Abstract
The objective of this study was to assess the outcome of operations on acetabular fractures from a developing country in the presence of locally available facilities. Sixty-three acetabular fractures were assessed at an average follow up of 52.94 months after operation. Twenty-six patients operated upon in the first three years and 37 operated thereafter were separately studied to discover the effect of the learning curve. Regarding the fractures, 47 of 63 (74.6%) had excellent/good results (Harris Hip Score>80). The complications included broken drill bit in eight patients (12.69%), deep infection and heterotopic ossification in five patients (7.93%), avascular necrosis and sciatic nerve palsy in two patients (3.17%) and implant failure in one patient (1.58%). The results collected during the learning curve were inferior in the complex fractures (p value<0.001). Complications were common in patients opting for local implants and in those operated after over 2 weeks delay.
Résumé
Le but de ce travail est d’évaluer le traitement des fractures de l’accétabulum dans un pays développé. Matériel et méthode : 63 fractures de l’accétabulum ont été suivies en moyenne pendant 52,94 mois. 26 patients ont été opérés dans les trois premières années de notre expérience et les 37 autres patients opérés trois ans après que nous ayons commencé ce type de traitement, ceci afin d’évaluer de façon séparée les effets de notre courbe d’apprentissage. 47 sur 63 (74,6%) ont eu un excellent/bon résultat avec un score de Harris supérieur à 80. Les complications ont été les suivantes : 8 fractures de mèches (12,69%), 5 infections profondes (7,93%) et 7 ossifications hétérotypiques (7,93%), 2 nécroses de la tête fémorale et 2 paralysies sciatiques (3,17%) une dans chaque groupe. Enfin, un débricolage chez un patient (1,58%). Les résultats selon la courbe d’apprentissage sont moins bons dans des fractures complexes (p < 0.001) en début de pratique. Les complications sont plus habituelles chez les patients ayant bénéficié de la mise en place d’implants ou chez ceux opérés après 2 semaines de délai.
Introduction
The treatment of displaced fractures of the acetabulum has changed. The conservative treatment of these fractures has been shown to give inferior results compared to operative treatment [10]. Open reduction and the internal fixation of displaced acetabular fractures, as for any intra-articular fracture, is a widely accepted mode of treatment [11, 18, 20]. Acetabular surgery is difficult due to its complex operative anatomy. Variables such as initial injury to the articular surface, residual intra-articular step, lost vascularity to the femoral head etc. define the ultimate outcome, including degenerative changes in the hip joint [25, 26].
With the overall increase in high-energy injuries, the number of complex acetabular fractures has increased in Third World countries. In order to obtain better results, it is recommended that trauma centres should designate a group of surgeons who will consistently treat these fractures [5]. In the absence of such specialised and dedicated acetabular surgery centres in developing countries, the majority of such fractures are either treated conservatively or operated on by general trauma surgeons. Due to the lack of computed tomography (CT) scanning facilities at many centres, the surgeons rely upon plain radiography for working out the operative plan. The non-existence of an organised health insurance sector forces the surgeon to use low-cost locally produced instruments and implants. Patients hailing from peripheral areas present to the operative centres usually after significant delays.
In recent years in India, the increased load of such fractures has coerced younger surgeons to take up such cases without any formal exposure to acetabular surgery, mainly relying on basic surgical techniques and the backing of the international literature. The older generation of surgeons generally believed in treating these fractures conservatively.
At our centre, we started operating upon displaced acetabular fractures in 1997. During this period, we saw almost all varieties of the reported acetabular fractures. In addition, we came across some rare and unusual fractures. The purpose of this retrospective study is to assess our results of operatively treating the displaced acetabular fractures in the Third World setting in the presence of the above mentioned factors.
Material and methods
Out of a total number of 68 patients operated upon from 1997 to 2003, 63 patients were available for assessment at a minimum follow up of 3 years. The average follow up was 52.94 months (range 37–96 months).
After initial resuscitation and clinical assessment, specific pre-operative investigations included plain radiography with anteroposterior (AP) and Judet (iliac oblique and obturator) views of the pelvis. CT scanning was only performed in those patients who could afford its cost. The fractures were classified according to the Letournel and Judet classification [17]. The indications for surgery included fracture displacement >2 mm, intra-articular fragments, posterior joint instability and the need for reconstruction for future total hip replacement. The operations were performed through single or combined standard approaches, as per the pre-operative plan. No agents for the prevention of heterotopic ossification or thromboembolism were given.
