Abstract
Objective
The precise intra- vs. extradural localization of aneurysms involving the paraclinoid internal carotid artery is critical for the evaluation of patients being considered for aneurysm surgery. The purpose of this study was to investigate the clinical usefulness of T2-weighted three-dimensional (3-D) fast spin-echo (FSE) magnetic resonance (MR) imaging in the evaluation of unruptured paraclinoid aneurysms.
Methods
Twenty-eight patients with unruptured cerebral aneurysms in their paraclinoid regions were prospectively evaluated using a T2-weighted 3-D FSE MR imaging technique with oblique coronal sections. The MR images were assessed for the location of the cerebral aneurysm in relation to the dural ring and other surrounding anatomic compartments, and were also compared with the surgical or angiographic findings.
Results
All 28 aneurysms were identified by T2-weighted 3D FSE MR imaging, which showed the precise anatomic relationships in regards to the subarachnoid space and the surrounding anatomic structures. Consequently, 13 aneurysms were determined to be intradural and the other 15 were deemed extradural as they were confined to the cavernous sinus. Of the 13 aneurysms with intradural locations, three superior hypophyseal artery aneurysms were found to be situated intradurally upon operation.
Conclusion
High-resolution T2-weighted 3-D FSE MR imaging is capable of confirming whether a cerebral aneurysm at the paraclinoid region is intradural or extradural, because of the MR imaging's high spatial resolution. The images may help in identifying patients with intradural aneurysms who require treatment, and they also can provide valuable information in the treatment plan for paraclinoid aneurysms.
Keywords: Dural ring, Internal carotid artery, Magnetic resonance imaging, Paraclinoid aneurysms
INTRODUCTION
The natural history of aneurysms involving the paraclinoid area varies based on their anatomic locations and hence the precise localization by neuroimaging study in preoperative period has been one of the most interesting and important problems in clinical neurosurgery4,7,11,18,24,25). Aneurysms identified as being completely intradural are at risk for subarachnoid hemorrhage (SAH), and usually require preventive endovascular or surgical treatment. However, aneurysms located completely below the distal dural ring cannot cause SAH, and they have lower morbidity than aneurysms arising from the intradural space.
Preoperative delineation of the distal dural ring and exact localization of the aneurysm in relation to the cavernous sinus structures continue to be critical clinical issues, but catheter angiography or other conventional imaging modalities have failed to localize these aneurysms exactly10,11,18). As a result of recent advances in magnetic resonance (MR) technology, T2-weighted three-dimensional (3-D) fast spin-echo (FSE) MR imaging allows for an easy examination of the brain using thin sections and a high signal-to-noise ratio (SNR)16,19,21,27). T2-weighted 3-D FSE MR imagings are characterized by a high vascular contrast created by a high signal from surrounding cerebrospinal fluid, a moderate signal from adjacent brain structures, and a signal void of the vessel. Based on these characteristics, we have proposed that the MR images may also be helpful for the evaluation of intracranial aneurysms involving the paraclinoid internal carotid artery (ICA).
Over the years, aneurysms of the proximal ICA have been placed under different classifications by various authors because the anatomy is complex in the area where the ICA enters the intradural space through the dura mater2,5,9). In this study we will call the penetrating segment of the ICA the "paraclinoid ICA", which includes the C4 (cavernous), C5 (clinoid) and C6 (ophthalmic) segments of the ICA, as described by Bouthillier2).
The purpose of this study was to evaluate the efficacy of T2-weighted 3-D FSE MR imaging in the differentiation of intradural and extradural aneurysms involving the paraclinoid ICA.
MATERIALS AND METHODS
Patients selection
Between July 2007 and June 2008, unruptured aneurysms of the paraclinoid segment of the ICA in 28 patients, consisting of 7 male and 21 female patients with ages ranging from 25 to 74 years (mean age, 53 years), were prospectively evaluated with the targeted T2-weighted 3-D FSE MR imaging. All aneurysms were incidentally identified in various ways. Three aneurysms were identified during the preoperative evaluation of SAH due to rupture of intracranial aneurysms at another location, two during the preoperative angiographic evaluation of meningioma and arteriovenous malformation, and the others during MR angiography and/or computed tomography (CT) angiography that had been performed in the evaluation of stroke, headache, syncope or a routine health check-up. Twenty-two aneurysms were found using conventional angiography plus MR angiography and/or CT angiography, two by using conventional angiography alone, and the remaining four by MR angiography alone.
