Abstract
The concept of a dual articulation acetabular cup was developed by Prof. Bousquet in 1974. This concept has been shown to provide high stability after revision and primary total hip arthroplasty. The aim of our study was to evaluate the incidence of prosthetic instability in a consecutive homogeneous series of 384 primary dual mobility cups. Incidence of instability and implant survival were evaluated. Mean follow-up was 15.3 years (range, 12–20). There was no early or late instability. On the acetabular side there were 13 aseptic loosenings, 14 intraprosthetic dislocations, and seven polyethylene wear cases that required replacement of the liner. The cumulative survival rate of the dual-articulation acetabular cup using surgical revision for aseptic loosening as the endpoint was 95.9% ± 4.1% at 18 years postoperatively. Our series proves the good long term behaviour of dual-articulation acetabular components in primary arthroplasty. Their excellent survivorship rate and the absence of episodes of prosthetic instability increase our confidence in this concept.
Résumé
Le concept de cupule à double mobilité a été inventé par le Professeur Gilles BOUSQUET en 1974. Ce concept a permis de mettre en évidence une importante stabilité des hanches, notamment après révision mais également dans les prothèses totales de hanches de première intention. Le but de cette étude est d’évaluer l’incidence et l’instabilité sur une série homogène consécutive de 384 hanches traitées avec cupule à double mobilité. Le taux d’instabilité des implants sur les patients survivants a été évalué. Le suivi moyen a été de 15,3 ans (de 12 à 20 ans) au plus long recul, il n’y a aucune instabilité ni primaire, ni tardive. Par contre, il existe 13 descellements aseptiques acétabulaires, 14 luxations intra prothétiques, 7 usures du polyéthylène qui ont nécessité un remplacement du PE. Le taux de survie cumulé de cette cupule à double mobilité est de 95,9% ± à 18 ans si l’on prend comme critère la révision pour descellement aseptique. Cette série prouve le bon devenir à long terme de cette articulation dans les prothèses totales primaires, avec un excellent taux de survie et l’absence de phénomènes de luxation inhérentes à ce concept.
Introduction
Implant instability is a major complication of total hip arthroplasty. Early dislocation rates after total hip arthroplasty vary between series, but they are generally around 2–3% [3, 7, 23]. Dislocation rates significantly increase in the long run; rates of 4.8% at ten-year follow-up and 7% at 25 years have been reported in the large Mayo Clinic’s series [3]. Many factors may affect the stability of a total hip prosthesis including: orientation of the components [12], surgical approach [23], patient-related factors (i.e. gender [9], age [17], neurological disorders), component geometry, and more particularly, head diameter and head–neck ratio.
Biomechanical studies showed that instability could be addressed by increasing the diameter of the head [5]. As a matter of fact, the larger the head diameter, the higher is the head–neck ratio and lower is the potential for instability. Many studies report lower instability rates with 28 mm and 32 mm diameter heads [16].
The concept of dual articulation invented by Prof. Bousquet in 1974 is now increasingly recognised in Europe. One can even find publications in the English literature, but implant designations and descriptions are different (e.g. “unconstrained tripolar cup” by Guyen et al. [14], “dual mobility sockets” by other authors [11, 21], and "mobile bearing” by other manufacturers). This concept has been shown to provide high stability after revision total hip arthroplasty and to successfully address chronic instability after total hip arthroplasty [14]. Implanting a dual-articulation acetabular cup is like using a large head; it reduces the postoperative instability.
We have been routinely using dual-articulation acetabular cups in primary cases since the 1980s; thus, we now have long-term experience with this concept [11, 21].
The aim of our study was to evaluate the incidence of prosthetic instability in a consecutive homogeneous series of 384 primary cases with a mean follow-up of 15 years.
Patients and methods
The initial dual-articulation acetabular cup system was designed by Prof. Gilles Bousquet and André Rambert (engineer) in 1974.
The three main goals of these dual-articulation implants were to decrease wear, restore near-normal range of motion, and increase implant stability.
