Abstract
This article reports an analysis of 75 consecutive lower limb amputees who developed painful neuroma requiring surgical excision after lower limb amputation following landmine explosions. This retrospective study analyses the results of 75 patients who were treated for painful neuroma after lower limb amputation following landmine explosions between the years 2000 and 2006. The average time period from use of prosthesis to start of symptoms suggesting neuroma was 9.6 months. The average time period from start of pain symptoms to neuroma surgery was 7.8 months. All clinically proven neuromas were surgically resected. In the mean follow-up of 2.8 years, all patients were satisfied with the end results and all were free of any pain symptoms. Painful stump with clinical diagnostic findings of neuroma described above may be regarded as neuroma without requiring any further imaging modalities and is an indication for surgery if conservative measures fail.
Résumé
Rapporter l’analyse de 75 patients amputés du membre inférieur qui ont développé des névromes douloureux, nécessitant une ablation chirurgicale, après une amputation causée par explosions de mines. cette étude rétrospective analyse les résultats de 75 patients opérés pour névromes douloureux après amputation du membre inférieur causé par explosions de mines entre 2000 et 2006. l’intervalle moyen entre le début du port d’une prothèse et le début des symptômes évoquant l’apparition d’un névrome est de 9,6 mois. L’intervalle de temps moyen entre le début des symptômes et la chirurgie d’ablation du névrome est de 7,8 mois. Tous les névromes démontrés chirurgicalement ont été réséqués. Sur la période de suivi moyen de 2,8 ans tous les patients ont été satisfaits du résultat final et n’avaient plus aucune douleur. les moignons douloureux avec des signes cliniques de névrome sont à considérer comme des névromes authentiques sans nécessité d’imagerie complémentaire et peuvent être traités chirurgicalement si les traitements conservateurs ne sont pas efficaces.
Introduction
Amputation is one of the oldest types of surgery and the most commonly performed. It is indicated in a variety of pathological conditions including major limb trauma, posttraumatic gangrenous infections, ischemia, uncontrollable infected pseudarthrosis, and tumours with neurovascular invasion. The major indication for amputation is to preserve the life of the patient, i.e. to sacrifice a part of the body to save life.
During both war and peace, transtibial amputation is the most common level of major amputation and transfemoral amputation is the second most common [4, 12, 13, 15, 17, 21]. Explosive munitions, such as land mines, artillery shells, mortar shells, bombs, and grenades, have been the primary agents of battlefield amputation since World War II. Today, in strife-torn regions throughout the world, an estimated 90–110 million antipersonnel land mines pose the threat of amputation to residents and peacekeepers alike [1].
Because of war, internal conflicts, and terrorism, landmines are being placed in increasingly greater areas of land. The most common type is the antipersonnel mine, which has lower energy than the other types, and is not always life threatening, but it poses a risk to the limb with which it comes into contact [2, 3, 10, 14].
Several postoperative complications associated with pain may develop in the stump of an amputated lower limb. Clinical findings are often nonspecific; however, radiological evaluation, especially with magnetic resonance (MR) imaging, is useful in the early diagnosis of these complications, thereby helping minimise physical disability with its psychological and socioeconomic implications. Conventional radiography can demonstrate evidence of osseous origins of pain (e.g., raised bone edge, heterotopic ossification, osteomyelitis) and should be the first imaging study performed after clinical examination. Ultrasonography can demonstrate inflammatory changes in the stump as well as soft-tissue fluid collections. However, MR imaging is the modality of choice when clinical and other imaging findings are indeterminate. Because of its high spatial and contrast resolution, MR imaging can demonstrate subtle inflammatory changes, fluid collections, cancers, neuromas, and subtle traumatic bone lesions.
One of the potentially troublesome sequelae of lower limb amputations is the development of stump neuromas at the severed ends of major nerves. The ability to define them and to distinguish them from other causes of stump pain is of considerable clinical significance. A neuroma is a tumour-like thickening of a nerve stump in the region of the scar after amputation of a limb and is tender to pressure. Even after only mild stimulation, neuromas transmit strong pain signals. If local measures to relieve pain are inadequate, it may be worth considering a surgical removal of the painful neuroma. This condition makes it virtually impossible to mould a well-fitting prosthesis socket.