MR image acquisition
MR imagings were acquired by using a 1.5-T system (Intera; Philips Medical Systems, Best, the Netherlands) with a six-channel sensitivity encoding (SENSE) head coil. The targeted coronal scan was obtained from a level of 1-cm anterior to the tuberculum sellae to a level of 1-cm posterior to it, and perpendicular to the anterior commisure (AC)-posterior commisure (PC) line with an angle 20° posteriorly on the sagittal scan (Fig. 1). The T2-weighted 3-D FSE-driven equilibrium RF reset pulse (DRIVE) sequence was performed with the following parameters : TR/TE = 1500/160 ms, 256 acquisition/256 reconstruction, 13-cm field of view, 1.5-mm section thickness with a 0.75-mm overlap, number of acquisitions = 2 and the total imaging time was less than 10 minutes.
Fig. 1.
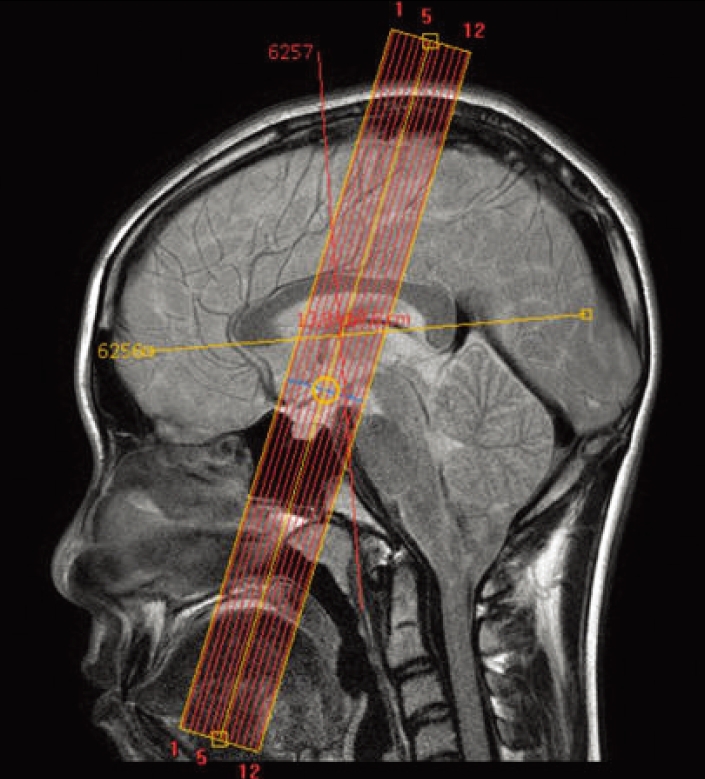
Magnetic resonance localizer for the targeted coronal scan, obtained from a level of 1-cm anterior to the tuberculum sellae to a level of 1-cm posterior to it, and perpendicular to the anterior commisure-posterior commisure line with an angle 20° posteriorly on the sagittal scan.
Data analysis
Two experienced neuroradiologists (D.J.K. and J.K.) reviewed the MR images without information about the angiographic findings, and a consensus was reached concerning the position of the distal dural ring and the location of the paraclinoid aneurysms in relation to the subarachnoid space. The imaging findings were compared with the angiographic findings, and in four patients it was possible to investigate the aneurysms during the surgery.
Based on the MR images, the locations of the aneurysms were classified into two categories : extradural (C4 or C5, cavernous or clinoid segments) or intradural locations (C6, ophthalmic segment). The aneurysms of the ophthalmic segment were classified topographically into ophthalmic (anterior variant) or superior hypophyseal aneurysms (medial or posteromedial variant).
RESULTS
Sixteen patients had a paraclinoid aneurysm involving the right ICA, while the other 12 patients had an aneurysm involving the left ICA. The mean size of the aneurysms was 4.3 mm (range, 2.3-11.0 mm). Five patients (18%) had multiple intracranial aneurysms; two with an aneurysm of the anterior communicating artery, one with bilateral aneurysms of the middle cerebral artery bifurcation, another with bilateral aneurysms of the ICA-posterior communicating artery junction, and the last one with an aneurysm of the posterior circulation.
All 28 aneurysms and their surrounding anatomic structures were identified on the T2-weighted 3-D FSE studies, and there was no discrepancy in the location and topography of the aneurysms between two neuroradiologists (Fig. 2). Thirteen aneurysms were considered to be located within the white subarachnoid space above the level of the distal dural ring, and the other 15 were determined to be in an extradural location confined to the cavernous sinus. The intradural aneurysms consisted of two ophthalmic aneurysms and 11 superior hypophyseal aneurysms in our series (Table 1).
