Abstract
Frequently, the imaging features of stress fractures may be misinterpreted as tumour-like lesions. The aim of this study was to analyse the quality of different examinations in detecting stress fractures mimicking tumour-like lesions in magnetic resonance imaging (MRI). We evaluated 22 cases which were referred to our department with the suspected diagnosis of bone tumours turning out to be stress fractures. Whenever the MRI did not lead to a diagnosis after a second review, computed tomography (CT) scans and, if still required, additional examinations were performed until the fracture was detected. A stress fracture was diagnosed in 15 cases after the additional CT scan, in five cases with the review of the MRI and in two cases with a combination of several examinations. Especially in stress fractures of the tibia and the femur, CT scanning was essential for making a diagnosis by detecting the fracture line. Bone scans and biopsies, in contrast, were not helpful in making a correct diagnosis.
Résumé
de façon fréquente les images de fractures de fatigue peuvent être interprétées comme des images pseudo tumorales. Pour cette étude nous avons analysé ce type de lésions à l’aide de l’IRM. Nous avons suivi 22 cas, de tumeur osseuse faisant penser à des fractures de fatigue. Chaque fois, l’IRM ne nous a pas permis de faire le diagnostic après un second examen. Le scanner a été également nécessaire ainsi que d’autres examens pour affirmer le diagnostic de fractures. une fracture de fatigue a été diagnostiquée dans 15 cas après un scanner additionnel, dans 5 cas après avoir revu l’IRM et dans 2 cas avec une combinaison de plusieurs examens. pour une fracture de fatigue du tibia et du fémur, le scanner est un examen essentiel par contre la biopsie n’apporte pas d’aide au diagnostic.
Introduction
A stress fracture is caused by repetitive overloading of a bone, exceeding its mechanical capacity. Two groups can be distinguished: fatigue fractures, which develop by excessive loads in normal bones, and insufficiency fractures, with normal loads acting upon bones with reduced mechanical properties [3, 19]. Pathological fractures in tumour lesions may, hence, be seen as a form of insufficiency fractures.
Stress fractures may occur as an accumulation of microdamage when the overload persists during the phase of bone weakening [22]. This fits well with some studies describing the first appearance of symptoms, for example, in fresh military recruits, between 10 and 12 days after the beginning of training [20].
The most important diagnostic study is a plain radiograph in two planes. However, in early stages, the sensitivity may be as low as 10%, rising to 30–70% at follow-up [12]. The first radiographic feature is the “grey cortex sign,” an area of decreased density in the cortex [17]. Later, localised periosteal reactions are frequent indicators for stress fractures [3].
If plain radiographs appear normal, most authors advise magnetic resonance imaging (MRI), as a number of studies have shown that MRI has a high sensitivity and specificity [5, 6, 8]. To increase the diagnostic value of T1- and T2-weighted images, the examination should be complemented by short inversion time inversion recovery (STIR) and fat-suppressed T2-weighted images [1, 2]. A staging system, as described by Fredericson et al. [7], can be used. But even with MRI, it is, in some cases, difficult to differentiate stress fractures from infections, bone infarctions or neoplastic lesions (such as osteosarcoma or Ewing sarcoma) [2, 18].
In this study, we analysed diagnostically difficult stress fractures mimicking tumour-like lesions in plain radiographs and MRI. The aim was to determine the sensitivity of additional examinations in detecting the stress fracture.
Methods
We retrospectively evaluated 22 cases. All of these patients were referred to the Orthopaedic Oncology department by general practitioners and orthopaedic surgeons between 1 January 2004 and 31 December 2006 with the diagnosis of a tumour or a tumour-like lesion. As an inclusion criterion, all patients had pain as the first symptom and had already undergone plain radiographs and an MRI. Some additional examinations (computed tomography [CT] scans, scintigraphies and biopsies) were also performed before admission. There were no exclusion criteria defined.
At the time of presentation, all examinations were reviewed by the senior author (H.-R. D) and an experienced skeletal radiologist (A. B-M). Whenever the diagnosis remained uncertain, additional studies, beginning with CT scans (if not already performed) and followed by bone scans and biopsies, were performed.