There is little information in the literature regarding incidence, consequences, or outcomes of painful neuroma subsequent to lower limb amputation caused by land-mine explosions. This article aimed to report an analysis of 75 consecutive lower limb amputees who developed painful neuromas requiring surgical excision after lower limb amputation following landmine explosions.
Materials and methods
This retrospective study analysed the results of 75 patients who were treated in our centre for painful neuroma after lower limb amputation following landmine explosions between the period of January 2000 and January 2006. During this period, the total number of patients suffering from land mine injuries who underwent lower extremity amputation was 527.
The initial and emergency treatment of acute lower limb amputations of the cases in the conflict area (where the separatist rebellion groups have terrorist activity against Turkish Armed Forces) had been performed in nine different field hospitals where experienced surgical teams were located. Of 75 patients, 52 (69%) had transtibial (7 bilateral) and the remaining 23 (31%) had transfemoral (4 bilateral) amputations. All of the patients were males with an average age of 26.2 years (range, 22–30 years).
All of the patients had moderate to severe stump pain and clinical signs suggestive of neuroma. Magnetic resonance imaging (MRI) and other radiological modalities were not used routinely for the diagnosis of neuroma in the stumps. The diagnosis was established on a clinical basis, and presence of a painful swelling in the stump was regarded as a satisfactory finding for neuroma.
All patients with neuroma were limited in their ability to use prostheses prior to surgery and, following failure of conservative measures (physical therapy, nonsteroidal antiinflammatory agents, injections) for at least 6 months, were referred for surgical opinion.
From the medical records and patients themselves, we have obtained information about how the initial injury occurred, the number and type of subsequent surgical procedures, and other medical problems. Also, information was obtained about current use of a prosthesis (the type of prosthesis, wear duration from last surgery, the number of hours it was worn each day, and dermatological or other prosthesis-related complications encountered).
Results
The records of 75 patients who had sustained an amputation on the battlefield and were surgically treated in our centre for painful neuroma were retrospectively reviewed.
From the initial medical records obtained, the mean time between patients’ injury and arrival at the clinic where the amputation was performed was 8.3 hours (range, 6–18 hours). While injuries occurred in a single limb in 64 of the patients, there were injuries in other limbs or other systems in the rest. The most frequent accompanying pathologies were head and neck injuries (8 cases, 10.6%). After the initial surgery (amputation with primary wound closure), 21 patients underwent revision surgery because of infection and wound healing problems. The mean time in hospital for primary amputation surgery was 16.4 days (range, 12–20 days).
The average period from amputation to admission for prosthetic fitting was 121 days (range, 96–150 days). The average period of prosthetic supply and training in our centre was 65 days (including nonworking days and weekends). As was to be expected, prosthetic supply was accompanied by certain local complications: flexion contractures of the neighbouring joint (knee, hip) and complications of the soft tissues of stump (necrosis, dehiscence, ischaemic tissue damage), which were responsible for the slower course of prosthetic supply.
The average time period from start of prosthesis wear and start of symptoms suggesting neuroma was 9.6 months (range, 6–12 months). The average time period from start of pain symptoms to neuroma surgery was 7.8 months (range, 6–9 months). During these periods, the average amount of daily use of the prosthesis was 7.1 hours for unilateral transtibial amputees, 6.7 hours for unilateral transfemoral amputees, 6.3 for bilateral transtibial amputees, and 5.8 hours for bilateral transfemoral amputees.
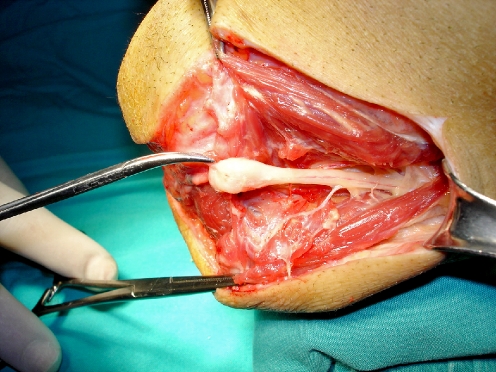
All clinically proven neuromas were resected under regional anesthesia with the help of a tourniquet (Fig. 1). During surgery, 2–4 cm shortening of bones was done in eight patients to improve closure. With the exception of three cases, no complications such as wound dehiscence or infection were observed. In those three cases, wound dehiscence was resolved as a result of local revision surgery. The average time period from neuroma surgery to start of prosthetic supply was 3 months, and prosthesis fitting and an adequate postprosthesis training programme lasted an average of 58 days. At the mean follow-up of 2.8 years (range, 6 months to 6 years), all patients were found to be satisfied with the end result and all were free of any pain symptoms.
