Abstract
Surface arthroplasty of the hip is increasingly popular. Optimising the position of the femoral component is essential to avoid early implant failures such as femoral neck fractures. Sixty hip surface replacements were retrospectively analysed. In 30 patients imageless navigation was used, and 30 patients were operated upon using conventional jigs. Accuracy, implant position, operating time, and complications have been recorded. The navigation device improved the implant position with high accuracy. Implant-shaft angles <130° and uncovered cancellous bone of the superior femoral neck could be safely avoided. After a significant learning curve, navigation took 15 minutes longer than conventional implantation. No complications were found in either group. Computer-assisted navigation allowed accurate implantation of the femoral component avoiding pitfalls of hip surface replacement. From our point of view the optimal placement of the femoral component outweighs the disadvantage of a longer operating time.
Résumé
Le resurfaçage de la hanche devient de plus en plus populaire. L’optimisation de la position du composant fémoral est importante afin d’éviter les échecs tels que les fractures du col. Matériel et méthode : 60 resurfaçages de hanche ont été analysés de façon rétrospective chez 30 patients en utilisant la même technique avec navigation, sans image et en comparant cette série à une série de 30 patients opérés de façon conventionnelle. La sécurité, la position de l’implant, le temps opératoire et les complications ont été rapportés. Résultats : le système de navigation améliore la position de l’implant de façon significative. Après la courbe d’apprentissage le temps de la navigation augmente de 15 minutes le temps opératoire. Aucune complication n’a été relevée dans les deux groupes. Conclusions : La technique chirurgicale assistée par la navigation permet une meilleure implantation du composant fémoral et évite les erreurs en cas de resurfaçage de hanche. Pour nous, l’amélioration de la position du composant fémoral contrebalance de façon avantageuse l’augmentation du temps opératoire.
Introduction
Over the last decade there has been a renewed enthusiasm for the concept of hip resurfacing as an alternative to conventional hip arthroplasty, especially for the young and active patient. The main advantage of hip resurfacing arthroplasty is the preservation of femoral bone stock thus improving the outcome of future hip replacements [1, 9].
Other benefits are better joint stability and proprioception because it more closely mimics normal hip kinematics and there is reduced risk of leg length discrepancy [4, 18, 23]. Furthermore, it has been suggested that this technique may permit the patient to return to a greater level of activity and sport than other reconstructive options [4].
While hip resurfacing has shown excellent short and middle term results, the technical procedure is more difficult. It has been shown that implantation of the femoral component is the crucial step during the operative procedure. The orientation of the femoral component strongly affects the risk of femoral neck fractures and osteonecrosis [5, 6, 15, 19, 20]. Therefore, tight alignment of the femoral component on the femoral neck and a sufficient valgus position must be achieved during the operation [5, 20].
The role of computer navigation in total joint arthroplasty is increasing and may improve long term results by enhancing the accuracy of implantation [17, 22]. Otherwise, there is no doubt that navigation prolongs the procedure. This, in turn, might lead to an increased rate of complications such as infection or bleeding.
Attempts have been made to use computer-assisted surgery to improve the implant position of the femoral component during hip resurfacing [7, 10–13]. Others have shown that the learning curve of inexperienced surgeons in hip resurfacing is reduced by the use of navigation [8]. But, to our knowledge, no comparative in vivo study has been undertaken to investigate the role of image-free computer navigation during the hip resurfacing procedure.
The purpose of our study was to discover if computer-assisted surgery (CAS) during hip resurfacing leads to an improved implant position of the femoral component. The accuracy of the navigation system, the amount of additional operating time, the existence of a learning curve, and the occurrence of complications are further points of interest in our study.
Materials and methods
Data of 60 patients with primary coxarthritis following a hip resurfacing procedure were retrospectively analysed. Patients were operated upon by DPK and PE using the ASR implant (DePuy, Leeds, England) and a standard posterior approach to the hip. In 30 patients (CAS group), hip resurfacing has been performed using the computer-assisted navigation system Ci Software for the DePuy ASR System (DePuy, Leeds, England). The other 30 patients (conventional group) were operated with the conventional jig technique as delivered from the manufacturer.