Results
The average age of the 22 patients (17 women, 5 men) was 47.9 years (range 6–80 years). In ten cases, the lesion was located in the pelvis (45.5%), in seven patients in the tibia (31.8%) and in five cases in the femur (22.7%). The ten patients (9 f, 1 m) with pelvic lesions (six sacrum, two pubic bone, one sciatic bone and one acetabulum) had an average age of 63.9 years. The average age of the seven patients (4 f, 3 m) with tibial involvement was 30.3 years. The five patients (3 f, 2 m) with a femoral stress fracture had an average age of 40.4 years.
In addition to the radiographs and the MRI, three CT scans, five scintigraphies and two biopsies had been performed prior to the referrals. In addition, we performed 16 CT scans, two scintigraphies and one biopsy. The key to the diagnosis was a CT scan in 15 cases (68.2%), a review of the MRI in five cases (22.7%) and in two cases (9.1%), a combination of several studies. This reveals a sensitivity of 78.9% for the CT scan. The seven scintigraphies did not lead to the exclusion of any differential diagnosis (sensitivity of 0%). In total, three patients had a biopsy performed, excluding a tumour in all of these cases. But this examination did not lead to the diagnosis of a stress fracture (for example, by showing callus formation).
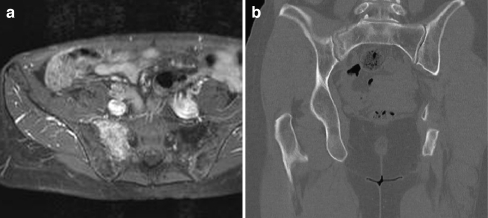
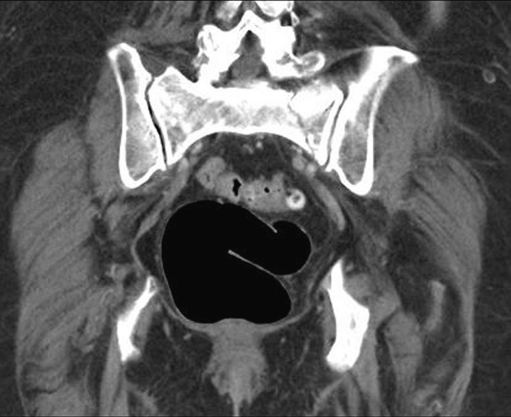
To further evaluate the value of the different imaging methods, the diagnostic imaging tool was linked to the site of involvement. The ten pelvic stress fractures could be identified by MRI in three cases, in five cases with CT scans and in two cases by a combination of examinations (see Figs. 1 and 2). Regarding the tibia, the clue to the diagnosis was CT in six cases. In one case, an MRI examination was sufficient for reaching a diagnosis (see Fig. 3). For the diagnosis of a femoral stress fracture, MRI was sufficient in one case and in four other cases, a CT scan was helpful.
Fig. 1.
a A 59-year-old female patient having pain with a history of breast cancer. The T1-w fat sat post contrast shows circumscribed gadolinium enhancement suspicious of metastasis. b The computed tomography (CT) scan could identify the fracture line
Fig. 2.
A 68-year-old female with acute onset of low back pain one month prior to presentation. The CT scan shows the insufficiency fracture of the sacrum
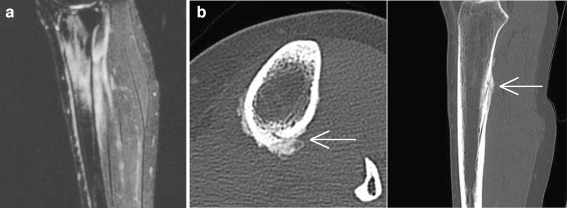
Fig. 3.
a Sagittal short inversion time inversion recovery (STIR) sequence of the lower leg of a 24-year-old female having pain in the lower left leg for 2 months after taking up jogging. Diffuse hyperintensity in the marrow of the proximal tibia as well as in the surrounding soft tissues. A fracture line could not be detected. b In the same patient, the fracture line and callus formation (arrow) in the thin-layer CT (scan) revealed the diagnosis of stress fracture
Discussion
The stress fractures included in this study were uncommon cases in which the diagnosis was unclear. They represent pre-selected cases that were referred to us after a general practitioner or an orthopaedic surgeon had diagnosed a tumour in the initial MRI.
