Abstract
The purpose of this study was to review the association between compensation status and surgical outcome especially of the shoulder. Given the high prevalence of shoulder injuries in the workplace and the large proportion of workers compensation (WC) claims involving such injuries, it is worth examining the correlation between WC status and surgical outcome of the shoulder. All studies published in journals (MEDLINE and PubMed) from 1980 through 2007 on surgical interventions performed on the shoulder in which workers compensation status was documented and the postoperative functional outcome was compared according to that status were pooled for meta-analysis. This systematic review shows that compensation status of an individual receiving shoulder surgery is a consistent positive predictor of poor functional outcome. The majority of questions posed in the most commonly adopted shoulder-specific functional outcome measurement tools were subjective in nature and may account for part of the phenomenon.
Résumé
Analyser l’effet du statut d’accident du travail sur les résultats de la chirurgie au niveau de l’épaule. Etant donnée la fréquence élevée des traumatismes de l’épaule sur le lieu de travail et la part importante de demandes d’indemnisation chez les travailleurs avec ce type de blessures, il est intéressant d’étudier la corrélation entre le statut accident du travail et les résultats de la chirurgie de l’épaule. Toutes les études publiées dans les journaux médicaux (MEDLINE et PUBMED) de 1980 à 2007 concernant des interventions réalisées au niveau de l’épaule dans lesquelles le statut accident du travail était documenté et le résultat post opératoire étudié en fonction de ce statut ont été réunis pour une méta analyse. Cette revue systématique montre que le statut accident du travail d’un individu opéré de l’épaule est un facteur prédictif d’un mauvais résultat. La majorité des questions posées dans les tests spécifiques de l’épaule les plus couramment utilisés sont de nature subjective et cela pourrait expliquer en partie ce phénomène.
Introduction
It has been well documented that workers’ compensation (WC) status is a positive predictor of poor postoperative functional outcome [1–3, 6, 8–10, 12, 14, 16–20, 22, 25, 28, 30, 32–35, 38, 39, 41, 42, 44]. Between the 1940s and 2005 numerous publications have incorporated patients’ WC status into subgroup analyses of therapeutic interventions. Particularly in surgical procedures, many of such studies have shown statistically significant differences in the relief of pain, the patient’s subjective satisfaction, the patient’s ability to return to normal activities of daily living, and return-to-work time between WC and non-WC individuals.
Amongst the articles in which workers’ compensation status was recorded, the three most common anatomical sites involved were the lumbar spine, shoulder, and carpel tunnel [15].
Ergonomically speaking, it is also expected that shoulder injuries can result from a wide range of occupations. Based on published evidence, occupations which involve poor work posture and repetitions are the most likely to cause shoulder injuries [5, 13]. The mechanisms causing shoulder tendonitis include a high intramuscular pressure in the rotator cuff which impedes microcirculation, causing inflammation and later degeneration [21], as well as actual tears in the subacromial tendons when they are squeezed between the humerus and acromial arch during overhead arm movements [29]. According to an extensive review by Bernard in 1997, the threshold angle after which shoulder injury occurs is 60 degrees of flexion [4].
Although the specific biomechanical risk factors and thresholds for injury in the workplace are difficult to quantify [4], we are nonetheless well aware that associations do exist between shoulder injuries and occupations with high repetition, high force requirements, and lack of pauses [13]. Using an index designed to rank industries according to their WC claims over 8 years, Silverstein et al. showed that within the top five industries responsible for compensable nontraumatic soft-tissue musculoskeletal disorders in Washington state, rotator cuff injuries ranked second only to carpel tunnel syndrome (CTS) in terms of upper extremity claims incidence rates [40], with CTS on a statistically significant downward trend and rotator cuff injuries remaining stable. Rotator cuff injuries in this study were defined as inflammation, degeneration, and tear of the supraspinatus, infraspinatus, and subscapularis tendons. These results imply that we may be seeing proportionally more and more of these shoulder injuries in the workplace. Some of the other occupations that frequently give rise to shoulder injuries include machinists, car mechanics, and house painters [43].
