance image showing injuries of the medial, lateral collateral ligament complex and anterior capsule with large haematoma (white arrows) in the anterior compartment. e Calcification in the brachialis which limited range of motion during rehabilitation. f, g Plain radiographs at 32 months postoperatively. h Photograph at last follow-up
Post-traumatic degenerative change was found in six patients (30%): five grade 1 and one grade 3 according to the scale of Broberg and Morrey [1].
Discussion
The surgical findings in this study are consistent with the other studies of Josefsson et al. [9]. In their series of 31 simple elbow dislocations, nine elbows were easily redislocated in the semiflexion position. They concluded that all of the ligaments were completely ruptured or avulsed in the epicondyle and the degree of muscle damage was correlated with the redislocation under anaesthesia. Rodgers et al. [18] reported 17 patients in a series of mixed fracture dislocation and found that 15 of 17 required medial collateral ligament and flexor-pronator origin repair and 10 of 17 underwent lateral collateral ligament repair.
The importance of the anterior capsule and brachialis muscle has been asserted by other authors. Dryer et al. [4] argued that avulsion of the brachialis and anterior capsule from the ulnar side should be repaired to avoid recurrent subluxation or dislocation. This is especially meaningful in the unstable elbow dislocation which has extensive damage to the soft tissue structures [23]. Of 20 elbows in this study, seven (35%) revealed either anterior capsular injury or brachialis muscle injury or both.
A study of the anatomy, mechanism of injury and clinical features suggested that there were soft tissue injuries around the elbow joint after dislocation [9]. The roles of the flexor-pronator and common extensor origins are, however, not fully understood. They are probably crucial stabilisers of the elbow next to articular constraint [3, 13]. In our series, the frequency of tendon injuries in unstable elbow dislocations was between 60 and 80%.
The indication for acute ligament repair or reconstruction is instability that does not permit early protected motion in a cast brace [5, 9]. This usually occurs only when there are associated fractures. In such cases, the ligaments may have been avulsed and can be repaired directly to the bone with heavy sutures [18]. If they are torn and cannot be repaired, reconstruction of the ligament using the palmaris longus tendon is recommended. Sanchez and his associates [19] reviewed and compared a clinical series of primary ligament repair and ligament reconstruction. Repair or reconstruction of the lateral collateral ligament complex initially improved or eliminated instability of the elbow in all but five of 45 patients (89%).
Plain radiographs and MRI provide valuable information on which sides of soft tissue were damaged [24]. In most cases, the common extensor tendon together with the lateral collateral ligament complex were ruptured or avulsed from the lateral epicondyle. On the other hand, the medial collateral ligament and capsule were avulsed from the humeral attachment and flexor-pronator tendons were torn at the musculotendinous junction, leaving some remaining soft tissue in the medial epicondyle. Spontaneous posterior subluxation at extension is consistent with complete disruption of both collateral ligaments and anterior capsular injury with or without brachialis muscle injury.
Postoperative stiffness is much more common than instability after elbow dislocation [2]. The average extension loss was 14.25° with average flexion of 127.5°. Heterotopic ossification is common after elbow dislocation reported in approximately 75% [8]. However, true ossification that limits motion is rare and fewer than 5%, which was a similar finding in our series [1, 2].
The limitation of this study is that it is a retrospective observational study in a selective population of a tertiary trauma centre. As we do not have preoperative clinical scores, it is not possible to compare the clinical results of the operation directly before and after operation. However, considering the fact that unstable simple dislocation of the elbow is relatively rare and has been rarely reported in the literature, this study is one of the largest series analysing the injured structure, pattern and clinical outcome of primary ligament repair.
In conclusion, primary soft tissue repair to treat unstable elbow dislocation provided satisfactory functional results, range of motion and stability in the majority of patients. Anatomical restoration of the soft tissue stabiliser of the elbow joint is important in this type of unstable elbow so that a complicated secondary reconstruction procedure could be avoided. Because of the high incidence of soft tissue avulsions shown in this study, early primary ligament repair followed by an early mobilisation programme is indicated in this type of injury. Further studies are required to validate our clinical results.
