Abstract
This article summarises a comparative retrospective study (1983–2001) of 42 consecutive spastic–diplegic ambulatory patients (aged 2–10 years) by examining the radiographic and clinical results of two soft-tissue procedures for paralytic hip subluxation (PSH). Group A comprised 20 patients (26 PSHs) who were treated by iliopsoas tenotomy, and group B comprised 22 patients (31 PSHs) who were treated by rectus femoris and iliopsoas tenotomy with iliac crest resection (sartorius release). All patients had bilateral adductor tenotomies. At 8.8 years mean follow-up, group A migration percentages (MP) improved from 39.8% to 24.7% with 92.3% good/average results. At a mean follow-up period of 8.3 years, group B improved from 58.0% to 25.9% with 96.8% good/average results. Long-term hip reduction was achieved in 84.6% of group A and 80.6% of group B hips. Relative MP correction was superior in group B. No patient had MP progression in either the PSH or non-PSH hip. Walking ability improved in 55% of group A and 86% of group B patients (Functional Mobility Scale). In conclusion, we recommend release of all the principle hip flexors: rectus femoris, sartorius, and iliopsoas, coupled with adductor tenotomies, in this patient group.
Résumé
Une comparative rétrospective de 42 patients diplégiques spatiques mais ambulatoirs âgés de 2 à 10 ans a été réalisée entre 1983 et 2001 avec évaluation des résultats. Deux techniques de libération tissulaire étant pratiquées devant l’existence d’une sub-luxation paralytique de la hanche. Le groupe A (20 patients, 26 hanches PSHs) ont été traités par ténotomie de l’iliopsoas, dans le groupe B 22 patients, 31 PSHs ont été traités par ténotomie du droit antérieur, de l’iliopsoas avec résection de la crête iliaque libérant le sartorius. Tous les patients ont bénéficié également d’une ténotomie bilatérale des adducteurs. À 8,8 ans de suivi, dans le groupe A, le pourcentage de migration de la tête MP est amélioré de 39,8% à 24,7% avec 92,3% de bons résultats en moyenne alors que dans le groupe B, à 8,3 ans la sub-luxation est améliorée de 58,0% à 25,9% avec 96,8% de bons résultats. La réduction de la hanche est obtenue dans 84,6% des cas du groupe A et 80,6% des cas du groupe B. La correction de la migration de la tête est supérieure dans le groupe B, aucun patient n’a vu sa migration augmenter. La marche a été améliorée de 55% dans le groupe A, à 86% dans le groupe B. Nous recommandons la libération de tous les muscles fléchisseurs de la hanche: droit antérieur, sartorius, iliopsoas en association avec une ténotomie des adducteurs chez ce type de patients.
Introduction
Paralytic subluxation of the hip (PSH) occurs in patients with cerebral palsy (CP) because of a muscle imbalance between the stronger hip flexors and adductors and the weaker hip extensors and abductors. This imbalance causes joint contractures which then lead to migration of the femoral head out of the acetabulum, subsequently causing impairment to mobility, pelvic obliquity, and scoliosis [7]. The contribution of other factors to the development of PSH, such as a valgus femoral neck, increased femoral neck anteversion, pelvic obliquity and scoliosis, remains uncertain; some authors emphasise these factors, while others question their significance [4, 5, 7, 10, 17].
There is however a general consensus that soft tissue surgery should be performed in treating PSH in CP patients [3, 12]; however, success rates vary. The aim of surgery is to regain a more normal muscle balance, reduce the subluxed hip joint, and prevent recurrence of PSH. This paper compares the radiographic and clinical results of a standard soft tissue procedure for PSH in CP patients to that of a new and more extensive technique.
Patients and methods
This is a comparative retrospective study of 57 hips in 42 consecutive patients with cerebral palsy and PSH who were operated at the Institute for Orthopaedic Surgery "Banjica" in Belgrade, Serbia between 1983 and 2001. All patients met inclusion criteria of being able to walk independently with or without support, being aged between 2 and 10 years at the time of surgery, and with spastic diplegia and paralytic subluxation of one or both hips.
