Abstract
Myoelectric prostheses have generally been provided for adolescent or adult patients. The availability of smaller-sized electric hands has enabled the introduction of myoelectric prostheses to preschool children, mainly in the Scandinavian countries. This study evaluates the acceptance of myoelectric prostheses in 41 children with unilateral upper limb deficiency between the ages of two and five years. The prosthesis was used for an average time of 5.8 hours per day. The level of amputation was found to influence the acceptance rate. Furthermore, prosthetic use training by an occupational therapist is related to successful use of the prosthesis. The general drop-out rate in preschool children is very low compared to adults. Therefore, infants can profit from myoelectric hand prostheses. Since a correct indication and an intense training program significantly influence the acceptance rate, introduction of myoelectric prostheses to preschool children should take place at specialised centres with an interdisciplinary team.
Résumé
Les prothèses myoélectriques sont généralement prévues pour les adolescents ou les adultes. La mise à disposition de matériel de petite taille à permis l’utilisation de prothèses myoélectriques chez des enfants en age pré-scolaire. Cette étude évalue l’acceptation de telles prothèses chez 41 enfants de 2 à 5 ans avec un déficit unilatéral du membre supérieur. La prithèse était utilisée en moyenne 5,8 H par jour. Le niveau d’amputation influence le taux d’acceptation. De plus un apprentissage par un ergothérapeute est en relation avec le succés de l’utilisation de la prothèse. Le taux de rejet chez ces jeunes enfants est trés faible comparativement à ce qu’il est chez l’adulte. Sous réserve d’une correcte indication et d’un programme intense d’apprentissage les prothèses myoélectriques ont une place chez les enfants d’age pré-scolaire.
Introduction
Although upper extremity amputees are rare compared to lower extremity, the deficiency or loss of the upper limb is a far greater catastrophe for the individual and the family. The upper limb deficiency results in major restriction of function and cosmesis. In very young children upper limb deficiency is mainly caused by congenital transverse defect and these children are commonly seen in paediatric orthopaedic centres. Upper limb deficient children can be provided with three types of prosthesis. At first, children are usually advised to be fitted with a cosmetic passive device. These can be started when the children can sit in a stable position. A passive device trains the child to use both hands and supports the brain development. A passive prosthesis must be regarded as an extension of the residual limb. It should be involved in the child body image and, for example, swing naturally when walking and be placed spontaneously on the table when sitting. The next step in the management is an active device to be fitted when the child starts kindergarden (age three to five years). The grab device is opened by the contra lateral shoulder and can be formed like a hook or cosmetic hand. The progression to myoelectric prosthesis usually takes place at the age of ten or during early adolescence. When myoelectric prostheses were initially developed the size of the electrical and mechanical components was too large to fit into the forearm of a child. Fitting myoeletrically controlled hand prostheses to young children was considered unrealistic and even contraindicated.
The availability of smaller-sized electric hands in conjunction with technical improvements enabled the introduction of myoelectric prostheses for preschool children. In 1976, Sörbye started to fit myoelectric prostheses to very young children, the youngest being 16 months of age [14]. A very early myoelectric fitting can develop a body image with respect to the prosthesis and further development of the stump muscles can be achieved. Although applications of electrically powered prostheses in very young children have been reported by centres in Sweden, England, and Canada [2, 10, 14], this progress remained widely unnoticed in Germany. The rapid growth of children and the motor activity of a young child led to the opinion in German speaking countries that myoelectric prostheses should not be provided to children before the age of ten.
Many studies conducted over recent decades have looked at the influence of certain factors in the successful use of the upper limb prosthesis. Level of amputation, age, level of education, and training in prosthetic use have all been shown to be factors that influence prosthetic success [12, 13]. However, these studies all investigated adolescent and adult patients. There are no data available about prosthetic use in preschool children.
The aim of this retrospective study was to evaluate the acceptance of myoelectric prostheses in preschool children and to examine factors related to successful use of upper extremity prostheses.
Patients and methods
Forty-one consecutive children younger than six years at the time of prosthesis delivery were included in this retrospective study. All subjects suffered from a unilateral congenital upper limb transverse deficiency or traumatic upper limb amputation, but showed regular development of motor function. Patients with bilateral amputations, additional handicaps, or mental retardation were not included in this study. All patients were seen regularly by the authors. Table 1 presents anthropometrical data of the study group and details of amputation.
Table 1.
