Abstract
Langerhans cell histiocytosis (LCH), a disorder of the phagocytic system, is a rare condition. Moreover, spinal involvement causing myelopathy is even rare and unusual. Here, we report a case of atypical LCH causing myelopathy, which was subsequently treated by corpectemy and fusion. A 5-year-old boy presented with 3 weeks of severe neck pain and limited neck movement accompanying right arm motor weakness. CT scans revealed destruction of C7 body and magnetic resonance imaging showed a tumoral process at C7 with cord compression. Interbody fusion using cervical mesh packed by autologus iliac bone was performed. Pathological examination confirmed the diagnosis of LCH. After the surgery, the boy recovered from radiating pain and motor weakness of right arm. Despite the rarity of the LCH in the cervical spine, it is necessary to maintain our awareness of this condition. When neurologic deficits are present, operative treatment should be considered.
Keywords: Langerhans cell histiocytosis, Cervical spine, Cord compression
INTRODUCTION
Langerhans cell histiocytosis (LCH) is a disease characterized by excessive accumulation of pathologic Langerhans cells2). Langerhans cells are dendritic cells that are found in greatest numbers in the skin3). LCH can present at any age from the neonate until old age. The commonest presentation of LCH in childhood is with a single mas lesion on the skull. Although it is an infrequent disease overall, LCH can involve the spine7). Most of them are treated with excellent outcomes without extensive surgery. In the spine, LCH most commonly affects the thoracic vertebrae while involvement of the cervical vertebra is rare9,11,12). We report a case of a child, diagnosed with LCH as a single LCH lesion causing myelopathy in the cervical spine which was subsequently treated by corpectomy and fusion.
CASE REPORT
A 5-year-old boy presented with 3 weeks of severe neck pain and limited neck movement. This was followed by complaints of pain in the right shoulder radiating to right upper arm and paresthesia. On physical examination, the patient had mild tenderness to palpation in the cervical spine. Neurologic examination showed slight motor weakness in the right upper arm (Grade IV). He was afebrile and results of blood tests, including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), were all within normal limits. Radiography of the cervical spine showed marked destruction of C7 body (Fig. 1A). Computed tomography (CT) scans revealed destruction of the corpus vertebra, but intact disc space on C6-C7, C7-T1 (Fig. 1B). Magnetic resonance imaging (MRI) revealed a tumoral process at C7 with destruction of the vertebral body and cord compression (Fig. 2); however, based on the MRI, the disc spaces remained intact. Based on both the clinical symptoms and radiologic findings, this case was considered as malignant neoplasm. Due to his intractable pain and motor weakness, surgical treatment was performed using an anterior approach. A C7 corpectomy followed by C6-C7 discectomy were performed. We performed interbody fusion using cervical mesh packed by autologus iliac bone grafted from the iliac crest. The patient's cervical spine was immobilized after surgery in a rigid cervical orthosis for 3 months. Halo-vest was not applied due to his young age. Subsequent pathological examination confirmed the diagnosis of LCH. This examination included a microscopy-based review as well as a strong positive immunohistochemical reaction for the S-100 protein, a marker of LCH (Fig. 3). After the surgery, the patient recovered from right upper arm radiating pain and motor weakness. He has now been in follow-up for 13 months. There have been no subjective complaints and no recurrence (Fig. 4).
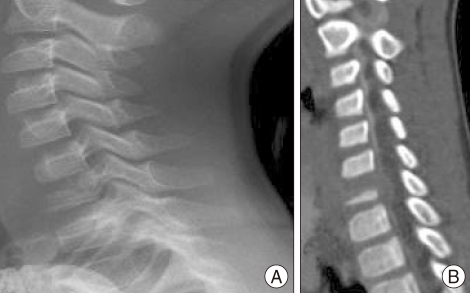
Fig. 1.
Preoperative radiographs show tumoral process at C7. A : Simple lateral radiograph reveals marked destruction of C7 body. B : Computed tomographic scan of cervical spine shows vertebral body destruction, namely, typical vertebra plana.
Fig. 2.
T1 and T2 weighted magnetic resonance images show cord compressing tumoral mass at C7 level.