This concept is an ingenious combination of the Charnley’s low friction principle using a 22.2 mm diameter head that articulates against polyethylene to decrease wear and the McKee-Farrar theory using a large-diameter polyethylene liner that articulates against a metal shell (in the same way as a large head) to enhance implant stability.
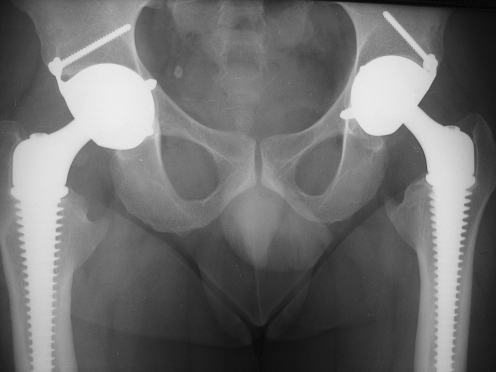
The dual-articulation acetabular cup system consists of a cementless stainless steel or titanium acetabular shell and a polyethylene liner which freely rotates within the shell and positively captures the prosthetic head. Thus, there are two distinct articulations sharing the same motion centre: a small articulation between the 22.2 mm metal head and the polyethylene liner, and a large articulation between the polyethylene liner and the metal shell (see Fig. 1). The initial NOVAE shell was a stainless steel shell with a porous plasma sprayed alumina (AL2O3) coating and a cylindrical/spherical geometry. Some shells were machined from TA6V4 titanium alloy, with the same porous AL2O3 alumina coating. The shell was implanted without cement. Press-fit fixation was supplemented by a three-point fixation system consisting of two morse taper pegs impacted into the ischium and the ischiopubic ramus respectively, and one 4.5 mm screw inserted bicortically into the ilium at 45° to the sagittal plane. This three-point fixation system was designed to resist rotation and pull-out forces and provide adequate primary fixation.
Fig. 1.
Double mobility acetabular cup system
The mobile liner was made of ultra-high molecular weight polyethylene (UHMWPE) sterilised by gamma irradiation in air. It was 5/8 of a sphere and articulated both with the femoral head and the metal shell. It was highly retentive; the femoral head had to be forced into the liner by impaction. All femoral heads were 22.2 mm in diameter.
All implantations were performed in a single orthopaedic centre, constituting a consecutive and homogeneous series of cases, i.e. the same acetabular component and same surgical indication. Only primary cases were included in the study; revision cases and total hip arthroplasties performed for treatment of fractures were excluded. A total of 384 total hip arthroplasties were analysed. On the femoral side, there were 160 PF stainless steel threaded stems (Serf, Décines, France) and 224 PRO titanium threaded stems (Serf, Décines, France). On the acetabular side, there were 79 NOVAE-1 titanium acetabular components (Serf, Décines, France) and 305 NOVAE-1 stainless steel acetabular components (Serf, Décines, France). All femoral heads were 22.2 mm cobalt–chromium or stainless steel heads.
Mean follow-up was 15.3 years (range, 12–20). Mean age at the time of surgery was 55.8 years (range, 23–87). The series consisted of 198 female and 186 male patients. According to the Charnley classification, there were 344 A, 26 B, and 14 C patients.
Aetiologies included 194 primary osteoarthritis (50.1%), 91 osteoarthritis in dysplastic hip (23.7%), 48 aseptic necrosis of the femoral head (12.6%), eight sequelae of acetabular fracture (2%), and 43 secondary osteoarthritis (11.1%).
All patients were clinically followed-up using the Merle d’Aubigné–Postel clinical rating system [20]. Antero–posterior and lateral X-rays were taken at two to three-year intervals for radiographic evaluation (see Fig. 2). A final evaluation was performed at the last follow-up.
Fig. 2.
Antero–posterior radiograph of pelvis 15 years postoperative
Osteolysis was radiologically assessed by the presence of granuloma in the Gruen [13] zones for the femur, and in the De Lee and Charnley zones for the acetabulum [10]. Heterotopic ossification was evaluated at the last follow-up and classified according to Brooker.
Failures were analysed based on the operation reports, intraoperative findings, and analysis of retrieved implants.
