Abstract
Our objective was to assess and validate low-dose computed tomography (CT) scanogram as a post-operative imaging modality to measure the mechanical axis after navigated total knee replacement. A prospective study was performed to compare intra-operative and post-operative mechanical axis after navigated total knee replacements. All consecutive patients who underwent navigated total knee replacement between May and December 2006 were included. The intra-operative final axis was recorded, and post-operatively a CT scanogram of lower limbs was performed. The mechanical axis was measured and compared against the intra-operative measurement. There were 15 patients ranging in age from 57 to 80 (average 70) years. The average final intra-operative axis was 0.56° varus (4° varus to 1.5° valgus) and post-operative CT scanogram axis was 0.52° varus (3.1° varus to 1.8° valgus). The average deviation from final axes to CT scanogram axes was 0.12° valgus with a correlation coefficient of 0.9. Our study suggests that CT scanogram is an imaging modality with reasonable accuracy for measuring mechanical axis despite significantly low radiation. It also confirms a high level of correlation between intra-operative and post-operative mechanical axis after navigated total knee replacement.
Résumé
Cette étude a pour but d’analyser et d’évaluer les images scanner et les modalités des clichés post-opératoires après prothèse totale du genou implantée avec navigation.
Matériel et méthode: une étude prospective a été réalisée pour comparer les axes mesurés en per et post-opératoire, après navigation, chez les patients ayant bénéficié d’une prothèse totale du genou avec navigation et inclus de mai à décembre 2006. Les axes per et post-opératoires ont été rapportés et comparés avec l’axe mécanique obtenu et mesuré en per-opératoire.
Résultats: 15 patients d’âge moyen de 70 ans (57 – 80 ans) ont été analysés. L’axe final per-opératoire a été de 0.52° varus (4° à 1,5°) et, l’axe post-opératoire mesuré par scanner a été de 0.52° varus (3,1° à 1,8°). La déviation axiale médiane est de 0.12° valgus avec un coefficient de corrélation de 0,9.
En conclusion, notre étude permet de penser que le scanner est une modalité d’évaluation raisonnable de mesure de l’axe mécanique en dépit d’une irradiation significative mais néanmoins assez basse. Cette étude permet également de confirmer un haut niveau de corrélation entre la mesure de l’axe per-opératoire et la mesure de l’axe post-opératoire dans les prothèses totales du genou avec navigation.
Introduction
Conventional instrumentation for total knee replacement (TKR) may have limited accuracy in determining the crucial landmarks required to achieve correct mechanical axis alignment [5, 17]. With the advent of computer-guided surgery, various studies have suggested improved mechanical axis alignment for TKR using this technique [3, 5, 13]. We consider the computer-generated axis measurement to be a gold standard, given its high accuracy and reproducibility. Computed tomography (CT) scanogram is an extremely low-dose radiation imaging modality which does not require any special equipment except a basic CT scanner. To our knowledge there are no studies in the literature comparing intra-operative computer-generated axis and post-operative radiographic axis with the use of CT scanograms. Conventional long leg films involve significant radiation, which can be minimised by the use of CT scanograms. Besides, long leg films also require special long film plates which are not commonly available in most hospitals.
Materials and methods
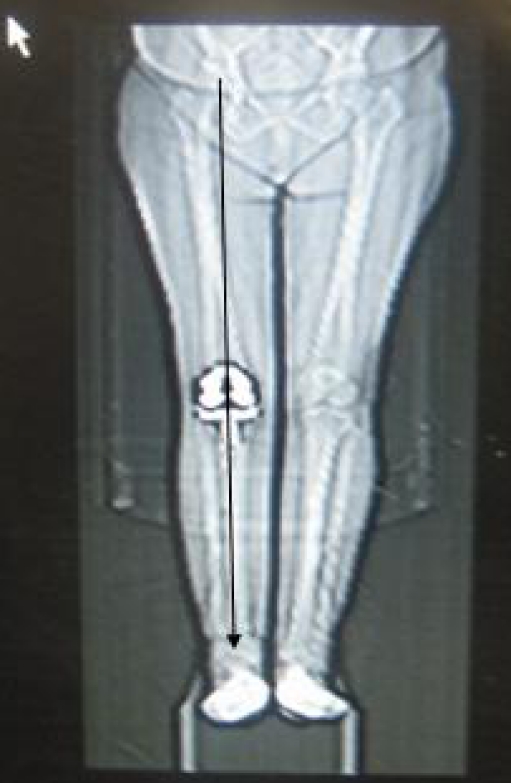
A prospective study was performed to compare the intra-operative and post-operative alignment of the lower limbs after navigated total knee replacements. All consecutive patients who underwent navigated total knee replacements between 1 May 2006 and 31 December 2006 were included in the study. An informed consent was obtained from all patients. Patients with inadequate data, patients who refused to participate in the study or were lost to follow-up and patients less than two weeks post-surgery were excluded. The intra-operative final axis in maximum extension was recorded from the navigation system. Post-operatively a CT scanogram of the lower limbs was performed with the knee in the same position (Fig. 1). Measurement of the mechanical hip-knee-ankle axis of the lower limb was performed on the scanogram. Results were subjected to matched pair analysis and a comparison made between the final and scanogram axis with assessment of their correlation coefficient.