The patients were followed up clinically and radiographically with all three views at 6 weeks, 3 months, 6 months, 1 year and then yearly thereafter. The functional results were evaluated by the Harris hip score [7].
Results
The average age was 38.4 years (range 19–68 years). Twenty-one patients (33.3%) reported with an average delay of 20.46 days (range 13–25 days). The average time from injury to surgery was 12.33 days (range 4–30 days). Forty-four patients were operated upon within two weeks of injury. One patient was treated on the 96th day due to delayed presentation. Fifteen fractures (23.8%) were simple, while 48 (76.19%) fractures were associated/complex fractures. Thirty-six injuries were associated with both column and posterior wall-transverse fractures.
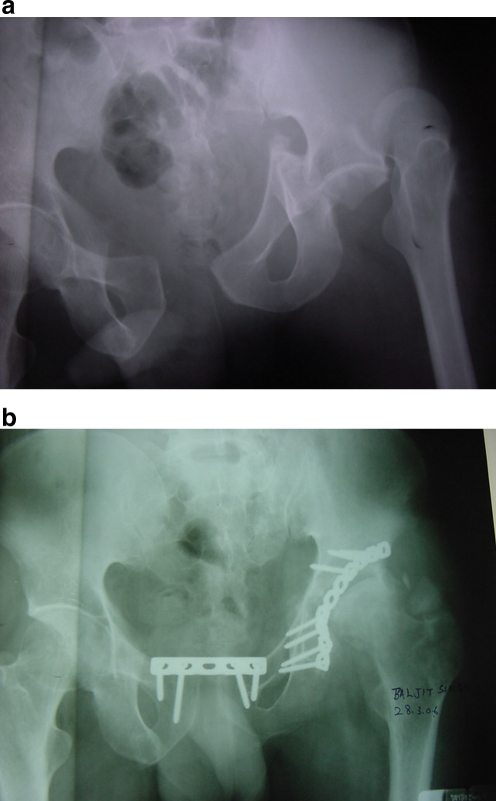
Amongst the rare presentations, a 24-year-old patient presented with floating acetabulum and had an unusual transverse acetabular fracture with locked dislocated femoral head combined with pubic diastasis (Fig. 1a). At 36 months follow up, both of the fractures had healed but the femoral head showed features of avascular necrosis and there was radiological evidence of heterotopic ossification (Fig. 1b).
Fig. 1.
a Pre-operative and b final follow up X-ray of a transverse acetabular fracture with posterior dislocation of the femoral head and pubic diastasis. Note the floating ischiopubic fragment. Note also avascular necrosis and mysositis in b
In 33 patients (52.38%), a locally manufactured low-cost implant was used.
The surgical approaches used included Kocher-Langenbeck in 30 cases (47.6%), ilio-inguinal in 14 cases (22.2%), triradiate in six cases (9.5%), extended ilio-femoral in two cases (3.2%) and combined Kocher-Langenbeck+ilio-femoral in 11 cases (17.5%). The average duration of surgery in the patients operated after more than 2 weeks of injury was 235 min, while in the patients operated earlier than 2 weeks of injury, it was 186.4 min. The average number of transfused units of blood in the former was 3.1 and in the latter was 2.2.
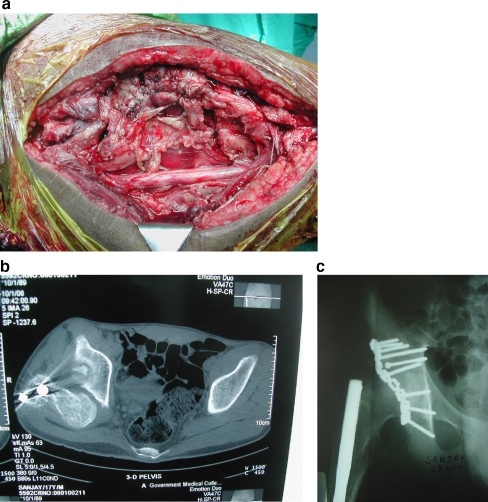
One patient suffered non-union of the acetabular fracture with broken plate (Fig. 2).