Implant survival was evaluated at the last follow-up using the actuarial method, with surgical revision for aseptic loosening as the endpoint. The standard error, given as a percentage, and the 95% confidence intervals were calculated from the data in the life table. Statistical analysis was performed using nonparametric tests. Significance was determined with StatView statistical software (version 5.0; SAS Institute, Cary, North Carolina) and was defined as a p value of <0.05.
We evaluated the incidence of instability at the last follow-up by prospectively listing all the episodes of implant instability.
Results
At the last follow-up, six patients (1.4%) could not be located and 92 (24%) had died (with their prosthesis still functioning at the time of death). The Merle d’Aubigné–Postel clinical score was 16.3, versus 6.4 preoperatively. There was no early or late instability.
Femoral complications included early PRO and PF stem unscrewing in nine cases and severe varus shift of the PRO stem after seven years in one case. Radiographic findings revealed 35 severe calcar resorbtions and 17 granuloma confined to zones I or VII. However, granuloma remained asymptomatic in all of the cases and did not require surgical revision of the femoral component.
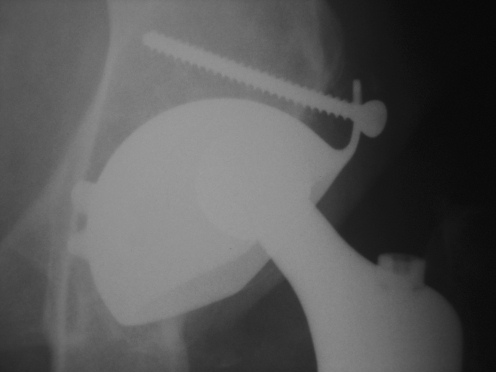
On the acetabular side, 15 minor lucencies were observed. On the same side, late complications occurred, including 13 aseptic loosening cases (3.3%), 14 intraprosthetic dislocations (3.6%), and seven instances of polyethylene wear that required replacement of the liner (1.8%). Mean time to intraprosthetic dislocation was 8.9 years [4–16]. Based on the clinical and radiological data and on analysis of the retrieved implants, we determined that two of the intraprosthetic dislocations were associated with loosening of the acetabular component (see Fig. 3), three with fibrosis (see Fig. 4), and nine were pure intraprosthetic dislocations. Interestingly, the intraprosthetic dislocations that resulted from jamming of the second articulation due to fibrosis occurred earlier than in the other two subgroups (p < 0.001). This complication is specific to dual-articulation cups. Its occurrence rate was 2% at ten years and 3% at 15 years.
Fig. 3.
Aspect of the acetabular cup system after intraprosthetic dislocation. In this case the intraprosthetic dislocation is associated with loosening of the acetabular component
Fig. 4.
Radiograph of an intraprosthetic dislocation due to fibrosis at six-year follow-up
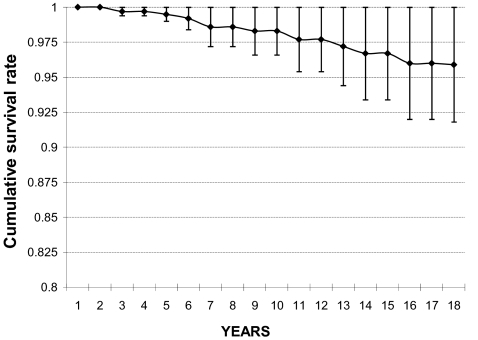
Survival of the dual-articulation acetabular cups was analysed using the actuarial method, with surgical revision for aseptic loosening as the endpoint. The cumulative survival rate was 96.7%±3.3% (95% confidence interval, 94.6–98.8%) at 15 years and 95.9%±4.1%(95% confidence interval, 93.5–98.2%) at 18 years postoperatively (see Fig. 5).
Fig. 5.
Cumulative survival rate of dual-articulation acetabular cup using surgical revision for aseptic loosening as the end point
Discussion
At the last follow-up, none of the 384 total hip arthroplasties showed signs of instability, which confirms the superior stability of dual-articulation designs in the long run.