Subluxed hips were defined as having a Reimers migration percentage (MP) of greater than 33% [16]. We chose Reimers MP (which represents the percentage of the subluxed femoral head uncovered by the acetabulum) to be our radiological criterion because it is a widely accepted parameter in the assessment of PSH in CP patients [2, 21]. In addition, CP patients are often difficult to control during radiographic imaging, and hip rotation during imaging does not influence the final MP value, unlike other radiographic parameters [16]. The medical records and radiographs of these 42 patients were reviewed retrospectively. MP values for each patient were determined by two independent orthopaedic surgeons not affiliated to the unit, who were blinded to the performed procedures. The selected patients were then subdivided into two groups according to the surgical procedures performed.
Group A comprised 20 CP patients: 12 female and 8 male with 26 operated PSH hips. Six patients had both hips operated synchronously. All patients were ambulatory with spastic diplegia preoperatively. Mean age at the time of the surgery was 6.65 years (range 3–10 years). Mean postoperative follow-up was 8.8 years (range 3–16 years). Group A patients underwent iliopsoas tenotomies of the subluxed hip in addition to bilateral hip adductor tenotomies (adductor longus and gracilis). Two patients also underwent medial hamstring elongation (of gracilis, semitendinosus, semimembranosus) following the iliopsoas tenotomies; four patients required triceps surae elongation prior to iliopsoas tenotomies (three on the ipsilateral hip, and one bilateral hip) and one patient following iliopsoas tenotomy.
Group B comprised 22 CP patients: 9 female and 13 male with 31 operated PSH hips. Nine patients had both hips operated synchronously. All patients were ambulatory with spastic diplegia preoperatively. Mean age at the time of the surgery was 5.6 years (range 2–8 years). Mean follow-up was 8.3 years (range 4–18 years). Group B patients underwent rectus femoris tenotomy and iliac crest resection [8] in addition to iliopsoas tenotomy and bilateral hip adductor tenotomy. No other procedures were performed either before or after the hip surgery.
All patients had pre- and postoperative assessments (at final follow-up) of their walking abilities which were classified according to the Functional Mobility Scale (FMS) [6], in preference to the Gross Motor Function Classification System (GMFCS) [13]. The FMS is a performance measure that classifies mobility according to the need for assistive devices over the distances 5.50 and 500 metres (chosen to represent mobility in the home, at school, and in the wider community).
During the operation patients were positioned in a lateral position (lying on the nonoperative side). The anterior iliofemoral approach to the hip was used in all patients. Iliopsoas tenotomy was made approximately 3 cm proximal to the lesser trochanter insertion (at the point where the tendon was surrounded by the muscle belly); intramuscular tenotomy was performed with the purpose of also weakening the iliopsoas muscle. Those patients undergoing rectus femoris tenotomy had release of both the straight and reflected heads of the muscle. Iliac crest resection was made 2 cm below the anterior–superior iliac spine and continued posteriorly and superiorly to the junction of the middle and posterior thirds of the iliac crest. The iliac apophyses were then closed without tension, with the hips in a fully extended position [8], thus releasing sartorius.
Postoperatively, patients had both legs placed on skin traction for 3 weeks. Three patients in each group were also administered 2 mg of oral Tizanidine (Zanaflex, Elan Pharmaceuticals, USA) daily, to prevent spasticity during traction. The legs were positioned in abduction of 10–20° with 1–2.5 kg of weight on each limb. Traction was followed by a rehabilitation programme with an emphasis on vertical stance and weight bearing on the operated leg.
Reimers migration percentage was measured at some point during the 6 months before surgery, immediately after surgery, then once every 6 months for the first 3 years. Following this period, patients were reviewed annually. MP values at the most recent follow-up appointment were used for analyses. There was no statistically significant difference in age at the time of surgery between the 2 groups, and mean follow-up for all patients was 8.5 years.