Fig. 2.
Broken plate with non-union of the fracture. Note the broken drill bit
The drill bit was broken in eight cases (12.69%).
Supplementary skin traction for 3–4 weeks was given to seven patients.
Detailed radiological and functional results are given in Table 1. In 48 (76.19%) cases, congruent reduction and in 15 (23.8%) cases, incongruent reduction was achieved. Functionally, 80% (12 out of 15) of the simple acetabular fractures and 72.91% (35 out of 48) of the complex associated type of fracture had a Harris hip score >80 (labelled as excellent/good).
Table 1.
Radiological and functional results
| Overall results | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| PW (5) | PC (4) | AW (1) | AC (3) | Tr (2) | T type (6) | PW+PC (3) | PW+T (14) | A+PT (3) | BC (22) | Total | |
| Radiographic results | |||||||||||
| Congruent | 5 | 4 | 1 | 2 | 1 | 4 | 2 | 11 | 2 | 16 | 48 |
| Non-congruent | 0 | 0 | 0 | 1 | 1 | 2 | 1 | 3 | 1 | 6 | 15 |
| Functional results | |||||||||||
| Excellent | 2 | 2 | 1 | 2 | 0 | 2 | 1 | 5 | 1 | 11 | 27 |
| Good | 2 | 2 | 0 | 0 | 1 | 1 | 1 | 5 | 1 | 7 | 20 |
| Fair | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 2 | 1 | 2 | 9 |
| Poor | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 2 | 0 | 2 | 7 |
PW=posterior wall; PC=posterior column; AW=anterior wall; AC=anterior column; Tr=transverse; BC=both columns
Five patients (7.93%) each developed deep infection and heterotopic ossification. Two (3.17%) patients had avascular necrosis of the femoral head.
Two patients had iatrogenic sciatic nerve palsy; one patient showed complete recovery at 3 months, while the other recovered partially.
For the purpose of discovering the effect of the learning curve on our results, we arbitrarily divided our study in two halves, i.e. the first 3 years, labelled as early cases, and the last 3 years, labelled as late cases (Table 2). The average operating time in the early cases and the late cases was 242.33 min and 158.42 min, respectively. The average amount of blood transfused in the former was 3.6 units and in the latter was 2.6 units. Statistically, the results of the complex cases operated in the late cases group were significantly better than the early cases group (p value<0.001 for both parameters); simple cases did not show a significant difference.
Table 3.
Comparison with published results
Discussion
Fractures of the acetabulum remain an enigma for the orthopaedic surgeon [21]. This 10-year-old statement is still applicable in the developing world, due to the lack of technical expertise and inadequate infrastructure. The trend is, however, changing because of the easy access of information technology and the international literature. The standardisation of clinico-radiological evaluation, fracture classification, surgical approaches and fixation techniques of displaced acetabular fractures has resulted in achieving the goal of preserving a functional, mobile and painless hip joint [17, 21].
It is an accepted fact that the functional results of the displaced acetabular fractures correlate well with the quality of reduction and that open reduction is the best method to achieve congruity [3, 10, 11, 13, 15, 18, 20, 21, 23, 27]. In our series also, radiographic congruity (76.19%) correlated well with the function (74.6%) (Table 1). The quality of reduction in our study decreased with the increase in the complexity of the acetabular fracture. Radiologically, 86.66% (13 out of 15) of simple fractures and 72.91% (35 out of 48) of complex fractures had congruent reduction. Correlating well with the congruity, 80% (12 out of 15) of the simple fractures and 72.91% (35 out of 48) of the complex fractures had excellent/good function (Harris Hip Score>80). Overall, 74.6% of our patients had excellent/good results (Harris Hip Score>80). Table 3 compares our results with the other reported series [4, 5, 8, 14, 21, 22, 24].
Table 2.