The surgeons in this study were experienced in hip resurfacing using the mechanically-based alignment technique using jigs; during the study, they began using the CAS system on the hip. Therefore one of the purposes of this study was to evaluate a potential learning curve for hip resurfacing and CAS.
The following data from the 60 patients were recorded: age, gender, preoperative projected neck–shaft angle (preoperative CCD angle), duration of the operation, postoperative shaft–implant angle (postoperative CCD angle), notching of the femoral neck, uncovered reamed cancellous bone, postoperative complications in the first two weeks (CCD angle = caput–collum–diaphysis angle).
Our aim concerning the postoperative CCD angle was to implant the smallest possible femoral component at an implant–shaft angle of at least 130° without notching the femoral neck or leaving uncovered reamed cancellous bone. The projected CCD angles were measured using a standard AP radiograph, taken the day before and two weeks after the operation. Using the same postoperative radiographs, femoral notching and uncovered cancellous bone were recorded.
Operative procedure
A standard posterior approach to the hip was used for both the navigated and conventional groups.
Standard procedure An alignment pin was placed in the lateral cortex of the femur as measured in the preoperative planning. A 2.4-mm guide wire was placed into the femoral head and neck using the mechanical jig as described by McMinn [18]. Subsequently, the femoral head was prepared stepwise.
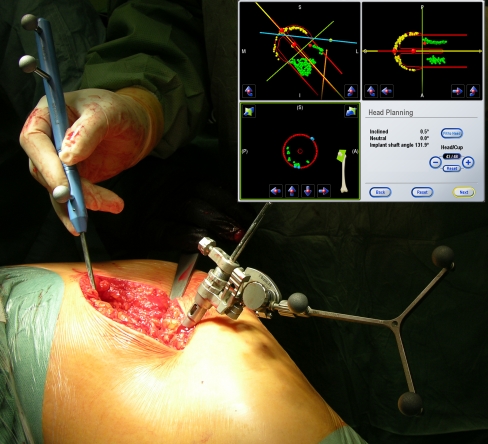
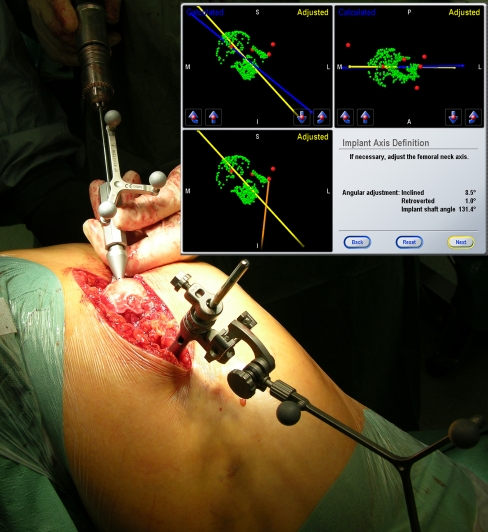
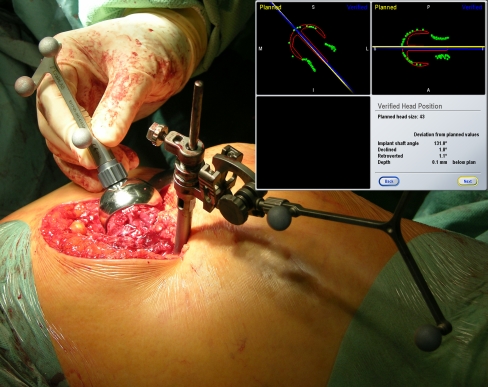
CAS procedure In order to establish a coordinate on the femur for real-time tracking during the procedure, a 5 mm pin was placed in the lesser trochanter and the optical unit was attached. The centre of rotation of the femoral head was calculated by pivoting the femur. The following landmarks were registered using the navigation pointer: medial and lateral epicondyles, tip of the greater trochanter, piriformis fossa, and intended cap edge. Clusters of points of the femoral head, as well as the superior, inferior, ventral, and dorsal femoral neck were taken (Fig. 1). The automatically generated model of the CAS system was checked for accuracy and the target position of the femoral implant was modified by the surgeon to place it in an optimal position. The 2.4-mm guide wire was inserted into the femoral head and neck using the navigated drill guide (Fig. 2). Navigated depth drilling was performed; thereafter, the femoral head was prepared using the standard instrumentation. The acetabular cup was prepared using conventional mills and the final cup was implanted. The final femoral component was implanted and, after curing of the cement, the position of the implanted femoral component was verified with the stem position verification tool and compared to the planned target position (Fig. 3). All data were recorded by the computer and saved for analysis.