Statistical evaluation of the results was made using Mann Whitney U and Wilcoxson testing where p values <0.05 were considered statistically significant.
Results
Mean preoperative values of MP were 39.8% in group A (range 34–64%), improving to a mean MP of 24.7% (range 13–100%) at final postoperative follow-up (p < 0.01) (Fig. 1). Two patients (2 hips) had an increase in the MP (Table 1), noted immediately postoperatively, which neither improved nor deteriorated over time. Eleven patients had improvement in their walking abilities. Three patients (5, 8, and 10) improved over 50 metres, with no improvement over 5 and 500 metres, while patient 4 improved over 500 metres, patient 11 improved over 5 and 500 metres, and 6 patients (2, 13, 14, 16, 17, and 20) improved over all three distances. Seven patients (1, 3, 6, 7, 9, 15, and 19) had no change over the three distances. Two patients had a deterioration in walking ability: patient 12 over 5 and 50 metres, and patient 18 over 500 metres (Table 2).
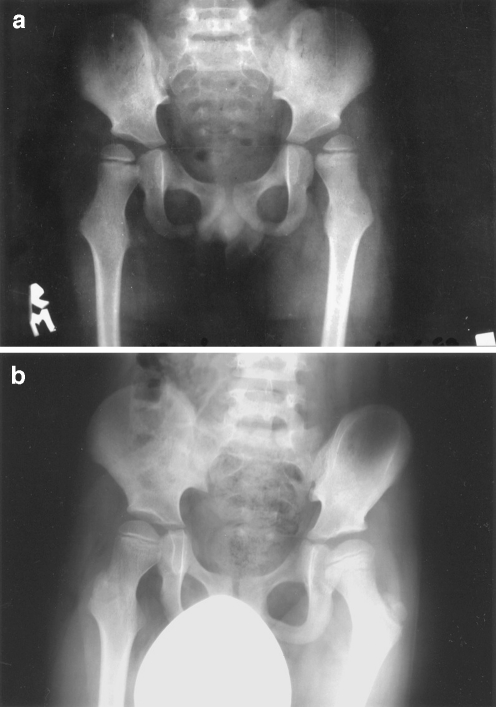
Fig. 1.
a Patient 15 (group A) with bilateral PSH preoperatively. b Patient 15 (group A) 4 years after iliopsoas and adductor tenotomy of both hips. Both hips are reduced
Table 1.
Group A and B cerebral palsy patient demographics including age at time of surgery, length of follow-up, and migration percentages (MP) before and at final postoperative follow-up
| Patient case number | Age (years) | MP before operation (percentage) | MP after operation (percentage) | Follow-up (years) | ||
|---|---|---|---|---|---|---|
| Right hip | Left hip | Right hip | Left hip | |||
| A 1 | 3 | 36 | 23 | 3 | ||
| A 2 | 7 | 34 | 13 | 5 | ||
| A 3 | 6 | 36 | 46 | 13 | 16 | 3 |
| A 4 | 4 | 37 | 22 | 3 | ||
| A 5 | 10 | 64 | 38 | 4 | ||
| A 6 | 10 | 40 | 34 | 5 | ||
| A 7 | 10 | 34 | 47 | 13 | ||
| A 8 | 10 | 50 | 100 | 6 | ||
| A 9 | 3 | 37 | 22 | 5 | ||
| A 10 | 7 | 43 | 16 | 4 | ||
| A 11 | 5 | 35 | 22 | 10 | ||
| A 12 | 4 | 34 | 40 | 22 | 19 | 12 |
| A 13 | 9 | 41 | 26 | 8 | ||
| A 14 | 6 | 36 | 50 | 19 | 30 | 5 |
| A 15 | 6 | 36 | 45 | 13 | 16 | 7 |
| A 16 | 5 | 50 | 40 | 27 | 29 | 9 |
| A 17 | 7 | 34 | 13 | 5 | ||
| A 18 | 6 | 34 | 19 | 8 | ||