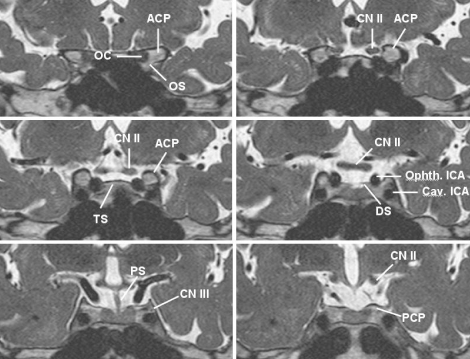
Fig. 2.
Sequential T2-weighted three-dimensional fast spin-echo magnetic resonance imaging in oblique coronal planes, photographed from anterior to posterior, shows the ICA in the paraclinoid region and its surrounding anatomic structures. ACP : anterior clinoid process, Cav. : cavernous, CN II : optic nerve, CN III : oculomotor nerve, DS : diaphragma sellae, ICA : internal carotid artery, OC : optic canal, OS : optic strut, Ophth. : ophthalmic, PCP : posterior clinoid process, PS : pituitary stalk, TS : tuberculum sellae.
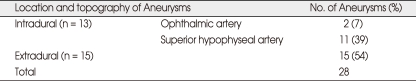
Table 1.
Summary of magnetic resonance data for 28 patients with unruptured paraclinoid aneurysms
Of the 13 intradural aneurysms, three superior hypophyseal artery aneurysms underwent satisfactory clipping, and two were clipped through the contralateral approach after a clipping of the aneurysms at the opposite side. During the surgery, the aneurysms observed on MR imaging at the roof of the cavernous sinus in the paraclinoid region were found to protrude into the cisterns, coinciding with the findings seen on MR imaging (Fig. 3). The other eight aneurysms were treated by endovascular coiling. The two ophthalmic aneurysms did not undergo any further treatment.
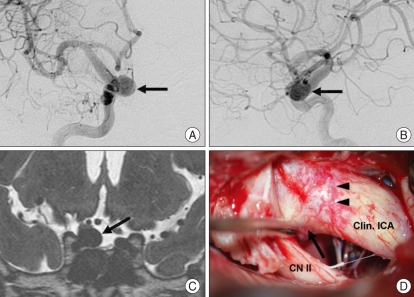
Fig. 3.
A 48-year-old man was incidentally diagnosed to have a intracranial aneurysm at the paraclinoid ICA. A and B : Preoperative anteroposterior (A) and lateral (B) angiogram show a large aneurysm (arrow) involving the right paraclinoid ICA at the level of the ophthalmic artery origin. It would be difficult to localize the aneurysm in relation to the distal dural ring, by using the level of ophthalmic artery origin as a landmark. C : T2-weighted three-dimensional fast spin-echo magnetic resonance imaging in the oblique coronal plane shows an aneurysm (arrow) within the cistern, arising from the medial aspect of the intradural ICA. D : Intraoperative photograph shows a superolateral view of the right paraclinoid region. The anterior clinoid process was drilled, exposing the aneurysm neck (arrow) protruding medially above the dissected distal dural ring (arrowheads). Clin. : clinoid, CN II : optic nerve, ICA : internal carotid artery.
Among the 15 aneurysms considered to be extradural on MR imaging, five aneurysms of relatively large in size were treated by endovascular coiling, while the remaining 10 aneurysms were placed under observation without any further treatment (Fig. 4). One of these 10 aneurysms was found to be located under the distal dural ring during the clipping of the contralateral unruptured aneurysm at the middle cerebral artery bifurcation. On follow-up, all of the patients were in good condition without any complaints of aneurysm-related symptoms.
Fig. 4.
A 57-year-old man was incidentally diagnosed to have a intracranial aneurysm at the paraclinoid ICA. A and B : Right anterior oblique (A) and lateral (B) angiogram show an aneurysm (arrow) involving the left paraclinoid ICA at the level of the ophthalmic artery origin. C : T2-weighted three-dimensional fast spin-echo magnetic resonance imaging in the oblique coronal plane shows an aneurysm (arrow) arising from the medial aspect of the extradural ICA, and confined to the cavernous sinus. ICA : internal carotid artery.
Among the 24 patients who underwent conventional angiography, eight aneurysms (33%) might have shown discordant findings with MR imagings in regard to their location, if they had been estimated simply on the basis of the level of ophthalmic artery origin.