Fig. 1.
Measurement of mechanical axis of the lower limb using CT scanogram after navigated total knee replacement
Results
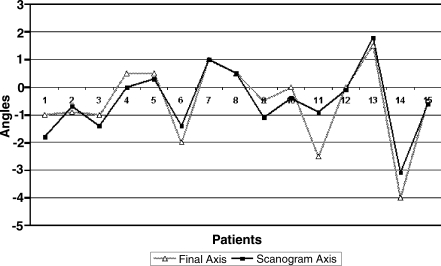
Complete data were available for 15 of the 25 patients initially recruited in the study. There were four men and 11 women ranging in age from 57 to 80 (average 70) years. The right knee was replaced in 12 and the left knee in three patients. The average intra-operative final axis recorded on the navigation system was 0.56° varus (4° varus to 1.5° valgus) and the average radiographic mechanical axis measured on CT scanogram in maximum possible extension was 0.52° varus (3.1° varus to 1.8° valgus) (Table 1). The average deviation from final to radiographic alignment was 0.12° valgus (Fig. 2). The correlation coefficient between final and scanogram axis was 0.9.
Table 1.
Demographics, intra-operative final axis and post-operative CT scanogram axis of 15 patients
| Patient No. | Age | Sex | Final axis | Scanogram axis |
|---|---|---|---|---|
| 1 | 76 | F | -1 | -1.8 |
| 2 | 57 | F | -0.9 | -0.7 |
| 3 | 60 | F | -1 | -1.4 |
| 4 | 62 | F | +0.5 | 0 |
| 5 | 66 | F | +0.5 | +0.3 |
| 6 | 68 | F | -2 | -1.4 |
| 7 | 68 | F | +1 | +1 |
| 8 | 70 | M | +0.5 | +0.5 |
| 9 | 70 | M | -0.5 | -1.1 |
| 10 | 70 | F | 0 | -0.4 |
| 11 | 73 | M | -2.5 | -0.9 |
| 12 | 75 | F | 0 | -0.1 |
| 13 | 77 | F | +1.5 | +1.8 |
| 14 | 79 | M | -4 | -3.1 |
| 15 | 80 | F | -0.5 | -0.6 |
| Average | -0.56 | -0.52 |
M male, F female, - indicates varus and + indicates valgus angles
Fig. 2.
Graph comparing the final and the scanogram axis of 15 patients after navigated total knee replacement
Discussion
The long-term results of total knee replacement are influenced by various factors. Several studies have emphasised the importance of the mechanical axis for good long-term results [1, 11, 13]. Implant malposition can cause pain, instability, implant loosening, polyethylene wear and decreased range of motion [2, 9, 11, 15]. Rand and Coventry reported 90% 10-year survivorship when the mechanical axis was within 0–4° varus or valgus and 73% ten-year survivorship when the mechanical axis was greater than 4° varus or valgus [16]. Various methods have been used to improve the accuracy of component placement. Kuzhupilly et al. have reported the use of Equiflex instrumentation to achieve optimum femoral rotation and improve patellar tracking [14].
With the use of computer navigation for TKR, many studies have reported an increase in the accuracy and reproducibility of component placement and limb alignment [3, 7, 18]. Given the precise algorithm which allows accurate measurement of mechanical axis, computer navigation is now considered to be the new gold standard for the purpose. Recently, Graydon et al. [6] evaluated the in vitro use of a navigation system based on electromagnetic technology, reporting accuracy similar to infrared-based navigation systems for total knee arthroplasty.
Most studies use full-leg radiographs or CT scan for assessment of overall mechanical alignment [4, 12]. However, these can be associated with significant radiation to the patient. The average dose of radiation with the conventional long leg radiograph is reported to be 0.7 mSv [8]. In our series, the average dose of radiation with the CT scanogram was estimated to be between 0.1 and 0.2 mSv. There is considerable variation in the literature regarding the dose of radiation depending on the CT technique and the protocol used. The Perth protocol [4] has reported a dose of 2.7 mSv and the Imperial knee protocol [10] a dose of 0.74 mSv in women and 0.54 mSv in men.