| A 19 | 8 | 34 | 34 | 15 | 14 | 10 |
| A 20 | 7 | 34 | 14 | 5 | ||
| B 1 | 8 | 68 | 31 | 4 | ||
| B 2 | 6 | 60 | 34 | 18 | ||
| B 3 | 8 | 44 | 34 | 4 | ||
| B 4 | 7 | 43 | 16 | 6 | ||
| B 5 | 3 | 72 | 32 | 6 | ||
| B 6 | 7 | 34 | 14 | 13 | ||
| B 7 | 4 | 37 | 22 | 9 | ||
| B 8 | 3 | 72 | 32 | 12 | ||
| B 9 | 6 | 68 | 48 | 30 | 21 | 3 |
| B 10 | 7 | 61 | 79 | 22 | 16 | 4 |
| B 11 | 5 | 54 | 36 | 30 | 18 | 8 |
| B 12 | 3 | 87 | 62 | 19 | 61 | 8 |
| B 13 | 2 | 37 | 65 | 26 | 26 | 4 |
| B 14 | 5 | 75 | 21 | 5 | ||
| B 15 | 3 | 58 | 48 | 26 | 16 | 7 |
| B 16 | 6 | 60 | 32 | 7 | ||
| B 17 | 4 | 40 | 40 | 13 | 17 | 8 |
| B 18 | 7 | 43 | 16 | 13 | ||
| B 19 | 7 | 100 | 42 | 20 | 16 | 9 |
| B 20 | 6 | 80 | 39 | 4 | ||
| B 21 | 7 | 72 | 37 | 6 | ||
| B 22 | 8 | 68 | 44 | 31 | 34 | 9 |
Table 2.
Group A and B patient Functional Mobility Scales (FMS) grading 1–6 (range from wheelchair to independent on all surfaces) over three specific distances: 5, 50, and 500 metres
| Walking distance before operation | Walking distance after operation | |||||
|---|---|---|---|---|---|---|
| 5 m | 50 m | 500 m | 5 m | 50 m | 500 m | |
| Patient case number | Grade (1–6) | Grade (1–6) | Grade (1–6) | Grade (1–6) | Grade (1–6) | Grade (1–6) |
| A 1 | 2 | 1 | 1 | 2 | 1 | 1 |
| A 2 | 2 | 1 | 1 | 5 | 4 | 2 |
| A 3 | 5 | 5 | 4 | 5 | 5 | 4 |
| A 4 | 5 | 5 | 4 | 5 | 5 | 5 |
| A 5 | 2 | 1 | 1 | 2 | 2 | 1 |
| A 6 | 5 | 5 | 4 | 5 | 5 | 4 |
| A 7 | 5 | 4 | 4 | 5 | 4 | 4 |
| A 8 | 2 | 1 | 1 | 2 | 2 | 1 |
| A 9 | 5 | 5 | 4 | 5 | 5 | 4 |
| A 10 | 5 | 4 | 4 | 5 | 5 | 4 |
| A 11 | 4 | 4 | 1 | 5 | 4 | 4 |
| A 12 | 4 | 4 | 1 | 3 | 3 | 1 |
| A 13 | 3 | 1 | 1 | 4 | 4 | 4 |
| A 14 | 2 | 1 | 1 | 4 | 4 | 2 |
| A 15 | 4 | 4 | 4 | 4 | 4 | 4 |
| A 16 | 2 | 1 | 1 | 4 | 4 | 2 |
| A 17 | 3 | 2 | 1 | 4 | 4 | 2 |
| A 18 | 4 | 4 | 4 | 4 | 4 | 3 |
| A 19 | 5 | 5 | 4 | 5 | 5 | 4 |
| A 20 | 3 | 2 | 1 | 4 | 4 | 2 |
| B 1 | 2 | 1 | 1 | 2 | 2 | 2 |
| B 2 | 2 | 1 | 1 | 2 | 2 | 2 |
| B 3 | 2 | 1 | 1 | 2 | 2 | 2 |
| B 4 | 5 | 5 | 4 | 5 | 5 | 5 |
| B 5 | 4 | 2 | 1 | 5 | 4 | 4 |
| B 6 | 3 | 2 | 1 | 4 | 4 | 4 |
| B 7 | 4 | 2 | 1 | 4 | 4 | 4 |
| B 8 | 4 | 2 | 1 | 5 | 5 | 4 |
| B 9 | 5 | 5 | 4 | 5 | 5 | 4 |
| B 10 | 2 | 1 | 1 | 2 | 2 | 1 |