Fig. 1.
Collection of points on the femoral neck and head with the navigation pointer. The optical unit is attached in the lesser trochanter. In the upper right corner of the figure, the navigation screen with the registered landmarks (yellow and green points) shows all three dimensions. The size of the implant with a natural neck–shaft angle is proposed by the computer and can be corrected by the surgeon
Fig. 2.
The navigated drill guide is inserted into the femoral neck and shaft. On the navigator screen the planned axis is shown (yellow). In addition to the natural neck–shaft angle, an inclination of 8.5° and retroversion of 1° was chosen to reach a CCD angle above 130° and to avoid notching
Fig. 3.
The implanted position of the femoral component is verified with the navigation tool. Differences between planning and implanted position are shown on the navigator screen
Postoperative management
Wound drains were removed on the first or second day after operation depending on the amount of bleeding. Patients were instructed in partial weight bearing (20 kg for six weeks). The patients were discharged from hospital between the 12th and 14th days after the operative procedure in accordance with our national financing system.
Statistics
Differences between the variables of the two techniques were computed using students t test. All differences were evaluated for significance based on a p value <0.05.
Results
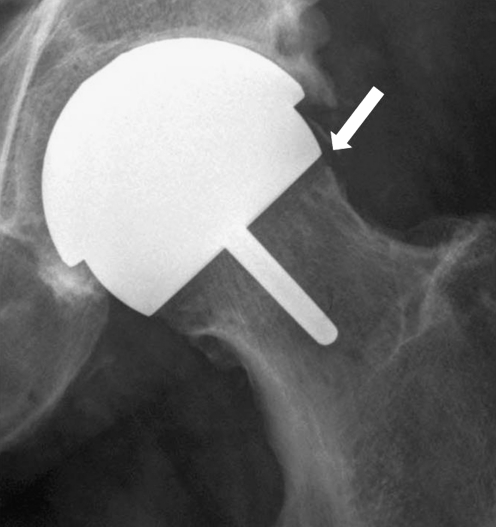
Of the data desired from the 60 operated patients, 93% were available and are shown in Table 1. Analysis of the pre- and postoperative radiographs resulted in an average increase of 4° valgus in both groups with a standard deviation of 4.9° vs. 4.1° irrespective of the different preoperative CCD angles (p = 0.73). The goals of reaching an implant-–shaft angle >130°, avoiding superior neck notching, and leaving no uncovered cancellous bone have been reached for all patients of the CAS group; whereas in the conventional group, three patients had a lower CCD angle and in three patients uncovered cancellous bone was detected (Fig. 4). Comparing the preoperative CCD angles, a slight varus position reaching from −1° to −2° of the implant occurred in four patients in each group (average in the CAS group: 137°, range 132–141°; average in the conventional group: 137°, range 129–145°). One operation (DH) had to be switched to a standard shaft implant due to the large diameter of the femoral neck and undersized acetabular seat. No further complications were recorded.
Table 1.