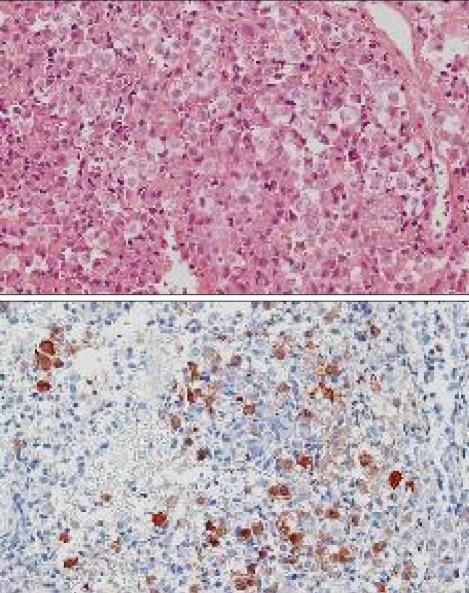
Fig. 3.
There are atypical histiocytic proliferations in bone marrow of vertebral body. Immunohistochemically, these cells have immunoreactivity for S-100 protein. (H&E ×100)
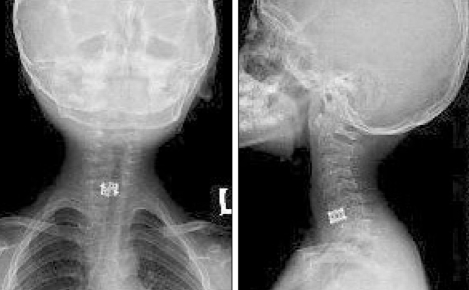
Fig. 4.
Thirteen months follow-up cervical spine radiographs demonstrate good bone fusion without any kyphotic deformities.
DISCUSSION
LCH is a rare disorder characterized by an excessive proliferation of pathologic Langerhans cells. The disease varies widely in clinical presentation from localized involvement of a single bone to a widely disseminated life-threatening disease (8). LCH includes three previously disparate diagnoses. Ranging from severity, they are Letterer-Siwe disease, Hand-Schüller-Christian disease, and eosinophilic granuloma. Letterer-Siwe disease involves multiple organs and Hand-Schüller-Christian disease presents with bony lesions and endocrine abnormalities. However, eosinophilic granuloma presents with isolated bony lesions3). Among them, variants of LCH other than eosinophilic granuloma, are far less likely to affect the spine. Eosinophilic granuloma occurs in the first or second decade with a peak incidence between 5 and 10 years of age, but spinal involvement is still rare13). The most commonly affected bone is the skull, followed by the long bones, the flat bones, and the vertebrae. In the spine, LCH most frequently affects the thoracic vertebrae. Solitary lytic lesions forming as a result of LCH in the cervical spine are very rare in children. Estimating the frequency of LCH in the cervical spine as a single lesion is difficult. Howarth et al.5) reported that the involvement of the cervical spine was present in only 0.02% of 342 bone lesions. LCH normally presents only with localized neck or back pain. Neurologic deficits are extremely rare and, when present, are usually only mild paresthesias or radiating pain1,4). Owing to the relative rarity of this disease, it remains a condition in which the diagnosis is often delayed or missed. The disease normally limits itself to bone; therefore, large soft tissue masses are not normally palpable on examination or present on imaging. On the contrary, malignancies such as Ewing sarcoma or osteosarcoma usually present with large soft tissue masses. Biopsy is necessary to confirm its diagnosis and to exclude malignancy or infectious diseases. The differential diagnosis includes Ewing sarcoma, osteomyelitis, lymphoma, osteosarcoma, and neuroblastoma. In most LCH cases, aggressive spine fusion beyond biopsy is not necessary for child cases involving the spine. Many studies have shown excellent healing and resolution of LCH using a variety of treatment including bracing, surgery, chemotherapy, radiation therapy, and even no therapy for its excellent prognosis6,10). Treatment is guided by extent of disease. Solitary bone lesion may be amenable through excision or limited radiation. However systemic diseases may require chemotherapy. Chemotherapeutic agents such as alkylating agents, antimetabolites, vinca alkaloids either singly or in combination can lead to complete remission in diffuse disease. Resolution of vertebral height for anterior lesions has also been described in the natural history of LCH. To prevent spinal deformity or permanent neurologic deficits, surgical treatment is also considered in selected cases; however, it should only be performed in cases of severe kyphosis or those exhibiting neurologic compromise. In our case, we had to perform extensive fusion surgery due to neurologic deficits caused by cord compression, which threatened the patient's neurologic function. The boy has now been in follow-up for 13 months, and he is doing well free from pain, motor weakness, or any limitation due to his previous LCH.