Comparison of radiological and functional evaluation between the early and late operated cases
| Simple fracture | Complex fracture | ||
|---|---|---|---|
| (No. of patients) | (No. of patients) | ||
| Radiological evaluation | |||
| Congruent | Early cases | 8 | 8 |
| Late cases | 5 | 27 | |
| Non-congruent | Early cases | 0 | 10 |
| Late cases | 2 | 3 | |
| Functional evaluation | |||
| Excellent/good | Early cases | 7 | 8 |
| Late cases | 5 | 28 | |
| Fair/poor | Early cases | 1 | 10 |
| Late cases | 2 | 2 | |
The most common approach used by us was that of Kocher-Langenbeck in about half of the patients (47.6%). In the early phase of our learning curve, probably due to greater familiarity with this approach only, it was used more commonly, even in some complex fractures, when we used to supplement the complex fractures by skin traction for 3–4 weeks because there was no anterior fixation. Gradually, as we became accustomed to the acetabular anatomy, we shifted to the ilio-inguinal approach for anterior wall/column fractures. Lately, all complex bicolumnar fractures requiring bicolumnar fixation were managed by a combined approach undertaken during single-stage surgery.
We believe that the anterior opening of the pelvic ring in the case of a floating acetabulum (Fig. 1a) is not associated with injury to the anterior interossious sacroiliac ligaments, which is, otherwise, a standard pathology associated with pubic diastasis. This pathology in the floating acetabulum is substituted with the displacement at the fractured acetabulum as the force is spent at the acetabular fracture; during surgery, reducing the acetabular fracture lead to a spontaneous reduction of the pubic diastasis, which was then stabilised with a plate (Fig. 1b).
During surgery, the drill bit was broken in eight patients (12.91%). All of the broken drill bits were locally manufactured and were broken during the drilling in the supra acetabular area above the pelvic brim (Fig. 2). Lately, we have been using 2.5-mm K wire for drilling the holes in this area instead of a drill bit and we are now able to avoid this complication.
Five patients (7.93%) had heterotopic ossification. The use of osteotomies, the amount of subperiosteal stripping and the severity of fracture predisposes to heterotopic ossification [1, 6, 12]. Two of the five patients with heterotopic ossification had a complex fracture anatomy, while the remaining three had presented to us at 15, 18 and 90 days of injury, resulting in the delayed operative intervention, leading to more handling and stripping of tissue at surgery. We now routinely use prophylactic indomethacin 75 mg twice daily for 4 weeks in the patients operated after a delay of more than 2 weeks.
In our series, the infection rate was 7.93%, which was higher than reported in other studies (0–3%) [2, 9, 19, 24]. Of these patients, 80% (4 out of 5) were operated upon during our learning curve period. In three patients, the indigenously produced cheaper implants had been used. All of these patients were treated more than 2 weeks after injury (15, 16, 18, 22 and 28 days). Of these, two had been operated by a tri-radiate approach, two with extended ilio-femoral approach and one with the Kocher-Langenbeck approach. One patient was operated with a combined approach that developed deep infection in the posterior wound. Four patients made complete recovery after wound debridement and antibiotics. A 56-year-old diabetic, treated via an ilio-inguinal approach on the 28th day of injury, underwent debridement for deep infection at 4 weeks of surgery. At 1 year follow up, the routine X-ray showed non-union of the fracture with sclerosed margins and broken plate (Fig. 2). The other factor of failure in this patient may be attributed to the use of a cheaper locally made implant. In India, due to the lack of an organised insurance sector, the cost of the implant is bourne by the patients. Although as a matter of routine we offer to the patients implants manufactured by internationally accepted manufacturers, yet, in some patients, we use the locally made more affordable implants.
The incidence of avascular necrosis was quite low in our series (2 of 63), probably because, during the posterior approach, we approach the fractured acetabular fragment from the iliac/ischial side. The capsule is only opened if reduction is not achievable without opening the capsule or, pre-operatively, there is evidence of an intra-articular loose bony fragment. We feel, however, that the minimum follow up in our study being 26 months, there may be some patients who develop radiological evidence of avascular necrosis at a later stage.