DISCUSSION
At the point where the ICA enters the intradural space, the ICA becomes surrounded by a distal dural ring, that is tightly and circumferentially attached to the adventitia of the ICA. It is continuous with the roof of the cavernous sinus along its lateral aspect, overlying the superior surface of the anterior clinoid process, and is also continuous with the diaphragma sellae along its posteromedial aspect and the dura mater covering the tuberculum sellae along its anteromedial aspect2,11,13,22).
Clinically, it is critical to discriminate between aneurysms proximal to the dural ring and aneurysms distal to the dural ring, because their locations determine surgical indications and the patient's prognosis4,7,11,18). If an unruptured proximal carotid aneurysm can be demonstrated with certainty to lie below the dural ring, the risk of subsequent SAH is extremely low, since the aneurysm is protected by the overlying anterior clinoid process and dural reflection1,14).
Conventional angiography is considered to be the standard method for the evaluation of intracranial aneurysms. However, with conventional angiography, the exact localization of paraclinoid aneurysms in relation to the distal dural ring has been difficult to define using traditional landmarks. For instance, Punt20) recognized the origin of the ophthalmic artery as a marker for the intradural ICA, but it is an unreliable indicator because the origin of the ophthalmic artery is extradural in approximately 10% of cases6,7,11,15). Taptas23) proposed the anterior clinoid process as a better marker. However, the anterior clinoid process also occasionally fails as a marker because it is a relatively large structure that cannot be clearly visualized with conventional angiography. Moreover, some intradural aneurysms have been observed below the level of the anterior clinoid process7,11). Interestingly, some researchers have reported that the concavity on the outer surface of the paraclinoid ICA, the "dural waist," can be seen on conventional angiography or 3-D CT angiography, and it can be a predictor of subarachnoid extension8,12,17,26). Although it is the result of the ring's attachment, the "dural waist" is just another indirect indicator that cannot be always recognized.
Recently, a few researchers have attempted the direct visualization of the paraclinoid aneurysms with MR imaging24,25), and we used high-resolution heavily T2-weighted 3-D FSE sequence for showing the topography of unruptured paraclinoid aneurysms incidentally found in 28 patients. The 3-D T2-FSE sequence has become clinically available as a result of recent technological advances in MR imaging, including the development of high-speed data processing, which makes it possible to obtain high-resolution images with an acceptable SNR by 3-D data acquisition19,27). The 3D T2-FSE sequence allows small blood vessels to be viewed with higher resolution than CT angiography, because the cerebral cisterns, nerves, and blood vessels are displayed with high contrast16,21). All of the paraclinoid aneurysms in our study were identified using a 3-D T2-FSE sequence, which was of great value in understanding the topography of paraclinoid aneurysms in relation to the "white" subarachnoid space and the "black" cavernous sinus. This technique enabled these structures to be observed from any desired projection and demonstrated the interrelationships between various anatomic structures "simultaneously", even in case of SAH by a ruptured aneurysm.
Many anatomical studies have revealed that the distal dural ring does not extend in a perfectly-flat horizontal plane. Instead, it slopes slightly downward both in the anterior-to-posterior and in the lateral-to-medial directions3,18). The plane of the dural ring inclines in the posterior direction with an angle of 5 to 43° (mean, 20.3°) in the lateral projection, so that we acquired coronal images obliquely with an angle of 110° to the AC-PC line on sagittal scan. This was done to demonstrate the exact point where the ascending ICA enters into the subarachnoid space. Optimizing scanning parameters is also necessary to create a greater difference in the signal intensity of the vessels relative to the cerebrospinal fluid and brain parenchyma.
The "carotid cave" is a dural invagination along the medial aspect of the ophthalmic segment at the level of the distal dural ring, which produces an extension of the intradural subarachnoid space and the possibility of SAH in case of rupture of the aneurysm located within it11,13). The carotid cave has been reported to be present in 68 to 90% of cadaveric specimens, and 36% of the superior hypophyseal arteries were thought to arise from the carotid cave7,11,18). With the targeted T2-weighted 3-D FSE MR imaging technique with higher resolution, it might be also possible to localize a paraclinoid aneurysm found in the carotid cave, which cannot be predicted by conventional angiography.
In this study, it can be a shortcoming that only a few aneurysms were identified at the time of open surgery. But we believe that the T2-weighted 3-D FSE MR imaging can be another complementary technique in the evaluation of paraclinoid aneurysms because of the high spatial resolution of the MR imaging, and that further study for comparison is necessary with a cadaveric dissection or intraoperative findings.