Patient data
| Initials | Group | Age | Gender | Date of the operation | Operating time (min) | Neck–shaft angle (°) | Implant–shaft angle (°) | CCD° difference |
|---|---|---|---|---|---|---|---|---|
| HH | CAS | 72 | M | 08.09.2005 | 145 | 135 | 135 | 0 |
| GF | CAS | 40 | M | 01.09.2005 | 210 | 142 | 141 | −1 |
| DH | CAS | 52 | M | 26.08.2005 | Switched to standard shaft implant | |||
| KU | CAS | 52 | F | 31.08.2005 | 200 | 143 | 148 | 5 |
| MI | CAS | 59 | F | 02.09.2005 | 175 | 136 | 137 | 1 |
| HS | CAS | 48 | F | 13.10.2005 | 140 | 130 | 135 | 5 |
| ST | CAS | 39 | M | 28.09.2005 | 155 | 140 | 140 | 0 |
| BP | CAS | 41 | M | 30.09.2005 | 195 | 133 | 132 | −1 |
| KJ | CAS | 52 | M | 28.11.2005 | 150 | 128 | 135 | 7 |
| HM | CAS | 34 | F | 25.01.2006 | 150 | |||
| RU | CAS | 55 | M | 03.02.2006 | 120 | 132 | 140 | 8 |
| MG | CAS | 55 | M | 11.05.2006 | 130 | 140 | ||
| RB | CAS | 51 | F | 31.07.2006 | 120 | 138 | 138 | 0 |
| GV | CAS | 74 | M | 24.08.2006 | 125 | 136 | 138 | 2 |
| GW | CAS | 52 | F | 06.12.2006 | 125 | 135 | 138 | 3 |
| WT | CAS | 66 | M | 18.01.2007 | 130 | 132 | 132 | 0 |
| KG | CAS | 59 | M | 22.01.2007 | 115 | 137 | 141 | 4 |
| EK | CAS | 55 | M | 12.02.2007 | 127 | 118 | 136 | 18 |
| RC | CAS | 65 | M | 12.02.2007 | 120 | 138 | ||
| UJ | CAS | 46 | M | 01.03.2007 | 125 | 142 | 140 | −2 |
| UG | CAS | 59 | F | 06.03.2007 | 120 | 132 | 134 | 2 |
| EJ | CAS | 58 | F | 22.03.2007 | 120 | 134 | 148 | 14 |
| FG | CAS | 62 | M | 27.03.2007 | 125 | 134 | 142 | 8 |
| RA | CAS | 58 | M | 02.04.2007 | 120 | 140 | 138 | −2 |
| HT | CAS | 51 | M | 19.04.2007 | 96 | 133 | 136 | 3 |
| BJ | CAS | 50 | F | 23.04.2007 | 100 | 141 | 145 | 4 |
| SW | CAS | 39 | M | 04.06.2007 | 90 | 138 | 140 | 2 |
| AR | CAS | 50 | F | 15.08.2007 | 115 | 130 | 132 | 2 |
| JK | CAS | 60 | M | 29.08.2007 | 100 | 140 | 144 | 4 |
| LC | CAS | 58 | F | 13.09.2007 | 86 | 136 | 148 | 12 |
| MV | Conventional | 53 | F | 10.01.2006 | 90 | 130 | 131 | 1 |
| LH | Conventional | 58 | F | 06.01.2006 | 110 | 126 | 131 | 5 |
| PK | Conventional | 47 | M | 22.09.2005 | 130 | 146 | 145 | −1 |
| PH | Conventional | 67 | M | 15.07.2005 | 85 | 131 | 129 | −2 |
| SP | Conventional | 45 | F | 01.08.2005 | 95 | 131 | 133 | 2 |
| NV | Conventional | 59 | M | 18.10.2005 | 110 | 130 | 131 | 1 |
| HB | Conventional | 49 | M | 03.11.2005 | 130 | 130 | 132 | 2 |
| SK | Conventional | 51 | M | 18.11.2005 | 90 | 143 | 140 | −3 |
| KP | Conventional | 55 | F | 23.11.2005 | 90 | 128 | 129 | 1 |
| VD | Conventional | 51 | M | 17.04.2007 | 90 | 132 | 140 | 8 |
| FS | Conventional | 48 | M | 08.03.2007 | 130 | 125 | 135 | 10 |
| JH | Conventional | 62 | M | 06.03.2007 | 70 | 120 | 130 | 10 |
| AL | Conventional | 56 | M | 22.02.2007 | 80 | 138 | 150 | 12 |
| KS | Conventional | 46 | F | 12.02.2007 | 105 | 130 | 138 | 8 |
| MN | Conventional | 62 | M | 05.02.2007 | 100 | 120 | 132 | 12 |