The fact that only 22 of these cases were referred to our centre over a period of 3 years reflects the literature, stating that most stress fractures can be clearly identified using MRI [2, 18]. In five cases, a second review of the MRI was able to exclude neoplastic processes and diagnose the fracture.
The distribution of the involved bones was similar to the literature. Regarding stress fractures of the lower extremity, the tibia was, according to other studies, the most frequently affected bone [13]. Especially, the posterior medial shaft is a preferred location (see Fig. 3b) [16]. The stress fractures in the femur and in the pelvis were also as described in the literature [11, 12, 21].
If MRI alone was not sufficient, additional studies were necessary. In our series, CT scanning proved to be the most sensitive additional imaging method. In 15 of the 19 (78.9%) performed CT scans, the fracture line could be detected and a stress fracture was diagnosed. Regarding only the 16 cases in which CT scanning was performed in our hospital (after excluding five cases by the review of all MRI scans), the sensitivity was 93.8%. In two of the four cases in which the CT scan alone could not identify the fracture, a combined review of the MRI and the CT scan was successful.
After having localised the lesion in MRI, we could focus the CT scan on a small region of interest, hence, radiation exposure was reduced. Similar to the literature, high-resolution multislice CT and multiplanar reconstructions turned out to be very helpful in depicting the fracture lines. According to other studies, CT scanning had the highest diagnostic value in stress fractures of the femur and the tibia [6]. Since, according to the literature, the sensitivity of CT regarding all stress fractures without preselection is lower than that of MRI and bone scintigraphy, its role remains mainly limited to excluding other diagnoses [15].
In contrast, bone scintigraphy has a relatively high sensitivity in the early stages, since a tracer uptake may be seen already 6–72 h after the onset of symptoms [10]. In later stages of stress fractures, the decreasing sensitivity of bone scintigraphy could be improved by performing a single photon emission computed tomography (SPECT) [9]. But comparable to the low specificity stated in the literature, we could not exclude differential diagnoses in any case by bone scanning alone [4, 14]. If a suspected stress fracture could not be identified by MRI, a bone scan gave no additional information.
The same held true for biopsies. Since the histological examinations could not identify the stress fracture, we would perform a biopsy only in very rare cases to exclude a neoplastic lesion, as recommended by Lassus et al. [13]. In some cases, a biopsy of the callus can affect fracture healing and may be misinterpreted as a neoplastic process [12].
In summary, we recommend radiographs followed by MRI if the radiographs show no pathological findings. In cases where MRI does not show the stress fracture, a CT scan (with thin-layer imaging) was most helpful. Bone scans or biopsies did not enhance the diagnostic accuracy in these difficult cases. An accurate clinical assessment remains very important.
References
- 1.Ahovuo JA, Kiuru MJ, Kinnunen JJ, Haapamaki V, Pihlajamaki HK. MR imaging of fatigue stress injuries to bones: intra- and interobserver agreement. Magn Reson Imaging. 2002;20(5):401–406. doi: 10.1016/S0730-725X(02)00514-3. [DOI] [PubMed] [Google Scholar]
- 2.Anderson MW, Greenspan A. Stress fractures. Radiology. 1996;199(1):1–12. doi: 10.1148/radiology.199.1.8633129. [DOI] [PubMed] [Google Scholar]
- 3.Daffner RH, Pavlov H. Stress fractures: current concepts. AJR Am J Roentgenol. 1992;159(2):245–252. doi: 10.2214/ajr.159.2.1632335. [DOI] [PubMed] [Google Scholar]