Chandler et al. [7] analysed 20 published series, which represented a total of 10,376 total hip arthroplasties, and reported an overall early instability rate of 2.7%. Woo and Morrey [23] reported a rate of 3.2%. However, these figures were obtained at three to four months postoperatively, when soft-tissue healing was complete. But instability rate increases with time, and unfortunately, while there are a wealth of studies about the early prosthetic dislocation rate, long-term studies are scarce. Berry et al. [3] analysed a few Mayo Clinic series and reported late prosthetic instability rates as high as 10%.
Furthermore, it is interesting to examine the factors which influence instability. The factors influencing early instability are essentially related to the patient’s condition. Woolson and Rahimtoola [24] showed that disorders of the mental capacity can promote postoperative instability. Tarasevicius et al. [22] reported a 10% dislocation rate within the first 12 months following surgery in a series of patients treated for femoral neck fractures. Levy et al. [17] reported rates up to 20% in patients over 80 years old. Coventry [9] found a male to female ratio of four to one in dislocation rates. Technical factors also can influence early instability. Lewinnek et al. [18] found a correlation between the incidence of anterior dislocation and an excessive cup anteversion (more than 35°). Biderman et al. [4] found a correlation between the incidence of posterior dislocation and a low anteversion angle. These data are fully consistent with the results reported by all the studies that investigated the correlation between implant malposition and instability rate [12]. Posterior approaches were often accused of being responsible for posterior instability. However, many authors proved that this approach had no direct influence on early postoperative instability rates, but that it did adversely affect these rates in the presence of associated factors such as component malposition or small heads [15].
Late instability factors have been described by Coventry [9]. The main factors are muscle weakening, onset of disorders of mental capacity, cup distortion due to repeated dislocations, and wear. It is a combination of all these factors that promotes late instability. Two major instability mechanisms have been identified: lift-off and cam effect. In both cases, the dislocation risk is primarily related to the diameter of the femoral head and the inclination of the cup. This risk can be determined using the formula:  where R is the radius of the prosthetic head, and AB the distance the head must displace before dislocation occurs. The principle of dual articulation is pretty similar to the McKee concept where a large-diameter head is used to decrease the potential for instability. For the same inclination angle, the distance AB for a 46 mm head (DUROM, Zimmer, UK) is 24 mm and for a 53 mm dual-articulation cup, it is 27.2 mm. The effective diameter of the femoral head is the outer diameter of the polyethylene mobile component. Therefore, it is easy to understand why 32 mm and 36 mm heads provide slightly less stability than dual-articulation acetabular components. This is confirmed by the results reported in the published series, with an average 1% early dislocation rate in implants with large heads [16]. This means that these implants are less effective in preventing postoperative dislocation than dual-articulation acetabular components. Furthermore, in metal/polyethylene bearings, larger heads result in higher volumetric wear than 22.2 mm heads. This may cause foreign body reactions which have been shown to be responsible for a large number of component loosenings due to osteolysis [19]. Adam et al. evaluated wear in dual-articulation acetabular components and showed that volumetric wear was similar to that in Charnley hips [1]. Therefore, one can say that dual-articulation cups provide better stability than large heads while minimising volumetric wear and, as a result, polyethylene debris.
where R is the radius of the prosthetic head, and AB the distance the head must displace before dislocation occurs. The principle of dual articulation is pretty similar to the McKee concept where a large-diameter head is used to decrease the potential for instability. For the same inclination angle, the distance AB for a 46 mm head (DUROM, Zimmer, UK) is 24 mm and for a 53 mm dual-articulation cup, it is 27.2 mm. The effective diameter of the femoral head is the outer diameter of the polyethylene mobile component. Therefore, it is easy to understand why 32 mm and 36 mm heads provide slightly less stability than dual-articulation acetabular components. This is confirmed by the results reported in the published series, with an average 1% early dislocation rate in implants with large heads [16]. This means that these implants are less effective in preventing postoperative dislocation than dual-articulation acetabular components. Furthermore, in metal/polyethylene bearings, larger heads result in higher volumetric wear than 22.2 mm heads. This may cause foreign body reactions which have been shown to be responsible for a large number of component loosenings due to osteolysis [19]. Adam et al. evaluated wear in dual-articulation acetabular components and showed that volumetric wear was similar to that in Charnley hips [1]. Therefore, one can say that dual-articulation cups provide better stability than large heads while minimising volumetric wear and, as a result, polyethylene debris.