Fig. 1.
Intraoperative appearance of neuroma in below-knee amputation stump
Discussion
Care of battlefield casualties is a concern for peacekeepers who must treat not only soldiers but also civilian casualties of war. Injuries caused by land mines remain a major clinical problem in areas of conflict in Asia, Africa, and the Balkans [1, 2, 4, 8, 14, 18].
Our institution is a specialised rehabilitation and care centre serving veterans with extremity amputations. Treatment by a service that specifically deals with amputees has proven beneficial for both patients and providers. The patient has the benefit of being with individuals who have similar medical problems. An amputee centre allows for the concentration of surgeons, nurses, prosthetists, and physical therapists to provide consistent care for the patients [6]. Gaining experience in the care of patients who have sustained an amputation during battle is essential.
Preservation of functional joints during the first treatment of traumatic amputations of the extremities has great importance for the rehabilitation and application of a prosthesis. King [11] reported that amputation resulting from land mines has a difficult and a different part in war wound treatment. A careful debridement must be performed, and soft tissues with the myoplasty technique must cover the osseous structures.
Neuroma is a non-neoplastic proliferation that occurs at the end of an injured nerve and is usually seen 1–12 months after amputation [7, 16]. Pain associated with a neuroma does not always have a precise topography and is often difficult to distinguish from phantom limb pain. Clinical findings may be normal or may include a soft-tissue mass or pain related to percussion of the stump (Tinel sign). Pain relief with injection of lidocaine in the painful area may help confirm the diagnosis.
Imaging is useful for confirmation and localisation of a painful neuroma. Detection is usually difficult when the neuroma is less than 1 cm. Most radiologically detected neuromas have been reported to measure 1.0–3.5 cm. MR imaging is considered optimal for detection of a neuroma [5, 19, 20].
To prevent neuromas from developing following amputation, the surgeon should cut the nerve and pull it moderately to induce retraction of the nerve ending away from the muscular-cutaneous scar [9, 22]. During the postoperative period, it is also important to mobilise the surgical scar to prevent the scar from adhering to underlying tissues [9, 22].
Conservative therapy has been reported to be successful in more than half of affected patients [2, 7, 16]. Corticosteroid therapy, nerve stimulation, or reshaping of the socket may help relieve pain. Resection of a neuroma should be undertaken in cases of persistent pain. In our opinion, painful stump with clinical diagnostic findings of neuroma described above may be regarded as neuroma without requiring any further imaging modalities and may undergo surgery if conservative measures fail.