- 4.Fayad LM, Kamel IR, Kawamoto S, Bluemke DA, Frassica FJ, Fishman EK. Distinguishing stress fractures from pathologic fractures: a multimodality approach. Skeletal Radiol. 2005;34(5):245–259. doi: 10.1007/s00256-004-0872-9. [DOI] [PubMed] [Google Scholar]
- 5.Fayad LM, Kawamoto S, Kamel IR, Bluemke DA, Eng J, Frassica FJ, Fishman EK. Distinction of long bone stress fractures from pathologic fractures on cross-sectional imaging: how successful are we? AJR Am J Roentgenol. 2005;185(4):915–924. doi: 10.2214/AJR.04.0950. [DOI] [PubMed] [Google Scholar]
- 6.Feydy A, Drapé J, Beret E, Sarazin L, Pessis E, Minoui A, Chevrot A. Longitudinal stress fractures of the tibia: comparative study of CT and MR imaging. Eur Radiol. 1998;8:598–602. doi: 10.1007/s003300050442. [DOI] [PubMed] [Google Scholar]
- 7.Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23(4):472–481. doi: 10.1177/036354659502300418. [DOI] [PubMed] [Google Scholar]
- 8.Gaeta M, Minutoli F, Scribano E, Ascenti G, Vinci S, Bruschetta D, Magaudda L, Blandino A. CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology. 2005;235(2):553–561. doi: 10.1148/radiol.2352040406. [DOI] [PubMed] [Google Scholar]
- 9.Garcés GL, González-Montoro I, Rasines JL, Santonja F. Early diagnosis of stress fracture of the lumbar spine in athletes. Int Orthop. 1999;23(4):213–215. doi: 10.1007/s002640050353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanstrup IL. Bone scintigraphy in sports medicine: a review. Scand J Med Sci Sports. 1997;7:322–330. doi: 10.1111/j.1600-0838.1997.tb00161.x. [DOI] [PubMed] [Google Scholar]
- 11.Kiuru MJ, Pihlajamäki HK, Ahovuo JA. Fatigue stress injuries of the pelvic bones and proximal femur: evaluation with MR imaging. Eur Radiol. 2003;13(3):605–611. doi: 10.1007/s00330-002-1562-4. [DOI] [PubMed] [Google Scholar]
- 12.Kiuru MJ, Pihlajamäki HK, Ahovuo JA. Bone stress injuries. Acta Radiol. 2004;45(3):317–326. doi: 10.1080/02841850410004724. [DOI] [PubMed] [Google Scholar]
- 13.Lassus J, Tulikoura I, Konttinen YT, Salo J, Santavirta S. Bone stress injuries of the lower extremity: a review. Acta Orthop Scand. 2002;73(3):359–368. doi: 10.1080/000164702320155392. [DOI] [PubMed] [Google Scholar]
- 14.Markey KL. Stress fractures. Clin Sports Med. 1987;6:405–425. [PubMed] [Google Scholar]
- 15.Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes. A study of 320 cases. Am J Sports Med. 1987;15:46–58. doi: 10.1177/036354658701500107. [DOI] [PubMed] [Google Scholar]
- 16.Milgrom C, Giladi M, Stein M, Kashtan H, Margulies JY, Chisin R, Steinberg R, Aharonson Z. Stress fractures in military recruits. A prospective study showing an unusually high incidence. J Bone Joint Surg Br. 1985;67(5):732–735. doi: 10.1302/0301-620X.67B5.4055871. [DOI] [PubMed] [Google Scholar]
- 17.Mulligan ME. The “gray cortex”: an early sign of stress fracture. Skeletal Radiol. 1995;24(3):201–203. doi: 10.1007/BF00228923. [DOI] [PubMed] [Google Scholar]
- 18.Pauleit D, Sommer T, Textor J, Flacke S, Hasan C, Steuer K, Emous D, Schild H. MRI diagnosis in longitudinal stress fractures: differential diagnosis of Ewing sarcoma. Rofo. 1999;170(1):28–34. doi: 10.1055/s-2007-1011003. [DOI] [PubMed] [Google Scholar]
- 19.Pentecost RL, Murray RA, Bridley HH. Fatigue, insufficiency, and pathologic fractures. JAMA. 1964;28(187):1001–1004. doi: 10.1001/jama.1964.03060260029006. [DOI] [PubMed] [Google Scholar]
- 20.Scully TJ, Besterman G. Stress fracture—a preventable training injury. Mil Med. 1982;147(4):285–287. [PubMed] [Google Scholar]
- 21.Soubrier M, Dubost JJ, Boisgard S, Sauvezie B, Gaillard P, Michel JL, Ristori JM. Insufficiency fracture. A survey of 60 cases and review of the literature. Joint Bone Spine. 2003;70(3):209–218. doi: 10.1016/S1297-319X(03)00024-1. [DOI] [PubMed] [Google Scholar]
- 22.Sterling JC, Edelstein DW, Calvo RD, Webb R., 2nd Stress fractures in the athlete. Diagnosis and management. Sports Med. 1992;14(5):336–346. doi: 10.2165/00007256-199214050-00005. [DOI] [PubMed] [Google Scholar]