Given the high prevalence of shoulder injuries in the workplace and the large proportion of workers’ compensation claims involving such injuries, our group thought it would be worthwhile to review all studies on shoulder surgery in which the workers’ compensation status of the patient was recorded and then recalculate the correlation between WC status and surgical outcome. This review also documents the original shoulder-specific score used by the primary investigators. We believe this is important since a good proportion of shoulder-specific tests are based on subjective questioning, and without tests specifically designed to delineate the psychosocial causes of shoulder pain and function (such as the Waddell’s nonorganic physical signs for low-back pain [45], or the nerve conduction studies for nerve entrapment syndromes), the use of these tests may lead to convenient over reporting of pain and under reporting of functional abilities.
Our hypothesis is that WC status will continue to be a positive predictor of poor outcome of shoulder surgery.
Eligible studies
All studies published in journals from 1980 through 2007 on surgical interventions performed on the shoulder in which worker’s compensation status was documented and the postoperative functional outcome was compared according to that status were eligible for our meta-analysis. We accepted studies in all languages. Official translations were sought whenever required. Each study had to provide data on at least one compensated and one uncompensated patient.
We included all types of surgical interventions on the shoulder and shoulder girdle, open or arthroscopic, including debridement procedures. There was no minimum requirement for follow-up period. Studies describing surgical outcomes that were not for each patient individually (i.e. dichotomous scores) but for patient groups were included in the review process, but their raw figures could not be extracted; hence, these studies were not included in statistical calculations.
Worker’s compensation status was defined as the patient’s legal status as a worker’s compensation claimant at the time of surgery through the time of assessment of functional outcome, but was not limited by the verdict of the legal process.
Postoperative functional outcome was documented as satisfactory or unsatisfactory as originally reported by the principal investigator(s) of the reviewed articles, regardless of the original shoulder-specific scores used. Following the classification system usually adopted in meta-analytical studies on postoperative outcome, scores of “excellent” or “good” were classified as satisfactory, and outcomes labelled as “fair”, “poor”, or “failure” were classified as unsatisfactory.
Search strategy
To identify studies published between 1980 and 2007, we performed an electronic database search using MEDLINE and PubMed.
The search strategy used the following keywords for compensation: “workers’ compensation” and “compensation and redress”; for shoulder surgery, the following keywords were used: “shoulder”, “acromioplasty”, “subacromial decompression”, “rotator cuff”, and “scapula”. Unpublished articles and indexed articles which have not been published yet were excluded from the analysis. Details of the search strategy are available from the authors.
Additional studies were identified by manual searching on the references lists of selected retrieved articles for additional publications that did not appear in our original search results.
Two investigators responsible for the review process independently selected articles for inclusion based on title and abstract, if one of both investigators considered the article as potentially eligible the full article was reviewed by both investigators. Each article was reviewed by two investigators and discrepancies in inclusion/exclusion criteria were resolved by discussion.
Extracted data included: year of publication, study design, type of surgery, number of patients, number of shoulders, worker’s compensation status, postoperative functional outcome, and the original shoulder-specific score used by the principal investigators. Only published data were considered in this meta-analysis.
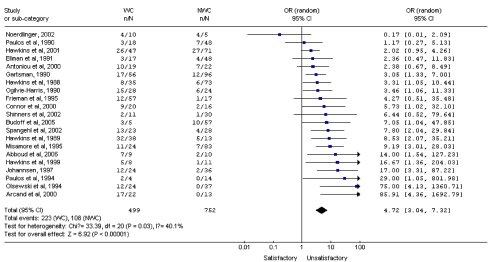
Cochrane Review Manager software version 4.2 was used to analyse the data. Data was entered by one investigator and checked by another. Odds ratio and 95% confidence intervals were calculated for dichotomous outcomes. The results were then examined for heterogeneity by examining the forest plot with random-effects model, and thereafter funnel plots were used to look for publication bias.
Results
The MEDLINE and PubMed searches yielded 24,506 studies, and we further identified 341 studies from the reference lists of retrieved articles. The final number of complete articles for review was 28 studies [1–3, 6, 8–10, 12, 14, 16–20, 22, 25, 28, 30–35, 38, 39, 41, 42, 44], all of which were reports on shoulder surgery and which included workers’ compensation status as part of the subgroup analyses.
There was one randomised controlled trial [42], seven prospective studies [2, 8, 10, 20, 25, 30, 41], and 20 retrospective case series [1, 3, 6, 9, 12, 14, 16–19, 22, 28, 31–35, 38, 39, 44]. Due to the nature of the subject being studied, randomisation for compensation status was not possible, and the only randomised controlled trial (performed by Spangehl) was for open versus arthroscopic acromioplasty (Table 1).