The tripolar acetabular cups are included in this category of implants because they have the same design rationale, that is, increase the diameter of the prosthetic head in order to decrease the potential for dislocation [6]. However, the episodes of postoperative instability reported in the published series suggest that the concept of dual articulation is much more effective in preventing dislocation than the “tripolar” concept. Cooke et al. are very critical towards this concept. They argue that polyethylene is too thin, and, more importantly, that the increased number of interfaces leads to high instability rates in the medium and long run [8].
Lastly, another type of constrained acetabular component has been developed, which aims to decrease instability by positively capturing the prosthetic head [2]. As far as prevention of instability is concerned, the goal is achieved. However, the significant increase in stresses at the interfaces jeopardises long-term fixation, which is the major drawback of this concept [25]. Therefore, the long-term survival of these constrained implants cannot compare with that of dual-articulation cups, which is 96.7% at 15 years.
The above shows that the concept of dual articulation fully meets long-term stability requirements. As regards fixation, the survivorship rates at 15 years fall within the average range. Therefore, this implant can be considered a first-choice option in all the primary cases where postoperative stability is the main concern (i.e. elderly patients, relatively young and active patients who need high range of motion).
However, wear has been found to occur at the liner/head interface. It decreases the retaining power of the polyethylene liner, results in dislocation of the small articulation (i.e. polyethylene liner/prosthetic head), and causes the prosthetic head to come into contact with the metal shell. This phenomenon is known as “intraprosthetic dislocation” [11, 21] and is enhanced by a number of factors including young age of the patient, design and material of the stem neck, and formation of periprosthetic fibrosis which may be associated with a cam effect. This complication is very infrequent; its occurrence is only 2–3% at 15 years [21]. Surgery is the only treatment option, consisting of replacement of the polyethylene liner, but it is a very straightforward procedure if performed at an early stage. This complication may be compared to late instability due to wear. In our series, such complications were seen in 2% at ten years and 3% at 15 years, which is much lower than the late instability rates reported by Berry in Charnley hips [3].
Conclusion
Our consecutive homogeneous series proves the good long-term behaviour of dual-articulation acetabular components in primary arthroplasty. Their excellent survivorship rate at 18 years increases our confidence in this concept. The initial goal of this cup was to decrease the postoperative dislocation rate. Considering the absence of episodes of prosthetic instability in our series, we can rightly claim that this goal has been achieved. Intraprosthetic dislocation due to wear at the liner–head interface is the main, although infrequent, issue (only 3% at 15 years) in dual-articulation acetabular cups.
These findings led us to slightly modify our indications. Thus, in patients below 65 years of age, we routinely use alumina-on-alumina bearings to minimise the long-term wear, but where there is a high risk of postoperative instability, we recommend a dual-articulation acetabular component; in patients older than 65 years, we systematically use a dual-articulation cup.