CONCLUSION
We performed prospective MR imaging studies for the detailed preoperative evaluation of an unruptured paraclinoid aneurysm of the ICA. This technique would be helpful in deciding on a surgical strategy preoperatively, as well as in the demonstration of accurate anatomic relationships among the paraclinoid aneurysms and their surrounding compartments from any desired projections. In the evaluation of paraclinoid aneurysms, we believe that preoperative imaging with this MR technique is advisable.
References
- 1.Barr HW, Blackwood W, Meadows SP. Intracavernous carotid aneurysms. A clinical-pathological report. Brain. 1971;94:607–622. doi: 10.1093/brain/94.4.607. [DOI] [PubMed] [Google Scholar]
- 2.Bouthillier A, van Loveren HR, Keller JT. Segments of the internal carotid artery : a new classification. Neurosurgery. 1996;38:425–432. doi: 10.1097/00006123-199603000-00001. discussion 432-433. [DOI] [PubMed] [Google Scholar]
- 3.Day AL. Aneurysms of the ophthalmic segment. A clinical and anatomical analysis. J Neurosurg. 1990;72:677–691. doi: 10.3171/jns.1990.72.5.0677. [DOI] [PubMed] [Google Scholar]
- 4.De Jesús O, Sekhar LN, Riedel CJ. Clinoid and paraclinoid aneurysms : surgical anatomy, operative techniques, and outcome. Surg Neurol. 1999;51:477–487. doi: 10.1016/s0090-3019(98)00137-2. discussion 487-488. [DOI] [PubMed] [Google Scholar]
- 5.Dolenc VV. A combined epi- and subdural direct approach to carotid-ophthalmic artery aneurysms. J Neurosurg. 1985;62:667–672. doi: 10.3171/jns.1985.62.5.0667. [DOI] [PubMed] [Google Scholar]
- 6.Gibo H, Lenkey C, Rhoton AL., Jr Microsurgical anatomy of the supraclinoid portion of the internal carotid artery. J Neurosurg. 1981;55:560–574. doi: 10.3171/jns.1981.55.4.0560. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez LF, Walker MT, Zabramski JM, Partovi S, Wallace RC, Spetzler RF. Distinction between paraclinoid and cavernous sinus aneurysms with computed tomographic angiography. Neurosurgery. 2003;52:1131–1137. discussion 1138-1139. [PubMed] [Google Scholar]
- 8.Horowitz M, Fichtel F, Samson D, Purdy P. Intracavernous carotid artery aneurysms : the possible importance of angiographic dural waisting. A case report. Surg Neurol. 1996;46:549–552. doi: 10.1016/s0090-3019(96)00163-2. [DOI] [PubMed] [Google Scholar]
- 9.Inoue T, Rhoton AL, Jr, Theele D, Barry ME. Surgical approaches to the cavernous sinus: a microsurgical study. Neurosurgery. 1990;26:903–932. doi: 10.1097/00006123-199006000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Ito K, Hongo K, Kakizawa Y, Kobayashi S. Three-dimensional contrast medium-enhanced computed tomographic cisternography for preoperative evaluation of surgical anatomy of intradural paraclinoid aneurysms of the internal carotid artery : technical note. Neurosurgery. 2002;51:1089–1092. doi: 10.1097/00006123-200210000-00045. discussion 1092-1093. [DOI] [PubMed] [Google Scholar]
- 11.Kim JM, Romano A, Sanan A, van Loveren HR, Keller JT. Microsurgical anatomic features and nomenclature of the paraclinoid region. Neurosurgery. 2000;46:670–680. doi: 10.1097/00006123-200003000-00029. discussion 680-682. [DOI] [PubMed] [Google Scholar]
- 12.Kim MY, Chung SY, Kim SM, Park MS, Jung SS. Determination of aneurysmal location with 3 dimension-computed tomographic angiography in the microsurgery of paraclinoid aneurysms. J Korean Neurosurg Soc. 2007;42:35–41. [Google Scholar]
- 13.Kobayashi S, Kyoshima K, Gibo H, Hegde SA, Takemae T, Sugita K. Carotid cave aneurysms of the internal carotid artery. J Neurosurg. 1989;70:216–221. doi: 10.3171/jns.1989.70.2.0216. [DOI] [PubMed] [Google Scholar]