Table 1.
Characteristics of studies included
| Study | Year | Dichotomous data | No. of cases | WC | NWC | Shoulder score used |
|---|---|---|---|---|---|---|
| Abboud | 2006 | Y | 19 | 9 | 10 | PENN |
| Antoniou | 2000 | Y | 41 | 19 | 22 | SST |
| Arcand | 2000 | Y | 35 | 22 | 13 | UCLA |
| Budoff | 2005 | Y | 62 | 5 | 57 | UCLA, SST |
| Chen | 2007 | N | 70 | 5 | 65 | ASES |
| Connor | 2000 | Y | 36 | 20 | 16 | ASES |
| Ellman | 1991 | Y | 65 | 17 | 48 | Modified UCLA |
| Frieman | 1995 | Y | 74 | 57 | 17 | ASES |
| Gartsman | 1990 | Y | 152 | 56 | 96 | ASES |
| Hawkins | 1988 | Y | 108 | 35 | 73 | Questionnaire |
| Hawkins | 1989 | Y | 51 | 38 | 13 | No objective test |
| Hawkins | 1999 | Y | 19 | 8 | 11 | No objective test, mostly subjective questioning |
| Hawkins | 2001 | Y | 118 | 47 | 71 | ASES |
| Iannotti | 1996 | N | 40 | 24 | 16 | Constant score |
| Johannsen | 1997 | Y | 60 | 24 | 36 | Constant score |
| Misamore | 1995 | Y | 107 | 24 | 83 | UCLA |
| McKee | 2000 | N | 71 | 23 | 48 | SST, SPADI, SSRS, M-ASES, SSI |
| Nicholson | 2003 | N | 106 | 40 | 66 | SST, ASES |
| Noerdlinger | 2002 | Y | 15 | 10 | 5 | SST, ASES, Constant Murley, Rowe, SF-36 |
| Ogilvie-Harris | 1990 | Y | 52 | 28 | 24 | NA |
| Olsewski | 1994 | Y | 61 | 24 | 37 | UCLA, Neer |
| Paulos | 1990 | Y | 66 | 18 | 48 | Questionnaire |
| Paulos | 1994 | Y | 18 | 4 | 14 | UCLA |
| Sallay | 2005 | N | 321 | 155 | 166 | ASES |
| Shinners | 2002 | Y | 41 | 11 | 30 | UCLA |
| Smith | 2000 | N | 191 | 44 | 147 | SST, SF-36 |
| Spanghel | 2002 | Y | 51 | 23 | 28 | UCLA |
| Viola | 2000 | N | 1063 | 335 | 728 | SST, SF-36 |
| Total no. of cases | 3113 | 1125 | 1988 | |||
| Total no. of cases for meta-analysis | 499 | 752 |
WC workers’ compensation, NWC nonworkers’ compensation, ASES American Shoulder and Elbow Surgeons rating scale, SST simple shoulder test, UCLA University of California Los Angeles score, SF-36 SF-36 Health Survey, PENN University of Pennsylvania shoulder score, Neer Neer shoulder score, Rowe Rowe shoulder score, NA not available
The primary outcome of this meta-analysis is odds-ratio for an unsatisfactory outcome in patients with workers’ compensation status compared with patients without workers’ compensation status.
The total number of cases recorded in these 28 studies was 3,133 amongst which 1,125 were WC and 1,988 were non-WC. Of the 28 studies, only one described a negative correlation between WC status and poor surgical outcome. Seven studies [8, 20, 25, 30, 38, 41, 44] provided no dichotomous scores, leaving 499 WC and 752 non-WC patients that could be pooled for comparison. Of the seven studies that provided no dichotomous scores, all of them showed a positive correlation between WC status and poor surgical outcome. The summary OR for an unsatisfactory outcome in WC patients was 4.72 (95% CI, range 3.04–7.32). The results for each study and the overall estimate are shown as a forest plot in Fig. 1.
Fig. 1.