| BS | Conventional | 57 | M | 30.01.2007 | 60 | 124 | 128 | 4 |
| WZ | Conventional | 50 | M | 29.01.2007 | 110 | 122 | 131 | 9 |
| DB | Conventional | 59 | M | 25.01.2007 | 90 | 126 | 134 | 8 |
| ES | Conventional | 59 | M | 16.01.2007 | 145 | 128 | 136 | 8 |
| HK | Conventional | 46 | F | 03.01.2007 | 100 | 130 | 136 | 6 |
| WB | Conventional | 47 | F | 06.06.2007 | 95 | 131 | 133 | 2 |
| HK | Conventional | 54 | M | 12.06.2007 | 80 | 127 | 131 | 4 |
| UR | Conventional | 55 | M | 03.02.2006 | 115 | 130 | 136 | 6 |
| VM | Conventional | 53 | M | 10.01.2006 | 95 | 133 | 138 | 5 |
| JW | Conventional | 41 | F | 14.11.2005 | 85 | 129 | 131 | 2 |
| FK | Conventional | 56 | M | 15.06.2005 | 95 | 128 | 135 | 7 |
| FW | Conventional | 59 | M | 16.11.2006 | 90 | 134 | 138 | 4 |
| SR | Conventional | 44 | M | 25.06.2007 | 100 | 137 | 135 | −2 |
| SS | Conventional | 37 | F | 25.06.2007 | 115 | 124 | 130 | 6 |
| CH | Conventional | 39 | F | 29.06.2007 | 95 | 130 | 134 | 4 |
CAS computer-assisted surgery with image-free navigation, conventional conventional jig technique, CCD caput–collum–diaphysis angle
Fig. 4.
Uncovered reamed cancellous bone on the superior region of the femoral neck (arrow)
Analysis of the accuracy between computer-aided planning and implant position of the femoral component was available after a software update in April 2006 and is shown in Table 2. The average error of the CCD angles was 0.67° (range −1 to 2.3°), error of anteversion 1.09° (range −3.7 to 0.8°), and the average error of depth was 1.56 mm (range −2.9 to 4.8 mm).
Table 2.
Accuracy of computer-assisted navigation
| Initials | CCD° error | Anteversion error | Depth error |
|---|---|---|---|
| MG | 2.3 | −3.7 | −0.7 |
| RB | 1.10 | −3.00 | 0.60 |
| GV | 0.80 | 1.20 | 1.20 |
| GW | 0.00 | 0.00 | 0.00 |
| WT | −1.10 | −0.60 | −1.60 |
| KG | −0.50 | 0.80 | 0.80 |
| EK | 0.20 | −0.40 | −1.20 |
| RC | 0.50 | 1.40 | 1.70 |
| UJ | 0.60 | 0.50 | 1.74 |
| UG | 0.80 | 1.30 | 1.60 |
| EJ | −0.40 | −1.00 | 0.40 |
| FG | −0.30 | −1.60 | −2.40 |
| RA | −1.30 | −0.80 | −2.90 |
| HT | −0.60 | 0.00 | −1.40 |
| BJ | 0.00 | 0.80 | 4.80 |
| SW | 1.00 | −1.10 | −2.80 |
| AR | −1.00 | −1.10 | −0.10 |
| JK | −0.10 | −1.00 | −3.40 |
| LC | 0.20 | 0.50 | −0.30 |
| Average | 0.67 | 1.09 | 1.56 |
Differences between planning and final implanted position of the femoral component are shown for caput–collum–diaphysis (CCD) angle, anteversion, and depth
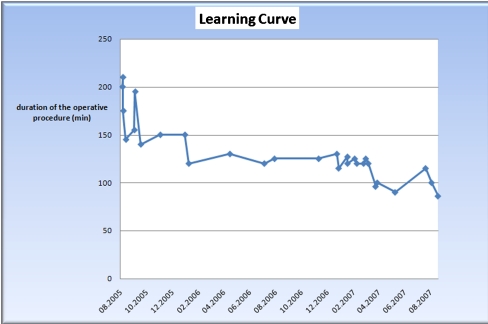
Operating times for the CAS procedure are shown in Fig. 5. Comparing the first and the last 15 patients the operative time dropped significantly from 153 minutes to 113 minutes (p < 0.005). No difference in duration of the operative procedure in the conventional group was detected (1st 15 patients 100 minutes vs. 2nd 15 patients 98 minutes; p = 0.35).