CONCLUSION
LCH in young children remains a dilemma for spinal surgeons. Despite the rarity of the disease in the cervical spine, it is necessary to maintain our awareness of this condition. When neurologic deficits are present, operative treatment should be considered.
References
- 1.Davidson RI, Shillito J., Jr Eosinophilic granuloma of the cervical spine in children. Pediatrics. 1970;45:746–752. [PubMed] [Google Scholar]
- 2.Favara BE, Feller AC, Pauli M, Jaffe ES, Weiss LM, Arico M, et al. The WHO Committee On Histiocytic/Reticulum Cell Proliferations. Reclassification Working Group of the Histiocyte Society. Contemporary classification of histiocytic disorders. Med Pediatr Oncol. 1997;29:157–166. doi: 10.1002/(sici)1096-911x(199709)29:3<157::aid-mpo1>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 3.Garg S, Mehta S, Dormans JP. An atypical presentation of Langerhans cell histiocytosis of the cervical spine in a child. Spine (Phila Pa 1976) 2003;28:E445–E448. doi: 10.1097/01.BRS.0000096462.51682.0F. [DOI] [PubMed] [Google Scholar]
- 4.Green NE, Robertson WW, Jr, Kilroy AW. Eosinophilic granuloma of the spine with associated neural deficit. Report of three cases. J Bone Joint Surg Am. 1980;62:1198–1202. [PubMed] [Google Scholar]
- 5.Howarth DM, Gilchrist GS, Mullan BP, Wiseman GA, Edmonson JH, Schomberg PJ. Langerhans cell histiocytosis : diagnosis, natural history, management, and outcome. Cancer. 1999;85:2278–2290. doi: 10.1002/(sici)1097-0142(19990515)85:10<2278::aid-cncr25>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 6.Ippolito E, Farsetti P, Tudisco C. Vertebra plana. Long-term follow-up in five patients. J Bone Joint Surg Am. 1984;66:1364–1368. [PubMed] [Google Scholar]
- 7.Kilpatrick SE, Wenger DE, Gilchrist GS, Shives TC, Wollan PC, Unni KK. Langerhans' cell histiocytosis (histiocytosis X) of bone. A clinicopathologic analysis of 263 pediatric and adult cases. Cancer. 1995;76:2471–2484. doi: 10.1002/1097-0142(19951215)76:12<2471::aid-cncr2820761211>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 8.Ladisch S. Langerhans cell histiocytosis. Curr Opin Hematol. 1998;5:54–58. doi: 10.1097/00062752-199801000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Levine SE, Dormans JP, Meyer JS, Corcoran TA. Langerhans' cell histiocytosis of the spine in children. Clin Orthop Relat Res. 1996:288–293. doi: 10.1097/00003086-199602000-00040. [DOI] [PubMed] [Google Scholar]
- 10.Raab P, Hohmann F, Kühl J, Krauspe R. Vertebral remodeling in eosinophilic granuloma of the spine. A long-term follow-up. Spine (Phila Pa 1976) 1998;23:1351–1354. doi: 10.1097/00007632-199806150-00011. [DOI] [PubMed] [Google Scholar]
- 11.Robert H, Dubousset J, Miladi L. Histiocytosis X in the juvenile spine. Spine (Phila Pa 1976) 1987;12:167–172. doi: 10.1097/00007632-198703000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Seimon LP. Eosinophil granuloma of the spine. J Pediatr Orthop. 1981;1:371–376. doi: 10.1097/01241398-198112000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Sohn MJ, Park HC, Park HS, Kim JJ, Kim EY. Anterior cervical corpectomy and fusion using miniplate and screws in a 7-year-old child with eosinophilic granuloma of the cervical spine. Spine (Phila Pa 1976) 2001;26:1193–1196. doi: 10.1097/00007632-200105150-00023. [DOI] [PubMed] [Google Scholar]