| B 11 | 2 | 2 | 1 | 3 | 3 | 2 |
| B 12 | 2 | 2 | 1 | 4 | 3 | 2 |
| B 13 | 3 | 2 | 1 | 4 | 2 | 2 |
| B 14 | 2 | 2 | 1 | 2 | 2 | 2 |
| B 15 | 4 | 2 | 1 | 4 | 4 | 4 |
| B 16 | 4 | 2 | 2 | 2 | 2 | 2 |
| B 17 | 4 | 2 | 1 | 4 | 2 | 2 |
| B 18 | 4 | 4 | 2 | 5 | 5 | 5 |
| B 19 | 2 | 2 | 1 | 4 | 2 | 1 |
| B 20 | 2 | 1 | 1 | 4 | 2 | 2 |
| B 21 | 3 | 2 | 1 | 2 | 2 | 2 |
| B 22 | 2 | 1 | 1 | 2 | 2 | 2 |
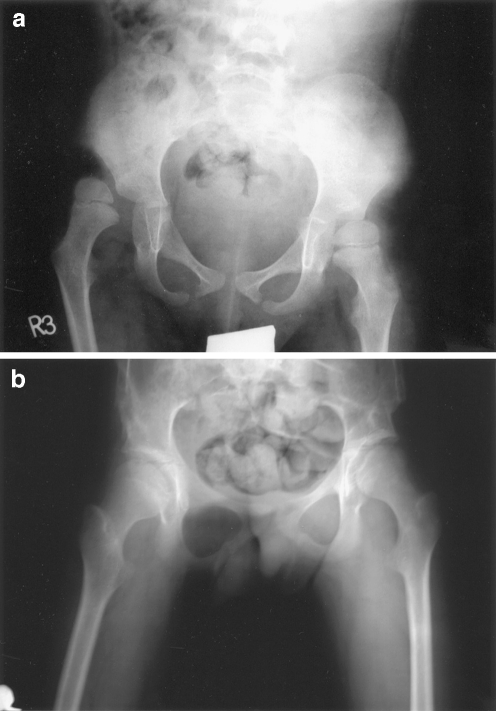
Mean preoperative values of MP were 58.0% in group B (range 34–100%), improving to a mean MP of 25.9% (range 13–61%) at most recent postoperative follow-up (p < 0.01) (Fig. 2). No patients had any increase in postoperative MP (Table 1).
Fig. 2.
a Patient 19 (group B) with right hip dislocation and PSH of the left hip preoperatively. b Patient 19 (group B) 6 years after bilateral iliac crest resection, flexor releases, and adductor tenotomies. Both hips are reduced
Nineteen patients had improvement in their walking abilities. Patient 10 improved over 50 metres, with no improvement over 5 and 500 metres. Six patients (1, 2, 3, 7, 15, and 22) improved over 50 and 500 metres, three patients (4, 14, and 17) improved over 500 metres, patients 13 and 19 improved over 5 and 500 metres, and seven patients (5, 6, 8, 11, 12, 18, and 20) improved over all three distances. One patient had no change over the three distances. Two patients had a deterioration in walking ability over 5 metres: patient 16 who remained unchanged over 50 and 500 metres, and patient 21 who also improved over 500 metres (Table 2).
There was a statistically significant difference in the preoperative values of MP (p < 0.01) between the two groups of patients, with greater MP values in group B (indicating greater levels of subluxation). There was no statistically significant difference in postoperative MP values between the two groups (p = 0.127). Hip reduction was not fully achieved in four hips (four patients) in group A and in six hips (six patients) in group B, where Reimers migration index remained 33% or greater postoperatively [16]. This gives overall maintained successful hip reduction rates of 84.6% for group A patients, and 80.6% for group B patients.