Anthropometric data of the study group (n = 41) and details of amputation
| Characteristic | Data | |
|---|---|---|
| Fitting age | 3.9 ± 1.1 y (mean ± SD) | Range 2.2–5.9 y |
| Sex | 22 female | 19 male |
| Affected body side | 14 right | 27 left |
| Level of amputation | 35 below elbow | Six above elbow |
| Causes of amputation | Five traumatic | 36 congenital |
According to our guidelines the majority of the children in the study group received a passive device at the age of approximately one year. Seven children were directly fitted with a myoelectric prosthesis due to recently sustained traumatic loss of the limb or due to a distal level of congenital amputation. A carpal level of amputation serves as a counter holder and, in our opinion, the fitting of a passive device doesn’t provide advantages in these cases. A body-powered mechanical device was used by one fourth of the patients before fitting of the electric powered prosthesis. To be fitted with a myoelectric prosthesis all patients had to fulfill the following inclusion criteria:
The child communicates well and follows instructions from strangers.
There is bi-manual handling and proactive interest in an artificial limb.
The family setting must support the child in using the myoelectric device.
The details of the myoelectric prosthesis were identical for all patients [11]. A socket was individually manufactured using the “Muenster” technique [11]. A single electrode was placed over the lateral aspect overlying the common finger and wrist extensor muscles or the triceps muscles for the group of children with higher level of deficiency [2]. The electrode controlled opening of the hand, while closing occurred automatically. The “Elektrohand 2000” (Otto Bock, Germany) was used and powered by a six volt rechargeable battery.
Initial introduction of the myoelectric prosthesis was either by specialised occupational therapists at the authors hospital (n = 32) or by outside therapists depending on the parents’ choice (n = 9). The statistical analysis showed no differences in the anthropometric data between these two subgroups. The initial one to two training weeks at the hospital involved the delivery of the prosthetic hand and a structured training program for the child and parents instructed by an interdisciplinary team.
A specially designed questionnaire was distributed to all families to receive information about acceptance and use of prosthetic devices during daily life (return rate 100%). The mean observation time between delivery of the prosthesis and receipt of the questionnaire was 2.0 years (0.7–5.1 years). The questions included information about internal or external occupational training and skin irritations at the stump. Use of the prosthesis for different activities of daily life was recorded in hours per day. Successful use of the prosthetic device was defined by a mean daily wearing time of more than two hours. The families were asked to rank the myoelectric prosthesis in regard to numerous parameters including weight, cosmetic appearance, function, and acceptance by strangers. In addition, the families gave suggestions to improve the prosthesis and the medical as well as technical attendance.
Statistical analysis was performed using the SPSS software package (SPSS Inc., Chicago, USA). Normal distribution of data was determined. Differences between subgroups were tested by the unpaired Student's t test or non-parametric testing for independent samples (Mann-Whitney U test). The level of statistical significance was set at P < 0.05. Data are presented as mean ± standard deviation unless otherwise stated.
Results
All children learned to open the prosthetic hand quickly, though some in a more controlled fashion than others (Fig. 1).
Fig. 1.

Use of the myoelectric powered prosthesis by a four-year-old girl
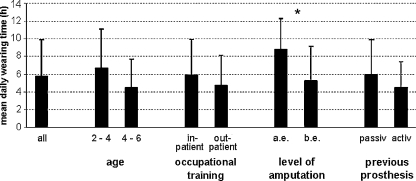
During the mean observation time of 2.0 ± 1.3 years, 76% of the study group appeared to be successfully using the prosthetic device. The actual mean time of daily use was 5.8 ± 4.1 hours per day (range, 0–14 hours). Children fitted between two and four years of age (n = 23) showed a higher average time of daily use compared to the older subgroup (four to six years [n = 18]), although the level of significance was not reached (Fig. 2). A tendency towards a higher daily use was observed in those who completed the intensive occupational training at the hospital. The level of amputation significantly influences the daily wearing time (p = 0.04). Above elbow amputees, although low in number, demonstrated a higher wearing time than children with below elbow amputations. Three out of five patients with amputations at or below the wrist denied use of any prosthetic device. Children who had a body-powered active device prior to myoelectric prosthesis show a tendency towards higher wearing time compared to patients with a passive device only (Fig. 2). Frequent skin irritation was associated with a trend to a higher daily wearing time.
Fig. 2.
Mean daily wearing time (mean ± SD) of myoelectric prosthesis in the study group (n = 41) and different subgroups arranged by age, occupational training, level of amputation, and the prosthetic device used prior to fitting of the myoelectric prosthesis. The differences between the subgroups did not reach the level of significance except for level of amputation. *p < 0.05, a.e. above elbow, b.e. below elbow
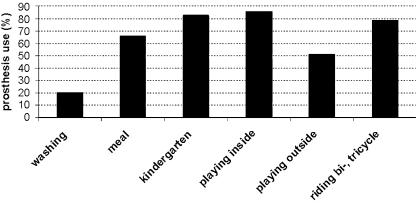
The myoelectric prosthesis was preferentially used for playing and in the kindergarten, and half of the study group preferred not to use the prosthesis playing outside (Fig. 3). During the observation period the prostheses of 33 out of 41 patients were temporarily unusable for reasons such as technical failure, breakdown, or problems with fitting. The mean frequency of maintenance was 1.9 ± 2.6 per year, ranging from zero to eight repairs. The number of repairs correlated positively with the daily wearing time (r = 0.67, p = 0.01).