Forest plot of random-effects odds rations (ORs) and 95% confidence intervals (CIs) for each study in the meta-analysis
In terms of the types of operations performed, there were nine studies for acromioplasties or other shoulder arthroplasties [8, 9, 12, 14, 16, 17, 30, 32, 42], eight for rotator cuff repairs [6, 18, 20, 25, 28, 35, 39, 41], seven for shoulder decompression [3, 9, 10, 19, 22, 33, 34], two for all types of shoulder operations [38, 44], one each for treatment of scapula winging and os acromiale [1], and one for capsulolabral augmentation [2].
The most frequently used shoulder-specific scores were the University of California at Los Angeles (UCLA) score (eight studies), the American Shoulder and Elbow Surgeons Rating Scale (ASES) (nine studies), and the Simple Shoulder Test (SST) (seven studies).
Discussion
This systematic review and meta-analysis of all surgical literature concerning shoulder operations showed a strong association between workers’ compensation status and poor outcome after shoulder surgery. The association was consistent and maintained for all types of compensation and for all but one surgical intervention reported.
The findings are consistent with previous meta-analytic studies on the effect of compensation status on the outcome after surgery in general [15].
Sixteen of the 21 studies included in the meta-analysis portion of this review showed a statistically significant correlation between workers’ compensation status and poor surgical outcome, with four more showing a positive but not statistically significant correlation. The remaining one study by Noerdlinger, published in 2002, showed a negative correlation, but the result was not statistically significant. The study reporting a negative correlation was the only article of the 21 reporting surgery which was not on the glenohumeral joint or the rotator cuff. All seven studies included in the review but not in the meta-analysis reported a positive correlation.
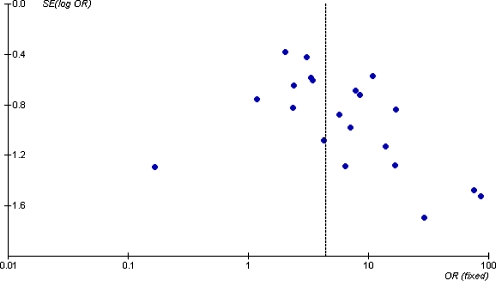
The selective reporting of this type of study has been previously commented upon by Harris et al. in their 2005 meta-analysis of all surgical interventions [15]. Their results suggested that bias could be present as a result of selective publication of studies showing an association or the selective reporting of an association only when it exists. If present, this may lead to an increased estimate of the association [7, 23]. The result of reporting only positive cases was examined by Harris and his group by comparing studies that were specifically designed to assess the compensation effect, to those that were not. It was shown that a difference was present but was small and not statistically significant. A funnel plot of the odds ratios for all studies in the meta-analysis portion of this study also reveals a mild degree of bias in the data representation in the published literature (Fig. 2).
Fig. 2.
Funnel plot of the odds ratios for all studies in the meta-analysis
The behaviour of conscious or unconscious exaggeration of severity of illness has been demonstrated previously [11], and in chronic low back pain, it has been shown that compensation involvement may have an adverse effect on self-reported pain, depression, and disability before and after rehabilitation interventions [36]. Although the three most frequently used scores in this review—the UCLA, ASES, and SST—have demonstrated good reliability, validity, and responsiveness [26, 27, 37], little has been done to explore the functional and psychological aspects of the shoulder. When the components of these rating scales are examined closely, the inadequacies becomes evident. For example, the SST is based on 12 subjective yes/no questions on pain and function, and the ASES is based on one question on subjective pain (5% of total score), 15 questions on subjective function (60% of total score), four questions on strength (20% of total score), and three on stability (15% of total score) in various directions and muscles to be completed by the therapist/physician. Also, the UCLA pain scale is based on one question on subjective pain (28.6% of total score), one on subjective function (28.6% of total score), one on range of motion (active only), one on strength, and one on subjective satisfaction (14.3% of total score for each). This type of scoring that incorporates primarily subjective reporting may lead to convenient overreporting of pain, and underreporting of function, including the active range of motion (Table 2). We also perceive the reporting of strength as not objective since there is no reliable way to discriminate between a submaximal effort and a maximal/best effort. The effect of litigation may also have bearing on how these questions are answered in a pain questionnaire [24].
Table 2.