Two patients developed iatrogenic sciatic nerve injury, which recovered partially with time. A 20-year-old labourer with posterior fracture dislocation was treated on the 24th day after injury due to late presentation. Probably, excessive traction during reduction or the pressure of a Hohman retractor in the greater sciatic notch resulted in concussion to the nerve. The patient showed complete recovery at 3 months. The other patient had suffered a posterior fracture dislocation, along with fracture of the shaft of the femur. His femoral shaft fracture was treated by intramedullary nailing outside our institution 3 months earlier when closed reduction was performed for acetabular fracture. At 2 months, the patient underwent open reduction for the persistent unreduced dislocation by the same surgeon. After the second operation, the patient developed a foot drop. At a total of 3 months after injury (one month after second operation), the dislocation was still seen to be unreduced associated with persistent foot drop. The patient was referred to us at this time. CT scan of the patient (Fig. 3b) showed a dislocated femoral head posteriorly and an intra-articular fragment. The missed intra-articular fragment at the time of the previous surgery was probably the cause of the unreduced dislocation. At surgery, we found fibrosis in the tissue planes and it took us time to dissect the sciatic nerve (Fig. 3a). Finally, at 48 months follow up, the patient had zero power in extensor hallucis longus and grade 3 power in the other dorsiflexors, while the plantar flexors were unaffected. Radiologically, the fracture had uneventful healing (Fig. 3c).
Fig. 3.
a Intact sciatic nerve in neglected unreduced dislocated head with previous surgery resulting in sciatic nerve injury. b Pre-operative CT scan showing intra-articular fragment and dislocated femoral head. c Final follow up X-ray of the same patient
The surgical treatment of acetabular fractures, in the cases presenting late after the accident, is difficult but, nevertheless, possible. The total joint replacement, if needed subsequently, in such cases is much simpler [16]. We found that complications like sciatic nerve palsy and heterotopic ossification, as well as infection, were more commonly observed in the patients who were operated upon after a delay of more than 2 weeks. Brueton [3] reported that the results were inferior if the patients were treated with an average delay of 17 days after the injury and recommended a rapid referral to a regional centre with the necessary facilities and expertise to manage displaced acetabular fractures.
Additionally, we observed that the patients in whom locally manufactured implants and drill bits were used suffered a higher rate of complications, such as broken drill bits (all eight cases), broken plate (only one case) and infection (3 of the 5 cases). Thus, we feel that the patients presenting late and being operated after a delay of over 2 weeks, and the patients opting for low-cost locally manufactured implants should be informed about the higher risk of these complications at the time of giving their consent.
In conclusion, the operative treatment of displaced acetabular fractures gives universally satisfactory results. The surgeons should prepare well for problems such as prolonged operating time and increased blood loss, more so in the learning curve phase and in the patients operated after a delay of over 2 weeks. Time spent on a thorough study of the radiographs and a proper pre-operative plan helps to outline an appropriate surgical approach and the appropriate type of implant. A higher risk of complication should be explained to the patients opting for low-cost locally manufactured implants and to the patients undergoing surgery after a delay of over 2 weeks. In addition, health planners should be apprised of the need for provision of high-quality implants to all patients, irrespective of their socio-economic status.
References
- 1.Bosse MJ, Poka A, Reinert CM, Ellwanger F, Slawson R, McDevitt ER. Heterotopic ossification as a complication of acetabular fracture. Prophylaxis with low-dose irradiation. J Bone Joint Surg Am. 1988;70(8):1231–1237. [PubMed] [Google Scholar]
- 2.Brooker AF, Bowerman JW, Robinson RA, Riley LH. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55(8):1629–1632. [PubMed] [Google Scholar]
- 3.Brueton RN. A review of 40 acetabular fractures. The importance of early surgery. Injury. 1993;24(3):171–174. doi: 10.1016/0020-1383(93)90285-E. [DOI] [PubMed] [Google Scholar]