Fig. 3.
Percentage of children using the prosthesis during activities of daily living
The families were asked to grade the prosthesis with regard to different aspects such as function, weight, or appearance (Table 2). Overall, the families were satisfied with the appearance and function of the prosthesis, whereas the susceptibility for breakdown and the weight of the prosthesis were rated less than good. There was consensus that the battery life span was too short.
Table 2.
The families valued different aspects of the prosthesis similar to school grades: 1 very good/important to 5 poor/insufficient
| Aspect | Assessment |
|---|---|
| Acceptance by other children | 1.4 ± 0.5 |
| Appearance | 1.6 ± 0.9 |
| Acceptance by other adults | 1.7 ± 0.7 |
| Function | 1.9 ± 0.6 |
| Weight | 2.4 ± 1.1 |
| Susceptibility to breakdown | 2.4 ± 1.3 |
Discussion
This study retrospectively evaluated the fitting of myoelectric prostheses in 41 consecutive preschool children with unilateral upper limb deficiency. A myoelectric prosthesis is able to combine the cosmetic demands of physical integrity by society and the family with the functional need for bimanual handling of the child.
The relatively large number of subjects included in this survey compared to previous studies [2, 14] is related to the experience of our centre with handicapped children. A multidisciplinary rehabilitation team consisting of paediatric orthopaedic surgeons, prosthetists (engineers), and occupational therapists accompanies the family during the rehabilitation program. When the prosthesis was fitted to the child, occupational therapists taught the use of the prosthesis during play and activities of everyday life appropriate to the age group, taking into account the individual degree of maturation and interest of the child [7]. The occupational therapy aims for the child to discover the abilities as well as the boundaries of the prosthesis in order to achieve bimanual handling and age-appropriate independence [6]. The mother or father was involved in practical aspects of putting the limb on, coping with battery changing, and encouragement of the child to the use the powered hand during the training programme. The importance of the professional prosthesis training may be reflected by the tendency towards longer daily wearing time in children who completed the in-patient occupational therapy programme. During the hospital stay the powered hand became the central point, and the child’s attention is focussed solely on the new situation. Although costs of the hospital stay are high and can be problematic due to cost restraints of health insurance, the advantages of the initial training week seem to be obvious and should be taken into account when myoelectric devices are fitted to young children. The relevance of occupational training during fitting of myoelectric prostheses in young children is well documented in the literature [6, 7, 14].
Successful use of the myoelectric prosthesis was deduced from the mean daily wearing time. In contrast to other publications [9, 13], the criteria for successful use (>2 h/day) in this study were found to be high, and low part-time use was still classified as rejection of the prosthesis. In this study, 24% of the subjects were categorised as rejecters of the myoelectric device. These patients preferred to wear a body-controlled split hook or declined to use a prosthetic device at all, including two patients with traumatic hand amputations below the wrist. In comparison with other data in the literature, our success rate is similar to other studies (Table 3). This also indicates that the success rate seems to be independent of age.
Table 3.
Literature review including percentages of upper limb deficient patients with successful use of myoelectric prosthesis
The mean daily wearing time in children with above-elbow amputations was higher than in patients with below-elbow amputations. The acceptance rate is influenced by the level of amputation [4, 5]. Individuals with a high level of amputation seem to avail themselves more of the prosthetic device than patients with a longer stump.
It appears to be an attractive option to switch to electrically-powered prosthetic hands for preschool children. Technical problems have already been overcome due to the current availability of very small-sized electric hands. Another concern regarding the myoelectric hand is the questionable cognitive and motor capacities of preschool children. The outcome of this study indicates that the use of the myoelectric prosthesis is not related to the age of the child. Most of our patients demonstrate developmental readiness to participate in the training program for myoelectric prosthesis as early as two years of age. In contrast to orthopaedic text books, age does not seem to be a contraindication for the use of a myoelectric prosthesis.
As opposed to age, the more important selection criteria seem to be activity and the temperament of the child. A calm child interested in doing handicrafts or similar playing activities is reliant on bimanual handling. Improved cosmesis, reduction of harness, improved grip force, and ability to work close to the body in various planes are advantages provided by the myoelectric prosthesis. In contrast, body-powered prostheses are more durable for playing outside with sand and water or sports such as soccer. A very active child might profit from a more robust prosthetic device such as the body-powered grippers. The introduction of a powered prosthesis at an earlier age can be a more suitable alternative than providing a body-powered prosthetic device and waiting to reach on older age when a myoelectric prosthesis is considered.
One of the keys to success seems to be the involvement of the family. The electrically powered prostheses are very much liked by the parents and therefore parental support is usually guaranteed. It is possible that parental contribution may have decreased rejection rates or very poor use.