- 14.Kupersmith MJ, Hurst R, Berenstein A, Choi IS, Jafar J, Ransohoff J. The benign course of cavernous carotid artery aneurysms. J Neurosurg. 1992;77:690–693. doi: 10.3171/jns.1992.77.5.0690. [DOI] [PubMed] [Google Scholar]
- 15.Kyoshima K, Oikawa S, Kobayashi S. Interdural origin of the ophthalmic artery at the dural ring of the internal carotid artery. Report of two cases. J Neurosurg. 2000;92:488–489. doi: 10.3171/jns.2000.92.3.0488. [DOI] [PubMed] [Google Scholar]
- 16.Mitsuoka H, Tsunoda A, Okuda O, Sato K, Makita J. Delineation of small nerves and blood vessels with three-dimensional fast spin-echo MR imaging : comparison of presurgical and surgical findings in patients with hemifacial spasm. AJNR Am J Neuroradiol. 1998;19:1823–1829. [PMC free article] [PubMed] [Google Scholar]
- 17.Murayama Y, Sakurama K, Satoh K, Nagahiro S. Identification of the carotid artery dural ring by using three-dimensional computerized tomography angiography. Technical note. J Neurosurg. 2001;95:533–536. doi: 10.3171/jns.2001.95.3.0533. [DOI] [PubMed] [Google Scholar]
- 18.Oikawa S, Kyoshima K, Kobayashi S. Surgical anatomy of the juxtadural ring area. J Neurosurg. 1998;89:250–254. doi: 10.3171/jns.1998.89.2.0250. [DOI] [PubMed] [Google Scholar]
- 19.Oshio K, Jolesz FA, Melki PS, Mulkern RV. T2-weighted thin-section imaging with the multislab three-dimensional RARE technique. J Magn Reson Imaging. 1991;1:695–700. doi: 10.1002/jmri.1880010614. [DOI] [PubMed] [Google Scholar]
- 20.Punt J. Some observations on aneurysms of the proximal internal carotid artery. J Neurosurg. 1979;51:151–154. doi: 10.3171/jns.1979.51.2.0151. [DOI] [PubMed] [Google Scholar]
- 21.Rubinstein D, Sandberg EJ, Breeze RE, Sheppard SK, Perkins TG, Cajade-Law AG, et al. T2-weighted three-dimensional turbo spin-echo MR of intracranial aneurysms. AJNR Am J Neuroradiol. 1997;18:1939–1943. [PMC free article] [PubMed] [Google Scholar]
- 22.Seoane E, Rhoton AL, Jr, de Oliveira E. Microsurgical anatomy of the dural collar (carotid collar) and rings around the clinoid segment of the internal carotid artery. Neurosurgery. 1998;42:869–884. doi: 10.1097/00006123-199804000-00108. discussion 884-886. [DOI] [PubMed] [Google Scholar]
- 23.Taptas JN. Intradural and extradural ICA. J Neurosurg. 1979;51:877–878. doi: 10.3171/jns.1979.51.6.0877a. [DOI] [PubMed] [Google Scholar]
- 24.Thines L, Gauvrit JY, Leclerc X, Le Gars D, Delmaire C, Pruvo JP, et al. Usefulness of MR imaging for the assessment of nonophthalmic paraclinoid aneurysms. AJNR Am J Neuroradiol. 2008;29:125–129. doi: 10.3174/ajnr.A0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thines L, Lee SK, Dehdashti AR, Agid R, Willinsky RA, Wallace CM, et al. Direct imaging of the distal dural ring and paraclinoid internal carotid artery aneurysms with high-resolution T2 turbo-spin echo technique at 3-T magnetic resonance imaging. Neurosurgery. 2009;64:1059–1064. doi: 10.1227/01.NEU.0000343523.67272.34. discussion 1064. [DOI] [PubMed] [Google Scholar]
- 26.White JA, Horowitz MB, Samson D. Dural waisting as a sign of subarachnoid extension of cavernous carotid aneurysms : a follow-up case report. Surg Neurol. 1999;52:607–609. doi: 10.1016/s0090-3019(99)00136-6. discussion 609-610. [DOI] [PubMed] [Google Scholar]
- 27.Yuan C, Schmiedl UP, Weinberger E, Krueck WR, Rand SD. Three-dimensional fast spin-echo imaging : pulse sequence and in vivo image evaluation. J Magn Reson Imaging. 1993;3:894–899. doi: 10.1002/jmri.1880030617. [DOI] [PubMed] [Google Scholar]