The number of objective questions out of all questions in three different shoulder-specific scores
| Score | SST | ASES | UCLA |
|---|---|---|---|
| Strict objective component (max objective score/total score) | 0/12 | 15/100 | 0/35 |
Conclusion
This systematic review shows that compensation status of an individual receiving shoulder surgery continues to be a positive predictor of poor functional outcome. All but one of the 28 articles selected for this review demonstrated a negative correlation between WC status and poor outcome. Due to the nature of the parameter being studied, only observational data were available, and may account for publication and/or selection bias. The majority of questions posed in the most commonly adopted shoulder-specific functional outcome measurement tools were subjective in nature and may account for part of the phenomenon.
Footnotes
An erratum to this article can be found at http://dx.doi.org/10.1007/s00264-008-0652-6
References
- 1.Abboud JA, Silverberg D, Pepe M, Beredjiklian PK, Iannotti JP, Williams GR, et al. Surgical treatment of os acromiale with and without associated rotator cuff tears. J Shoulder Elbow Surg. 2006;15(3):265–270. doi: 10.1016/j.jse.2005.08.024. [DOI] [PubMed] [Google Scholar]
- 2.Antoniou J, Duckworth DT, Harryman DT., II Capsulolabral augmentation for the management of posteroinferior instability of the shoulder. J Bone Jt Surg Am. 2007;82-A(9):1220–1230. doi: 10.2106/00004623-200009000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Arcand MA, O’Rourke P, Zeman CA, Burkhead WZ., Jr Revision surgery after failed subacromial decompression. Int Orthop. 2000;24:61–64. doi: 10.1007/s002640000124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bernard BP (1997) Musculoskeletal disorders and workplace factors: a critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. National Institute for Occupational Safety and Health, Center for Disease Control and Prevention, Atlanta, GA, USA
- 5.Buckle PW, Devereux JJ. The nature of work-related neck and upper limb musculoskeletal disorders. Appl Ergon. 2002;33:207–217. doi: 10.1016/S0003-6870(02)00014-5. [DOI] [PubMed] [Google Scholar]
- 6.Budoff JE, Rodin D, Ochiai D, Nirschl RP. Arthroscopic rotator cuff debridement without decompression for the treatment of tendinosis. Arthroscopy. 2005;21(9):1081–1089. doi: 10.1016/j.arthro.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 7.Callaham ML, Wears RL, Weber EJ, Barton C, Young G. Positive-outcome bias and other limitations in the outcome of research abstracts submitted to a scientific meeting. JAMA. 1998;280(3):254–257. doi: 10.1001/jama.280.3.254. [DOI] [PubMed] [Google Scholar]
- 8.Chen AL, Bain EB, Horan MP, Hawkins RJ. Determinants of patient satisfaction with outcome after shoulder arthroplasty. J Shoulder Elbow Surg. 2007;16(1):25–30. doi: 10.1016/j.jse.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 9.Connor PM, Yamaguchi K, Pollock RG. Comparison of arthroscopic and open revision decompression for failed anterior acromoplasty. Orthopedics. 2000;23(6):549–554. doi: 10.3928/0147-7447-20000601-11. [DOI] [PubMed] [Google Scholar]
- 10.Ellman H, Kay SP. Arthroscopic subacromial decompression for chronic impingement. J Bone Jt Surg Br. 1991;73-B(3):395–398. doi: 10.1302/0301-620X.73B3.1670435. [DOI] [PubMed] [Google Scholar]
- 11.Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain disability exaggeration/malingering and submaximal effort research. Clin J Pain. 1999;5(4):244–274. doi: 10.1097/00002508-199912000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Frieman BG, Fenlin JM. Anterior acromioplasty: effect of litigation and workers’ compensation. J Shoulder Elbow Surg. 1995;4(3):175–181. doi: 10.1016/S1058-2746(05)80048-5. [DOI] [PubMed] [Google Scholar]