Under appropriate conditions the application of a myoelectric hand prosthesis in a young child can be very successful. One should, however, be aware that no child can be expected to continuously be a clever prosthetic user or an all-day wearer. The needs of the child regarding the artificial limb and therefore the wearing patterns change during growth. A preschool child demonstrates different demands than the school boy with high sport activities or the teenaged adolescent who may temporally reject all prosthetic devices. The children should be trained in a suitable way to be well prepared for their own choice later and for the best possible use of the prosthesis as an adult.
To achieve sustained success of a prosthetic and rehabilitation program, in our opinion, the most important points are as follows:
Fitting of the myoelectric prosthesis from a specialist centre
Management by a multidisciplinary team including paediatric orthopaedics, occupational therapists, and specialist technicians
An initial training week
Regular monitoring to assess the use of the artificial limb and to respond when the child's needs are changing
Continuing support to provide prompt and efficient maintenance or repair
Due to the poor of durability of the myoelectric hand as well as the changing needs of the child during growth and development, we tend to provide a variety of prosthetic options including passive devices, myoelectric hands, and body-powered hooks to the child. The paediatric amputees may choose multiple prostheses on the basis of function and situation. The child changes the prostheses during the day and is able to wear an artificial limb based on the situation. Positive experiences offered by a variety of prosthetic options to help with normal activities of daily living have been reported by several authors [1, 3, 8, 9]. Crandall et al. reported that 41% of the patients continued as multiple users in the long-term follow-up [1], but the impact of this prosthesis supply on costs and reduction in maintenance frequency need to be evaluated in future studies.
References
- 1.Crandall RC, Tomhave W. Pediatric unilateral below-elbow amputees: retrospective analysis of 34 patients given multiple prosthetic options. J Pediatr Orthop. 2002;22:380–383. doi: 10.1097/00004694-200205000-00023. [DOI] [PubMed] [Google Scholar]
- 2.Datta D, Ibbotson V. Powered prosthetic hands in very young children. Prosthet Orthot Int. 1998;22:150–154. doi: 10.3109/03093649809164477. [DOI] [PubMed] [Google Scholar]
- 3.Gaine WJ, Smart C, Bransby-Zachary M. Upper limb traumatic amputees. Review of prosthetic use. J Hand Surg [Br] 1997;22:73–76. doi: 10.1016/s0266-7681(97)80023-x. [DOI] [PubMed] [Google Scholar]
- 4.Glynn MK, Galway HR, Hunter G, Sauter WF (1986) Management of the upper-limb-deficient child with a powered prosthetic device. Clin Orthop:202–205 [PubMed]
- 5.Heger H, Millstein S, Hunter GA. Electrically powered prostheses for the adult with an upper limb amputation. J Bone Joint Surg Br. 1985;67:278–281. doi: 10.1302/0301-620X.67B2.3980541. [DOI] [PubMed] [Google Scholar]
- 6.Hermansson LM. Structured training of children fitted with myoelectric prostheses. Prosthet Orthot Int. 1991;15:88–92. doi: 10.3109/03093649109164639. [DOI] [PubMed] [Google Scholar]
- 7.Hubbard S, Galway HR, Milner M. Myoelectric training methods for the preschool child with congenital below-elbow amputation. A comparison of two training programmes. J Bone Joint Surg Br. 1985;67:273–277. doi: 10.1302/0301-620X.67B2.3980540. [DOI] [PubMed] [Google Scholar]
- 8.Kritter AE. Myoelectric prostheses. J Bone Joint Surg Am. 1985;67:654–657. [PubMed] [Google Scholar]
- 9.Kruger LM, Fishman S. Myoelectric and body-powered prostheses. J Pediatr Orthop. 1993;13:68–75. doi: 10.1097/01241398-199301000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Mendez MA. Evaluation of a myoelectric hand prosthesis for children with a below-elbow absence. Prosthet Orthot Int. 1985;9:137–140. doi: 10.3109/03093648509164725. [DOI] [PubMed] [Google Scholar]
- 11.Nader M (1990) The artificial substitution of missing hands with myoelectrical prostheses. Clin Orthop:9–17 [PubMed]
- 12.Roeschlein RA, Domholdt E. Factors related to successful upper extremity prosthetic use. Prosthet Orthot Int. 1989;13:14–18. doi: 10.3109/03093648909079404. [DOI] [PubMed] [Google Scholar]
- 13.Silcox DH, III, Rooks MD, Vogel RR, Fleming LL. Myoelectric prostheses. A long-term follow-up and a study of the use of alternate prostheses. J Bone Joint Surg Am. 1993;75:1781–1789. doi: 10.2106/00004623-199312000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Sorbye R (1980) Myoelectric prosthetic fitting in young children. Clin Orthop:34–40 [PubMed]