No significant hip migration was seen in the contralateral hips of patients with operated unilateral PSH.
Discussion
We are quite aware that our two patient groups are not fully homogenous and that group B patients had more severe levels of hip subluxation and lesser preoperative walking ability. However, it is difficult to have identically matched samples when comparing so few patients, even though this is, in fact, a fairly large CP case series. The mean preoperative group B MPs were significantly greater. Although six hips in six patients did not achieve full reduction (MP<33%), all group B patients had an improvement in MP postoperatively, with no hip subsequently dislocating, compared with group A, where 2 patients had worsening in MP following surgery.
Detailed analyses of our results showed that we had very good outcomes following procedures undertaken on both our CP patient groups, with rates of hip reduction of over 80%. To further standardise our results we have subdivided them into recognised MP ranges [11, 15]: good being an MP <33%, average an MP 33–39%, and poor an MP >39%. In group A, 22 hips (84.6%) had good results, two hips (7.7%) average results, and two hips (7.7%) poor results; hence, 92.3% had good/average results. In group B, 25 hips (80.6%) had good results, five hips (16.1%) average results, and one hip (3.2%) poor results; hence, 96.8% had good/average results. This compares very favourably with the literature, where success rates are variable and claims range from 67–80% [1, 3, 9, 11, 15, 18, 19].
With regards to the FMS assessment, 55% of patients in group A had an improvement in walking ability, with 35% improving at all three distances; 10% of patients had deterioration in walking ability (Table 2). In group B, 86% of patients had improvement in walking ability, 32% at all three distances, and 9% had some deterioration in mobility (Table 2). Hence, it appears that greater improvements in walking ability were achieved in group B patients.
We acknowledge that our patients were all spastic diplegics and ambulatory preoperatively, both of which are factors related to more positive outcomes [15]; however, we observed no deterioration in MP in our patients during the 8.5-year mean follow-up period in the operated PSH hips, which once again compares favourably to similar patient groups already published. A recent study of 76 PSH hips in 41 CP spastic diplegic patients undergoing only adductor tenotomy found that, at 3 years, over half had developed radiographic progression in hip subluxation [14]. The two group A patients who suffered an increase in MP did so immediately postoperatively and had no deterioration or improvement over the follow-up period.
We also observed that no patient had progressive subluxation of their “normal” nonsubluxed hip over the mean 8.5 year follow-up period after undergoing adductor tenotomy. We are hesitant to draw any conclusions from this, however, this appears contrary to findings in quadriplegic CP patients undergoing prophylactic adductor tenotomies where 58% still had progressive PSH [20].
Most of the literature describes releases of either hip adductors alone, or in combination with the iliopsoas muscle [1, 3, 9, 11, 12, 14, 15, 18– 20]. To our knowledge the release of rectus femoris with iliac crest resection, in addition to iliopsoas tenotomy and bilateral hip adductor tenotomy, has not previously been described. Though there was no statistically significant difference in postoperative MP value between the two patient groups, we feel that the operative release of all the principle hip flexors in addition to adductors, as performed in group B patients, is a more effective procedure (Fig. 2a and b), because it addresses more of the potential deforming forces acting on the hip, appears to lead to greater improvements in FMS, and appears to achieve higher levels of hip reduction.
Footnotes
No competing interests or funding declared in connection with this study.