- 4.Deo SD, Tavares SP, Pandey RK, El-Saied G, Willett KM, Worlock PH. Operative management of acetabular fractures in Oxford. Injury. 2001;32:581–586. doi: 10.1016/S0020-1383(00)00200-X. [DOI] [PubMed] [Google Scholar]
- 5.Fica G, Cordova M, Guzman L, Schweitzer D. Open reduction and internal fixation of acetabular fractures. Int Orthop. 1998;22(6):348–351. doi: 10.1007/s002640050275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghalambor N, Matta JM, Bernstein L. Heterotopic ossification following operative treatment of acetabular fracture: an analysis of risk factors. Clin Orthop Relat Res. 1994;305:96–105. doi: 10.1097/00003086-199408000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 8.Heeg M, Klasen HJ, Visser JD. Operative treatment for acetabular fractures. J Bone Joint Surg Br. 1990;72(3):383–386. doi: 10.1302/0301-620X.72B3.2341432. [DOI] [PubMed] [Google Scholar]
- 9.Helfet DL, Schmeling GJ. Management of complex acetabular fractures through single nonextensile exposures. Clin Orthop Relat Res. 1994;305:58–68. doi: 10.1097/00003086-199408000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Hesp WL, Goris RJ. Conservative treatment of fractures of the acetabulum. Results after long-term follow-up. Acta Chirurg Belg. 1988;88:27–32. [PubMed] [Google Scholar]
- 11.Holdsworth FW. Dislocation and fracture-dislocation of the pelvis. J Bone Joint Surg Br. 1948;30B:461–466. [PubMed] [Google Scholar]
- 12.Kaempffe FA, Bone LB, Border JR. Open reduction and internal fixation of acetabular fractures: heterotopic ossification and other complications of treatment. J Orthop Trauma. 1991;5(4):439–445. doi: 10.1097/00005131-199112000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Kebaish AS, Roy A, Rennie W. Displaced acetabular fractures: long-term follow-up. J Trauma. 1991;31(11):1539–1542. doi: 10.1097/00005373-199111000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Kumar A, Shah NA, Kershaw SA, Clayson AD. Operative management of acetabular fractures. A review of 73 fractures. Injury. 2005;36:605–612. doi: 10.1016/j.injury.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 15.Latenser BA, Gentilello LM, Tarver AA, Thalgott JS, Batdorf JW. Improved outcome with early fixation of skeletally unstable pelvic fractures. J Trauma. 1991;31(1):28–31. doi: 10.1097/00005373-199101000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Letournel E. Surgical repair of acetabular fractures more than three weeks after injury, apart from total hip replacement. Int Orthop. 1978;2(4):305–313. doi: 10.1007/BF00571814. [DOI] [Google Scholar]
- 17.Letournel E, Judet R, Elson RA. Fractures of the acetabulum. 2. Berlin Heidelberg New York: Springer; 1993. [Google Scholar]
- 18.Letournel E. Fractures of the acetabulum: a study of a series of 75 cases. Clin Orthop Relat Res. 1994;305:5–9. doi: 10.1097/00003086-199408000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Liebergall M, Mosheiff R, Low J, Goldvirt M, Matan Y, Segal D. Acetabular fractures. Clinical outcome of surgical treatment. Clin Orthop Relat Res. 1999;366:205–216. doi: 10.1097/00003086-199909000-00027. [DOI] [PubMed] [Google Scholar]
- 20.Matta JM, Mehne DK, Roffi R. Fractures of the acetabulum: early results of a prospective study. Clin Orthop Relat Res. 1986;205:241–250. [PubMed] [Google Scholar]
- 21.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–1645. [PubMed] [Google Scholar]
- 22.Mayo KA. Open reduction and internal fixation of fractures of the acetabulum. Results in 163 fractures. Clin Orthop Relat Res. 1994;305:31–37. [PubMed] [Google Scholar]
- 23.Pennal GF, Davidson J, Garside H, Plewes J. Results of treatment of acetabular fractures. Clin Orthop Relat Res. 1980;151:115–123. [PubMed] [Google Scholar]
- 24.Rommens PM, Broos PL, Vanderschot P. Preparation and technique for surgical treatment of 225 acetabulum fractures. 2 year results of 175 cases (in German) Unfallchirurg. 1997;100(5):338–348. doi: 10.1007/s001130050128. [DOI] [PubMed] [Google Scholar]
- 25.Tile M. Fractures of the acetabulum. In: Schatzker J, Tile M, editors. Rationale of operative fracture care. 2. Berlin Heidelberg New York: Springer; 1996. [Google Scholar]
- 26.Tornetta P, Mostafavi HR. Hip dislocation: current treatment regimens. J Am Acad Orthop Surg. 1997;5(1):27–36. doi: 10.5435/00124635-199701000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Ward DA, Bircher MD. The early management of pelvic and acetabular fractures. Injury. 1996;27(Suppl 1):S-A24–S-A28. doi: 10.1016/0020-1383(96)83791-0. [DOI] [PubMed] [Google Scholar]