- 13.Frost P, Bonde JPE, Mikkelsen S, Andersen JH, Fallentin N, Kaergaard A, et al. Risk of shoulder tendinitis in relation to shoulder loads in monotonous repetitive work. Am J Ind Med. 2002;41:11–18. doi: 10.1002/ajim.10019. [DOI] [PubMed] [Google Scholar]
- 14.Gartsman GM. Arthroscopic acromioplasty for lesions of the rotator cuff. J Bone Jt Surg. 1990;72(2):169–180. [PubMed] [Google Scholar]
- 15.Harris I, Mulford J, Solomon M, vanGelder JM, Young J. Association between compensation status and outcome after surgery. JAMA. 2005;293(13):1644–1652. doi: 10.1001/jama.293.13.1644. [DOI] [PubMed] [Google Scholar]
- 16.Hawkins RJ, Brock RM, Abrams JS, Hobeika P. Acromioplasty for impingement with an intact rotator cuff. J Bone Jt Surg. 1988;70-B(5):795–797. doi: 10.1302/0301-620X.70B5.3192582. [DOI] [PubMed] [Google Scholar]
- 17.Hawkins RJ, Chris T, Bokor D, Kiefer G. Failed anterior acromioplasty: a review of 51 cases. Clin Orthop Relat Res. 1989;243:106–111. [PubMed] [Google Scholar]
- 18.Hawkins RJ, Morin WD, Bonutti PM. Surgical treatment of full-thickness rotator cuff tears in patients 20 years of age or younger. J Shoulder Elbow Surg. 1999;8(3):259–265. doi: 10.1016/S1058-2746(99)90139-8. [DOI] [PubMed] [Google Scholar]
- 19.Hawkins RJ, Plancher KD, Saddemi SR, Brezenoff LS, Moor JT. Arthroscopic subacromial decompression. J Shoulder Elbow Surg. 2001;10(3):225–230. doi: 10.1067/mse.2001.114679. [DOI] [PubMed] [Google Scholar]
- 20.Iannotti JP, Bernot MP, Kuhlman JR, Kelley MJ, Williams GR. Postoperative assessment of shoulder function: a prospective study of full-thickness rotator cuff tears. J Shoulder Elbow Surg. 1996;5(6):449–457. doi: 10.1016/S1058-2746(96)80017-6. [DOI] [PubMed] [Google Scholar]
- 21.Jarvholm V, Styf J, Suurkula M, Herberts P. Intramuscular pressure and muscle blood flow in the supraspinatus. Eur J Appl Physiol. 1988;58:219–224. doi: 10.1007/BF00417252. [DOI] [PubMed] [Google Scholar]
- 22.Johannsen HV, Andersen NH, Sojbjerg JO, Sneppen O. Arthroscopic subacromial decompression. Ugeskr Laeger. 1997;159(2):166–170. [PubMed] [Google Scholar]
- 23.Klassen TP, Wiebe N, Russell K, Stevens K, Hartling L, Craig WR, et al. Abstracts of randomized controlled trials presented at the society for pediatric research meeting: an example of publication bias. Arch Pediatr Adolesc Med. 2002;156:474–479. doi: 10.1001/archpedi.156.5.474. [DOI] [PubMed] [Google Scholar]
- 24.Lees-Haley P. Attorneys influence expert evidence in forensic psychological and neuropsychological cases. Assessment. 1997;4:321–324. [Google Scholar]
- 25.McKee MD, Yoo DJ. The effect of surgery for rotator cuff disease on general health status. J Bone Jt Surg. 2000;82-A(7):970–979. doi: 10.2106/00004623-200007000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Michener LA, Leggin BG. A review of self-report scales for the assessment of functional limitation and disability of the shoulder. J Hand Ther. 2001;14(2):68–76. doi: 10.1016/s0894-1130(01)80036-3. [DOI] [PubMed] [Google Scholar]
- 27.Michener LA, McClure PW, Sennett BJ. American shoulder and elbow surgeons standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587–594. doi: 10.1067/mse.2002.127096. [DOI] [PubMed] [Google Scholar]
- 28.Misamore MW, Ziegler DW, Rushton JL. Repair of the rotator cuff. J Bone Jt Surg. 1995;77-A(9):1335–1339. doi: 10.2106/00004623-199509000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Neer CS., II Anterior acromioplasty for the chronic impingement syndrome in the shoulder. J Bone Jt Surg. 1972;54:41–50. [PubMed] [Google Scholar]
- 30.Nicholson GP. Arthroscopic acromioplasty: a comparison between workers’ compensation and non-workers’ compensation population. J Bone Jt Surg. 2003;85-A(4):682–689. [PubMed] [Google Scholar]