References
- 1.Barrie J, Galasco C. Surgery for unstable hips in cerebral palsy. J Pediatr Orthop. 1996;5(4):225–331. doi: 10.1097/01202412-199605040-00002. [DOI] [PubMed] [Google Scholar]
- 2.Bleck E. Orthopaedic management in cerebral palsy. Philadelphia: Blackwell Scientific ; 1987. [Google Scholar]
- 3.Bleck E. Management of the lower extremities in children who have cerebral palsy. J Bone Joint Surg. 1990;72-A:140–144. [PubMed] [Google Scholar]
- 4.Christoforo F, Taddonio R, Gelb R. The effect of correction of spinal deformity and pelvic obliquity in hip stability in neuromuscular disease. Orthop Trans. 1983;7:557. [Google Scholar]
- 5.Fabry G, McEwen G, Shands A. Torsion of the femur. J Bone Joint Surg. 1973;55-A:1726–1738. [PubMed] [Google Scholar]
- 6.Graham HK, Harvey A, Rodda J, et al. The Functional Mobility Scale (FMS) J Pediatr Orthop. 2004;24(5):514–520. doi: 10.1097/00004694-200409000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Hodgkinson I, Berard C, Chotel F, et al. Pelvic obliquity and scoliosis in non-ambulatory patients with cerebral palsy: a descriptive study of 234 patients over 15 years of age. Rev Chir Orthop Reparatrice Appar Mot. 2002;88(4):337–341. [PubMed] [Google Scholar]
- 8.Ingram AJ. Paralytic disorders. In: Crenshaw AH, editor. Campbell’s operative orthopaedics, vol 4. 7. St Louis: C.V. Mosby; 1987. pp. 2987–2989. [Google Scholar]
- 9.Kalen V, Bleck E. Prevention of spastic paralytic dislocation of the hip. Develop Med Child Neurol. 1985;27:17–24. doi: 10.1111/j.1469-8749.1985.tb04520.x. [DOI] [PubMed] [Google Scholar]
- 10.Michele AA. Iliopsoas. 1. Springfield, Illinois: Charles C. Thomas; 1962. [Google Scholar]
- 11.Miller F, Cardoso Dias R, et al. Soft-tissue release for spastic hip subluxation in cerebral palsy. J Pediatr Orthop. 1997;17(5):571–584. doi: 10.1097/00004694-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Moreau M, Cook P, Ashton B. Adductor and psoas release for subluxation of the hip in children with spastic cerebral palsy. J Pediatr Orthop. 1995;15(5):672–676. doi: 10.1097/01241398-199509000-00024. [DOI] [PubMed] [Google Scholar]
- 13.Palisano R, Rosenbaum P, Walter S, et al. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- 14.Pap K, Kiss S, Vizkelety T, et al. Open adductor tenotomy in the prevention of hip subluxation in cerebral palsy. Int Orthop. 2005;29(1):18–20. doi: 10.1007/s00264-004-0610-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Presedo A, Oh CW, Dabney KW, et al. Soft-tissue releases to treat hip subluxation in children with cerebral palsy. J Bone Joint Surg Am. 2005;87(4):832–841. doi: 10.2106/JBJS.C.01099. [DOI] [PubMed] [Google Scholar]
- 16.Reimers J. The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand (Suppl) 1980;134:1–97. doi: 10.3109/ort.1980.51.suppl-184.01. [DOI] [PubMed] [Google Scholar]
- 17.Samilsion R, Tsou P, Aamoth G, et al. Dislocation and subluxation of the hip in cerebral palsy. J Bone Joint Surg. 1972;54-A:863–873. [PubMed] [Google Scholar]
- 18.Sharrard W. Paralytic deformity in the lower limb. J Bone Joint Surg. 1967;49-B:731–747. [PubMed] [Google Scholar]
- 19.Spruit M, Fabry G. Psoas and adductor release in children with cerebral palsy. Acta Orthop Belg. 1997;63(2):91–93. [PubMed] [Google Scholar]
- 20.Turker RJ, Lee R. Adductor tenotomies in children with quadriplegic cerebral palsy: longer term follow-up. J Pediatr Orthop. 2000;20(3):370–374. doi: 10.1097/00004694-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 21.Vidal J, Deguillaume P, Vidal M. The anatomy of the dysplastic hip in cerebral palsy related to prognosis and treatment. Int Orthop. 1985;9:105–110. doi: 10.1007/BF00266951. [DOI] [PubMed] [Google Scholar]