Our study shows no significant variation between intra-operative final computer-generated axis and CT scanogram axis, the average deviation being only 0.12° valgus. The correlation coefficient of 0.90 between final navigation axis and post-operative radiographic axis confirms that CT scanogram can be a reliable imaging modality in the measurement of mechanical axis alignment. It is easy to perform, involves low-dose radiation and yet provides reasonable accuracy.
Several limitations can be cited to be inherent to the technique, which involve variation due to rotational malalignment, inability to perform imaging whilst weight-bearing (although this is not possible intra-operatively either, hence does not affect the validity of the study) and perhaps a relatively small number of patients included in this study. We suggest that more studies be undertaken in different settings to further check the results before widespread use of the technique is advocated.
References
- 1.Bargren JH, Blaha JD, Freeman MA. Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Clin Orthop Relat Res. 1983;173:178–183. [PubMed] [Google Scholar]
- 2.Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A. Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Joint Surg Br. 2002;84:50–53. doi: 10.1302/0301-620X.84B1.12432. [DOI] [PubMed] [Google Scholar]
- 3.Chauhan SK, Clark GW, Lloyd S, Scott RG, Breidahl W, Sikorski JM. Computer-assisted total knee replacement. A controlled cadaver study using a multi-parameter quantitative CT assessment of alignment (the Perth CT Protocol) J Bone Joint Surg Br. 2004;86(6):818–823. doi: 10.1302/0301-620X.86B6.15456. [DOI] [PubMed] [Google Scholar]
- 4.Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg Br. 2004;86:372–377. doi: 10.1302/0301-620X.86B3.14643. [DOI] [PubMed] [Google Scholar]
- 5.Chiu KY, Yau WP, Ng TP, Tang WM. The accuracy of extramedullary guides for tibial component placement in total knee arthroplasty. Int Orthop. 2008;32:467–471. doi: 10.1007/s00264-007-0354-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graydon AJ, Malak S, Anderson IA, Pitto RP (2008) Evaluation of accuracy of an electromagnetic computer-assisted navigation system in total knee arthroplasty. Int Orthop. May 28. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 7.Haaker R, Stockheim M, Kamp M, Proff G, Breitenfelder J, Ottersbach A. Computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res. 2005;433:152–159. doi: 10.1097/01.blo.0000150564.31880.c4. [DOI] [PubMed] [Google Scholar]
- 8.Hart D, Millier MC, Wall BF, Shrimpton PC, Bungay D (1995) Doses to patients from medical X-ray examinations in the UK 1995 review, NRPB-R289. Her Majesty’s Stationary Office, London, pp 199–201
- 9.Hofmann S, Romero J, Roth-Schiffl E, Albrecht T. Rotational malalignment of the components may cause chronic pain or early failure in total knee arthroplasty (in German) Orthopade. 2003;32:469–476. doi: 10.1007/s00132-003-0503-5. [DOI] [PubMed] [Google Scholar]
- 10.Henckel J, Richards R, Lozhkin K, Harris S, Baena FM, Barrett AR, Cobb JP. Very low-dose computed tomography for planning and outcome measurement in knee replacemen.: The imperial knee protocol. J Bone Joint Surg Br. 2006;88:1513–1518. doi: 10.1302/0301-620X.88B11.17986. [DOI] [PubMed] [Google Scholar]
- 11.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 12.Jessup DE, Worland RL, Clelland C, Arredondo J. Restoration of limb alignment in total knee arthroplasty: evaluation and methods. J South Orthop Assoc. 1997;6(1):37–47. [PubMed] [Google Scholar]
- 13.Jonsson B, Astrom J. Alignment and long-term clinical results of a semiconstrained knee prosthesis. Clin Orthop Relat Res. 1988;226:124–128. [PubMed] [Google Scholar]
- 14.Kuzhupilly RR, Seferiadis I, Lennox IA. Optimising femoral component rotation using Equiflex instrumentation: a clinical review. Int Orthop. 2008;32(3):345–353. doi: 10.1007/s00264-007-0340-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59:77–79. [PubMed] [Google Scholar]
- 16.Rand JA, Coventry MB. Ten-year evaluation of geometric total knee arthroplasty. Clin Orthop Relat Res. 1988;232:168–173. [PubMed] [Google Scholar]
- 17.Stulberg SD, Loan P, Sarin V. Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am. 2002;84:90–98. [PubMed] [Google Scholar]
- 18.Victor J, Hoste D. Image-based computer-assisted total knee arthroplasty leads to lower variability in coronal alignment. Clin Orthop Relat Res. 2004;428:131–139. doi: 10.1097/01.blo.0000147710.69612.76. [DOI] [PubMed] [Google Scholar]