Fig. 5.
Learning curve in the navigated group. Duration of the operative procedure dropped from 153 minutes for the first 15 patients to 113 minutes for the last 15 patients (p < 0.005)
Discussion
Follow-up studies have shown that the main reason for early implant failure is malorientation of the femoral component [2, 5, 21]. In this context a relatively high rate of early implant failures has been reported. For example, Amstutz reported about 3% early failures, significantly associated with a varus position of the implant [2], and Shimmin detected a rate of 1.46% femoral neck fractures after resurfacing of the hip [21]. Of those patients 46% had notching of the superior femoral neck and in 71% the femoral component had been implanted in a varus position.
To minimise the risk of malposition, we applied computer-assisted navigation of the femoral component. As far as we know our study is the first to report the clinical application of the image-free navigation for surface replacement of the hip.
In our series the navigation resulted in an extremely accurate placement of the femoral component. Discrepancies between planning and implantation below 1° for CCD angle, circa 1° for anteversion, and about 1.5 mm for depth were found to be superior to other studies. Other reports include CCD angle errors of 2.6° and 3.3° in cadaver studies with computer tomography-based navigation systems [7, 10], 2.2° in image-free cadaver studies [12], and 2.8° in a clinical fluoroscopic study [11]. The accuracy of our navigation system is comparable to the results of image-free computer navigation of total knee arthroplasty, resulting in an error of approximately 1° [14].
A planning problem of our study was the definition of the target CCD angle of the femoral component. It is common sense that a varus placement increases the total stresses (compression and bending) in the superior femoral neck [5, 16] and that a varus orientation correlates with early neck fractures and femoral implant loosening [2, 5, 20, 21]. Likewise, uncovered reamed cancellous bone or notching, especially of the superior femoral neck, is undesirable leading to early implant failure. But the available data about the optimal CCD angle is inconsistent. In one study, a target position of the femoral component with as much valgus as possible is published [11], but others have defined a fixed CCD angle of 140° [2]. Other groups have defined the target CCD angle as a valgus position compared to the preoperative CCD angle [3, 20]. In a follow-up study of nearly 3,500 surface replacements and analysis of femoral neck fractures, no implant failure occurred while the femoral component had been placed in valgus compared with the preoperative neck–shaft angle [21]. Beaulé reported that CCD angles of the femoral component below 130° had an increased risk of an adverse outcome [5].
Therefore, our philosophy was to place the smallest possible femoral component in a valgus position of at least 130°. An excessive valgus placement was not desired because in this case a larger femoral component had to be implanted to avoid femoral notching, leading to additional loss of acetabular bone stock. These targets were reached for all patients of the CAS group, while femoral implant position was significantly more imprecise in the conventional group where three patients had an implant angle below 130° and in three patients uncovered cancellous bone remained in the superior neck region. In both groups a slight varus placement occurred in four patients. In the CAS group the slight varus drift between −1° and −2° was exclusively caused by the surgeon (the navigation system recommends a position of the femoral component with a physiological CCD angle and the surgeon may correct the position on the touchscreen to a slight valgus position). If the surgeon accepts the natural CCD angle, a varus placement of one or two degrees may occur due to the limits of the navigation device. It is important to know about this potential source of error as this can be avoided by correcting the target implant position to a valgus angle.