References
- 1.Adam P, Farizon F, Fessy MH. Dual articulation retentive acetabular liners and wear: surface analysis of 40 retrieved polyethylene implants. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:627–636. doi: 10.1016/s0035-1040(05)84466-6. [DOI] [PubMed] [Google Scholar]
- 2.Anderson MJ, Murray WR, Skinner HB. Constrained acetabular components. J Arthroplasty. 1994;9:17–23. doi: 10.1016/0883-5403(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ, Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86-A:9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stockl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005;87:762–769. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 5.Burroughs BR, Rubash HE, Harris WH (2002) Femoral head sizes larger than 32 mm against highly cross-linked polyethylene. Clin Orthop Relat Res 150–157 [DOI] [PubMed]
- 6.Callaghan JJ, O’Rourke MR, Goetz DD, Lewallen DG, Johnston RC, Capello WN (2004) Use of a constrained tripolar acetabular liner to treat intraoperative instability and postoperative dislocation after total hip arthroplasty: a review of our experience. Clin Orthop Relat Res 117–123 [DOI] [PubMed]
- 7.Chandler RW, Dorr LD, Perry J (1982) The functional cost of dislocation following total hip arthroplasty. Clin Orthop Relat Res 168–172 [PubMed]
- 8.Cooke CC, Hozack W, Lavernia C, Sharkey P, Shastri S, Rothman RH. Early failure mechanisms of constrained tripolar acetabular sockets used in revision total hip arthroplasty. J Arthroplasty. 2003;18:827–833. doi: 10.1016/S0883-5403(03)00325-5. [DOI] [PubMed] [Google Scholar]
- 9.Coventry MB. Late dislocations in patients with Charnley total hip arthroplasty. J Bone Joint Surg Am. 1985;67:832–841. [PubMed] [Google Scholar]
- 10.DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 20–32 [PubMed]
- 11.Farizon F, Lavison R, Azoulai JJ, Bousquet G. Results with a cementless alumina-coated cup with dual mobility. A twelve-year follow-up study. Int Orthop. 1998;22:219–224. doi: 10.1007/s002640050246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goergen TG, Resnick D. Evaluation of acetabular anteversion following total hip arthroplasty: necessity of proper centring. Br J Radiol. 1975;48:259–260. doi: 10.1259/0007-1285-48-568-259. [DOI] [PubMed] [Google Scholar]
- 13.Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 17–27 [PubMed]
- 14.Guyen O, Chen QS, Bejui-Hugues J, Berry DJ, An KN. Unconstrained tripolar hip implants: effect on hip stability. Clin Orthop Relat Res. 2007;455:202–208. doi: 10.1097/01.blo.0000238796.59596.1f. [DOI] [PubMed] [Google Scholar]
- 15.Kavanagh BF, Ilstrup DM, Fitzgerald RH., Jr Revision total hip arthroplasty. J Bone Joint Surg Am. 1985;67:517–526. [PubMed] [Google Scholar]
- 16.Kelley SS, Lachiewicz PF, Hickman JM, Paterno SM (1998) Relationship of femoral head and acetabular size to the prevalence of dislocation. Clin Orthop Relat Res 163–170 [DOI] [PubMed]
- 17.Levy RN, Levy CM, Snyder J, Digiovanni J (1995) Outcome and long-term results following total hip replacement in elderly patients. Clin Orthop Relat Res 25–30 [PubMed]
- 18.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 19.Livermore J, Ilstrup D, Morrey B. Effect of femoral head size on wear of the polyethylene acetabular component. J Bone Joint Surg Am. 1990;72:518–528. [PubMed] [Google Scholar]
- 20.Merle d’Aubigné R. Cotation chiffrée de la fonction de hanche. Rev Chir Orthop Reparatrice Appar Mot. 1970;56:481–486. [PubMed] [Google Scholar]
- 21.Philippot R, Adam P, Farizon F, Fessy MH, Bousquet G. Survival of cementless dual mobility sockets: ten-year follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2006;92:326–331. doi: 10.1016/s0035-1040(06)75762-2. [DOI] [PubMed] [Google Scholar]
- 22.Tarasevicius S, Jermolajevas V, Tarasevicius R, Zegunis V, Smailys A, Kalesinskas RJ. Total hip replacement for the treatment of femoral neck fractures. Long-term results. Medicina (Kaunas) 2005;41:465–469. [PubMed] [Google Scholar]
- 23.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 24.Woolson ST, Rahimtoola ZO. Risk factors for dislocation during the first 3 months after primary total hip replacement. J Arthroplasty. 1999;14:662–668. doi: 10.1016/S0883-5403(99)90219-X. [DOI] [PubMed] [Google Scholar]
- 25.Yun AG, Padgett D, Pellicci P, Dorr LD. Constrained acetabular liners: mechanisms of failure. J Arthroplasty. 2005;20:536–541. doi: 10.1016/j.arth.2004.12.054. [DOI] [PubMed] [Google Scholar]