References
- 1.Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669–674. [PubMed] [Google Scholar]
- 2.Cohen MS, Hastings H., 2nd Acute elbow dislocation: evaluation and management. J Am Acad Orthop Surg. 1998;6:15–23. doi: 10.5435/00124635-199801000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Deutch SR, Jensen SL, Tyrdal S, Olsen BS, Sneppen O. Elbow joint stability following experimental osteoligamentous injury and reconstruction. J Shoulder Elbow Surg. 2003;12:466–471. doi: 10.1016/S1058-2746(03)00062-4. [DOI] [PubMed] [Google Scholar]
- 4.Dryer RF, Buckwalter JA, Sprague BL. Treatment of chronic elbow instability. Clin Orthop Relat Res. 1980;148:254–255. [PubMed] [Google Scholar]
- 5.Dürig M, Müller W, Rüedi TP, Gauer EF. The operative treatment of elbow dislocation in the adult. J Bone Joint Surg Am. 1979;61:239–244. [PubMed] [Google Scholar]
- 6.Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86:262–273. doi: 10.2106/00004623-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Josefsson PO, Gentz CF, Johnell O, Wendeberg B. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint. A prospective randomized study. J Bone Joint Surg Am. 1987;69:605–608. [PubMed] [Google Scholar]
- 8.Josefsson PO, Johnell O, Gentz CF. Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg Am. 1984;66:927–930. doi: 10.2106/00004623-198466060-00014. [DOI] [PubMed] [Google Scholar]
- 9.Josefsson PO, Johnell O, Wendeberg B. Ligamentous injuries in dislocations of the elbow joint. Clin Orthop Relat Res. 1987;221:221–225. [PubMed] [Google Scholar]
- 10.McGowan AJ. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg Br. 1950;32:293–301. doi: 10.1302/0301-620X.32B3.293. [DOI] [PubMed] [Google Scholar]
- 11.McKee MD, Bowden SH, King GJ, Patterson SD, Jupiter JB, Bamberger HB, Paksima N. Management of recurrent, complex instability of the elbow with a hinged external fixator. J Bone Joint Surg Am. 1998;80:1031–1036. doi: 10.1302/0301-620X.80B6.8536. [DOI] [PubMed] [Google Scholar]
- 12.McKee MD, Pugh DM, Wild LM, Schemitsch EH, King GJ. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. Surgical technique. J Bone Joint Surg Am. 2005;87(Suppl 1):22–32. doi: 10.2106/JBJS.D.02933. [DOI] [PubMed] [Google Scholar]
- 13.Morrey BF. Complex instability of the elbow. Instr Course Lect. 1998;47:157–164. [PubMed] [Google Scholar]
- 14.Morrey BF. Functional evaluation of the elbow joint. In: Morrey BF, editor. The elbow and its disorders. Philadelphia: Saunders; 1993. pp. 16–52. [Google Scholar]
- 15.O’Driscoll SW, Jupiter JB, King GJ, Hotchkiss RN, Morrey BF. The unstable elbow. Instr Course Lect. 2001;50:89–102. [PubMed] [Google Scholar]
- 16.Potter HG. Imaging of the multiple-ligament-injured knee. Clin Sports Med. 2000;19:425–441. doi: 10.1016/S0278-5919(05)70216-7. [DOI] [PubMed] [Google Scholar]
- 17.Ring D, Jupiter JB. Compass hinge fixator for acute and chronic instability of the elbow. Oper Orthop Traumatol. 2005;17:143–157. doi: 10.1007/s00064-005-1126-2. [DOI] [PubMed] [Google Scholar]
- 18.Rodgers WB, Kharrazi FD, Waters PM, Kennedy JG, McKee MD, Lhowe DW. The use of osseous suture anchors in the treatment of severe, complicated elbow dislocations. Am J Orthop. 1996;25:794–798. [PubMed] [Google Scholar]
- 19.Sanchez-Sotelo J, Morrey BF, O’Driscoll SW. Ligamentous repair and reconstruction for posterolateral rotatory instability of the elbow. J Bone Joint Surg Br. 2005;87:54–61. [PubMed] [Google Scholar]
- 20.Sheps DM, Hildebrand KA, Boorman RS. Simple dislocations of the elbow: evaluation and treatment. Hand Clin. 2004;20:389–404. doi: 10.1016/j.hcl.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 21.Sotereanos DG, Darlis NA, Wright TW, Goitz RJ, King GJ. Unstable fracture-dislocations of the elbow. Instr Course Lect. 2007;56:369–376. [PubMed] [Google Scholar]
- 22.Tashjian RZ, Katarincic JA. Complex elbow instability. J Am Acad Orthop Surg. 2006;14:278–286. doi: 10.5435/00124635-200605000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Terada N, Yamada H, Seki T, Urabe T, Takayama S. The importance of reducing small fractures of the coronoid process in the treatment of unstable elbow dislocation. J Shoulder Elbow Surg. 2000;9:344–346. doi: 10.1067/mse.2000.106082. [DOI] [PubMed] [Google Scholar]
- 24.Twaddle BC, Bidwell TA, Chapman JR. Knee dislocations: where are the lesions? A prospective evaluation of surgical findings in 63 cases. J Orthop Trauma. 2003;17:198–202. doi: 10.1097/00005131-200303000-00008. [DOI] [PubMed] [Google Scholar]