As mentioned above, the inconsistent target CCD angle complicated the analysis of the benefit of computer navigation in our series. Hence, no significant difference in angles of the femoral component between both groups could be detected. These findings correspond to other published studies [13]. In any case, the unfavourable situations of a placement below 130° and leaving uncovered reamed cancellous bone could be reliably avoided by use of the computer navigation.
Our learning curve for computer-assisted navigation was mainly influenced by technical aspects of using pointers, drill guides, and software. After a training period the navigation took about 15 minutes longer compared to conventional implanted surface replacements. Similar results have been published by Hess et al. [11] while others reported no additional lead time [13]. It has been shown that computer navigation accelerates the learning curve of inexperienced surgeons in implanting surface replacements of the hip [8]. In our opinion, image-free computer navigated implantation of hip surface replacement definitely needs additional time compared to conventional implantation due to the necessity of positioning the optical unit and registration of the required points. In our study, no adverse effects of the extended operating time in the form of infections, wound healing disorders, or bleeding have been detected; but, the prolonged operation is a disadvantage of computer navigation and causes a price increase of the operation and may potentially favour complications.
Our study has obvious limitations. Due to the retrospective design the evaluated groups differ, e.g. in the preoperative CCD angles, and therefore complicated interpretation of our data. Furthermore, we analysed only a relatively small number of patients and long term follow-up data for navigated implantation of surface replacements is missing.
In our opinion additional computer navigation of the acetabular component is desirable to minimise risks of femoral neck impingement or malposition. Therefore, navigation of the femoral and acetabular components is part of our ongoing study.
In conclusion, computer-assisted navigation allowed an extremely accurate implantation of the femoral component, avoiding the pitfalls of hip surface replacement such as femoral notching or leaving reamed cancellous bone uncovered. Hence, navigation may improve the possibility for long term survival of the implant. From our point of view the optimal placement of the femoral component outweighs the disadvantage of a longer operating time. Ongoing prospective follow-up studies are necessary to evaluate the benefit of computer-assisted navigation of hip surface replacement.
References
- 1.Amstutz HC, Ball ST, Le Duff MJ, Dorey FJ (2007) Resurfacing THA for patients younger than 50 years: results of 2- to 9-year followup. Clin Orthop Relat Res 460:159–164 [DOI] [PubMed]
- 2.Amstutz HC, Beaule PE, Dorey FJ, Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Jt Surg Am. 2004;86-A:28–39. [PubMed] [Google Scholar]
- 3.Anglin C, Masri BA, Tonetti J, Hodgson AJ, Greidanus NV (2007) Hip resurfacing femoral neck fracture influenced by valgus placement. Clin Orthop Relat Res 465:71–79 [DOI] [PubMed]
- 4.Beaule PE, Amstutz HC, Le DM, Dorey F. Surface arthroplasty for osteonecrosis of the hip: hemiresurfacing versus metal-on-metal hybrid resurfacing. J Arthroplasty. 2004;19:54–58. doi: 10.1016/j.arth.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 5.Beaule PE, Lee JL, Le Duff MJ, Amstutz HC, Ebramzadeh E. Orientation of the femoral component in surface arthroplasty of the hip. A biomechanical and clinical analysis. J Bone Jt Surg Am. 2004;86-A:2015–2021. doi: 10.2106/00004623-200409000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Beaule PE, Poitras P. Femoral component sizing and positioning in hip resurfacing arthroplasty. Instr Course Lect. 2007;56:163–169. [PubMed] [Google Scholar]