- 31.Noerdlinger MA, Cole BJ, Stewart M, Post M. Results of pectoralis major transfer with fascia lata autograft augmentation for scapula winging. J Shoulder Elbow Surg. 2002;11(4):345–350. doi: 10.1067/mse.2002.124525. [DOI] [PubMed] [Google Scholar]
- 32.Ogilvie-Harris DJ, Wiley AM, Sattarian J. Failed acromioplasty for impingement syndrome. J Bone Jt Surg Br. 1990;72-B(6):1070–1072. doi: 10.1302/0301-620X.72B6.2246291. [DOI] [PubMed] [Google Scholar]
- 33.Olsewski JM, Depew AD. Arthroscopic subacromial decompression and rotator cuff debridement for stage II and stage III impingement. Arthroscopy. 1994;10(1):61–68. doi: 10.1016/S0749-8063(05)80294-4. [DOI] [PubMed] [Google Scholar]
- 34.Paulos LE, Franklin JL. Arthroscopic shoulder decompression development and application. Am J Sports Med. 1990;18(3):235–244. doi: 10.1177/036354659001800303. [DOI] [PubMed] [Google Scholar]
- 35.Paulos LE, Kody MH. Arthroscopically enhanced “miniapproach” to rotator cuff repair. Am J Sports Med. 1994;22(1):19–25. doi: 10.1177/036354659402200104. [DOI] [PubMed] [Google Scholar]
- 36.Rainville J, Sobel JB, Hartigan C, Wright A. The effect of compensation involvement on the reporting of pain and disability by patients referred for rehabilitation of chronic low back pain. Spine. 1997;22(17):2016–2024. doi: 10.1097/00007632-199709010-00016. [DOI] [PubMed] [Google Scholar]
- 37.Roddey TS, Olson SL, Cook KF, Gartsman GM, Hanten W. Comparison of the University of California–Los Angeles shoulder scale and the simple shoulder test with the shoulder pain and disability index: single-administration reliability and validity. Phys Ther. 2000;80(8):759–768. [PubMed] [Google Scholar]
- 38.Sallay PI, Hunker PJ, Brown L. Measurement of baseline shoulder function in subjects receiving workers’ compensation versus noncompensated subjects. J Shoulder Elbow Surg. 2005;14(3):286–291. doi: 10.1016/j.jse.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 39.Shinners TJ, Noordsij PG, Orwin JF. Arthroscopically assisted mini-open rotator cuff repair. Arthroscopy. 2002;18(1):21–26. doi: 10.1053/jars.2002.26480. [DOI] [PubMed] [Google Scholar]
- 40.Silverstein B, Viikari-Juntura E, Kalat J. Use of a prevention index to identify industries at high risk for work-related musculoskeletal disorders of the neck, back, and upper extremity in Washington state, 1990–1998. Am J Ind Med. 2002;41:149–169. doi: 10.1002/ajim.10054. [DOI] [PubMed] [Google Scholar]
- 41.Smith KL, Harryman DT, II, Antoniou J, Campbell B, Sidles JA, Matsen FA., III A prospective, multipractice study of shoulder function ad health status in patients with documented rotator cuff tears. J Shoulder Elbow Surg. 2000;9(5):395–402. doi: 10.1067/mse.2000.108962. [DOI] [PubMed] [Google Scholar]
- 42.Spangehl MJ, Hawkins RH, McCormack RG, Loomer RL. Arthroscopic versus open acromioplasty: a prospective, randomized, blinded study. J Shoulder Elbow Surg. 2002;11(2):101–107. doi: 10.1067/mse.2002.120915. [DOI] [PubMed] [Google Scholar]
- 43.Svendsen SW, Gelineck J, Mathiassen SE, Bonde JP, Frich LH, Stengaard-Pedersen K, et al. Work above shoulder level and degenerative alterations of the rotator cuff tendons: a magnetic resonance imaging study. Arthritis Rheum. 2004;50(10):3314–3322. doi: 10.1002/art.20495. [DOI] [PubMed] [Google Scholar]
- 44.Viola RW, Boatright KC, Smith KL, Sidles JA, Matsen FA., III Do shoulder patients insured by workers’ compensation present with worse self-assessed function and health status? J Shoulder Elbow Surg. 2000;9(5):368–372. doi: 10.1067/mse.2000.107391. [DOI] [PubMed] [Google Scholar]
- 45.Waddell G, McCulloch J, Kummel E, Venner R. Nonorganic physical signs in low back pain. Spine. 1980;5(2):117–125. doi: 10.1097/00007632-198003000-00005. [DOI] [PubMed] [Google Scholar]