References
- 1.Aboutanos MB, Baker SP. Wartime civilian injuries: epidemiology and intervention strategies. J Trauma. 1997;43:719–726. doi: 10.1097/00005373-199710000-00031. [DOI] [PubMed] [Google Scholar]
- 2.Atesalp AS, Erler K, Gur E, Solakoglu C. Below-knee amputations as a result of land-mine injuries: comparison of primary closure versus delayed primary closure. J Trauma. 1999;47:724–727. doi: 10.1097/00005373-199910000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Atesalp AS, Erler K, Gur E, Koseoglu E, Kirdemir V. Bilateral lower limb amputations as a result of land-mine injuries. Prosthet Orthot Int. 1999;23:50–54. doi: 10.3109/03093649909071610. [DOI] [PubMed] [Google Scholar]
- 4.Coupland R, Korver A. Injuries from antipersonnel land mines: the experience of the International Committee of the Red Cross. BMJ. 1991;303:1509–1512. doi: 10.1136/bmj.303.6816.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donnal JF, Blinder RA, Coblentz CL, Moylan JA, Fitzpatrick KP. MR imaging of stump neuroma. J Comput Assist Tomogr. 1990;14(4):656–657. doi: 10.1097/00004728-199007000-00028. [DOI] [PubMed] [Google Scholar]
- 6.Dougherty PJ. Transtibial amputees from the Vietnam War. Twenty-eight year follow-up. J Bone Joint Surg Am. 2001;83:383–389. doi: 10.2106/00004623-200103000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Dougherty PJ. Long-term follow-up of unilateral transfemoral amputees from the Vietnam War. J Trauma. 2003;54:718–723. doi: 10.1097/01.TA.0000046260.16866.A9. [DOI] [PubMed] [Google Scholar]
- 8.Gondring WH. The anti-personnel land mine epidemic: a case report and review of the literature. Mil Med. 1996;161:760–762. [PubMed] [Google Scholar]
- 9.Gorkisch K, Boese-Landgraf J, Vaubel E. Treatment and prevention of amputation neuromas in hand surgery. Plast Reconstr Surg. 1984;73(2):293–299. doi: 10.1097/00006534-198402000-00027. [DOI] [PubMed] [Google Scholar]
- 10.Khan MT, Husain FN, Ahmet A. Hind-foot injuries due to land mine blast accidents. Injury. 2002;33:167–171. doi: 10.1016/S0020-1383(01)00092-4. [DOI] [PubMed] [Google Scholar]
- 11.King KF, Rne M. Orthopedic aspects of war wounds in South Vietnam. J Bone Joint Surg Br. 1969;51:112–117. [PubMed] [Google Scholar]
- 12.Korver A. Injuries of the lower limbs caused by antipersonnel mines: the experience of the International Committee of the Red Cross. Injury. 1996;27:477–479. doi: 10.1016/0020-1383(96)00066-6. [DOI] [PubMed] [Google Scholar]
- 13.Livingston DH, Keenan D, Kim D, Elcavage J, Malangoni MA. Extent of disability following traumatic extremity amputation. J Trauma. 1994;37:495–499. doi: 10.1097/00005373-199409000-00027. [DOI] [PubMed] [Google Scholar]
- 14.Meade P, Mirocha J. Civilian land-mine injuries in Sri Lanka. J Trauma. 2000;48:735–739. doi: 10.1097/00005373-200004000-00024. [DOI] [PubMed] [Google Scholar]
- 15.Moore TJ, Barron J, Hutchinson F, III, Golden C, Ellis C, Humphries D. Prosthetic usage following major lower extremity amputation. Clin Orthop. 1989;238:219–224. [PubMed] [Google Scholar]
- 16.Necmioglu S, Subasi M, Kayikci C, Young DB. Lower-limb landmine injuries. Prosthet Orthot Int. 2004;28:37–43. doi: 10.3109/03093640409167923. [DOI] [PubMed] [Google Scholar]
- 17.Odom CB. Causes of amputations in battle casualties with emphasis on vascular injuries. Surgery. 1946;20:562–569. [PubMed] [Google Scholar]
- 18.Simper LB. Below knee amputation in war surgery: a review of 111 amputations with delayed primary closure. J Trauma. 1993;34:96–98. doi: 10.1097/00005373-199301000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Singson RD, Feldman F, Slipman CW, Gonzalez E, Rosenberg ZS, Kiernan H. Postamputation neuromas and other symptomatic stump abnormalities: detection with CT. Radiology. 1987;162(3):743–745. doi: 10.1148/radiology.162.3.3809488. [DOI] [PubMed] [Google Scholar]
- 20.Singson RD, Feldman F, Staron R, Fechtner D, Gonzalez E, Stein J. MRI of postamputation neuromas. Skeletal Radiol. 1990;19(4):259–262. doi: 10.1007/BF00191667. [DOI] [PubMed] [Google Scholar]
- 21.Smith DG, Horn P, Malchow D, Boone DA, Reiber GE, Hansen ST., Jr Prosthetic history, prosthetic charges, and functional outcome of the isolated, traumatic below-knee amputee. J Trauma. 1995;38:44–47. doi: 10.1097/00005373-199501000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Smith DG, Fergason JR. Transtibial amputations. Clin Orthop. 1999;361:108–115. doi: 10.1097/00003086-199904000-00015. [DOI] [PubMed] [Google Scholar]