- 7.Belei P, Skwara A, La FM, Schkommodau E, Fuchs S, Wirtz DC, Kamper C, Radermacher K. Fluoroscopic navigation system for hip surface replacement. Comput Aided Surg. 2007;12:160–167. doi: 10.1080/10929080701336207. [DOI] [PubMed] [Google Scholar]
- 8.Cobb JP, Kannan V, Brust K, Thevendran G (2007) Navigation reduces the learning curve in resurfacing total hip arthroplasty. Clin Orthop Relat Res 463:90–97 [DOI] [PubMed]
- 9.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Jt Surg Br. 2004;86:177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 10.Davis ET, Gallie P, Macgroarty K, Waddell JP, Schemitsch E. The accuracy of image-free computer navigation in the placement of the femoral component of the Birmingham hip resurfacing: a cadaver study. J Bone Jt Surg Br. 2007;89-B:557–560. doi: 10.1302/0301-620X.89B4.17893. [DOI] [PubMed] [Google Scholar]
- 11.Hess T, Gampe T, Kottgen C, Szawlowski B. Intraoperative navigation for hip resurfacing. Methods and first results. Orthopade. 2004;33:1183–1193. doi: 10.1007/s00132-004-0693-5. [DOI] [PubMed] [Google Scholar]
- 12.Hodgson AJ, Inkpen KB, Shekhman M, Anglin C, Tonetti J, Masri BA, Duncan CP, Garbuz DS, Greidanus NV. Computer-assisted femoral head resurfacing. Comput Aided Surg. 2005;10:337–343. doi: 10.1080/10929080500379440. [DOI] [PubMed] [Google Scholar]
- 13.Kruger S, Zambelli PY, Leyvraz PF, Jolles BM (2007) Computer-assisted placement technique in hip resurfacing arthroplasty: improvement in accuracy? Int Orthop 24 Aug 2007. Epub ahead of print [DOI] [PMC free article] [PubMed]
- 14.Laskin RS, Beksac B. Computer-assisted navigation in TKA: where we are and where we are going. Clin Orthop Relat Res. 2006;452:127–131. doi: 10.1097/01.blo.0000238823.78895.dc. [DOI] [PubMed] [Google Scholar]
- 15.Little JP, Taddei F, Viceconti M, Murray DW, Gill HS. Changes in femur stress after hip resurfacing arthroplasty: response to physiological loads. Clin Biomech. 2007;22:440–448. doi: 10.1016/j.clinbiomech.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 16.Long JP, Bartel DL. Surgical variables affect the mechanics of a hip resurfacing system. Clin Orthop Relat Res. 2006;453:115–122. doi: 10.1097/01.blo.0000238873.09390.6f. [DOI] [PubMed] [Google Scholar]
- 17.Martin A, Wohlgenannt O, Prenn M, Oelsch C, Strempel A. Imageless navigation for TKA increases implantation accuracy. Clin Orthop Relat Res. 2007;460:178–184. doi: 10.1097/BLO.0b013e31804ea45f. [DOI] [PubMed] [Google Scholar]
- 18.McMinn D, Treacy R, Lin K, Pynsent P. Metal on metal surface replacement of the hip. Experience of the McMinn prosthesis. Clin Orthop Relat Res. 1996;329:S89–S98. doi: 10.1097/00003086-199608001-00009. [DOI] [PubMed] [Google Scholar]
- 19.Morlock MM, Bishop N, Ruther W, Delling G, Hahn M. Biomechanical, morphological, and histological analysis of early failures in hip resurfacing arthroplasty. Proc Inst Mech Eng. 2006;220:333–344. doi: 10.1243/095441105X69015. [DOI] [PubMed] [Google Scholar]
- 20.Radcliffe IA, Taylor M. Investigation into the effect of varus-valgus orientation on load transfer in the resurfaced femoral head: a multi-femur finite element analysis. Clin Biomech. 2007;22:780–786. doi: 10.1016/j.clinbiomech.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Shimmin AJ, Back D. Femoral neck fractures following Birmingham hip resurfacing: a national review of 50 cases. J Bone Jt Surg Br. 2005;87:463–464. doi: 10.1302/0301-620X.87B4.15498. [DOI] [PubMed] [Google Scholar]
- 22.Siston RA, Giori NJ, Goodman SB, Delp SL. Surgical navigation for total knee arthroplasty: a perspective. J Biomech. 2007;40:728–735. doi: 10.1016/j.jbiomech.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 23.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Jt Surg Br. 2005;87:167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]