Abstract
The purpose of this prospective study was to describe cementless humeral surface replacement arthroplasty (CHSRA) as a bone preserving treatment option for patients with fixed anterior glenohumeral dislocation. Ten patients with post-traumatic fixed anterior glenohumeral dislocation underwent CHSRA with a mean follow-up of 24 months. All patients were evaluated clinically using the Constant score and with radiographs in two planes. There were two reoperations: one patient developed glenoid erosion and was revised and in another case redislocation occurred. Clinical or radiographical signs of implant loosening were not found. The humeral head centred in the glenoid in nine out of ten cases radiographically. The Constant score increased from 20 points preoperatively to 61 points postoperatively (p < 0.007). CHSRA is a viable treatment option for elderly patients with fixed anterior glenohumeral dislocation and bone defects of the humeral head. Good clinical results and a moderate complication rate were found in the short term.
Résumé
Le sujet de cette étude prospective était de montrer que le resurfaçage sans ciment au niveau de l’épaule est un option permettant la préservation du capital osseux pour des patients avec une luxation antérieure chronique de l’épaule. Dix patients avec une luxation gléno humérale antérieure fixée ont subi un resurfaçage sans ciment avec un suivi moyen de 24 mois. Tous les patients ont été évalués cliniquement à l’aide du score de Constant et des radiographies dans deux plans. Deux réinterventions ont été nécessaires. Un patient a développé une érosion glénoïdienne nécessitant un changement de prothèse et un patient a récidivé sa luxation. Il n’y avait pas de signe clinique ou radiographique de descellement des implants. La tête humérale était centrée dans la glène dans 9 cas sur 10. Le score de constant s’est accru de 20 points en préopératoire à 61 points en post opératoire (p<0.007). Le resurfaçage huméral sans ciment est donc une solution fiable pour les patients âgés avec une luxation antérieure chronique et une encoche au niveau de la tête humérale. De bons résultats clinique et un taux de complications modéré ont été retrouvés à court terme.
Introduction
Traumatic anterior glenohumeral dislocation is a serious condition which can lead to soft tissue damage and substantial defects of the humeral head and glenoid. Disturbance of shoulder joint congruency and soft tissue balancing can lead to poor function and severe impairment in these patients. Several surgical treatment options have been described to avoid redislocation of the humeral head. These include reorientation of the humeral head [9, 23], filling the defect with humeral allograft [18] to restore joint congruency, and bone transfer techniques [4, 7, 11, 24]. Shoulder replacement for fixed shoulder dislocation has been discussed extensively as new implants were developed in shoulder arthroplasty in recent years [1, 14, 17, 19, 21]. Resurfacing arthroplasty is an established bone preserving alternative treatment option for shoulder hemiarthroplasty [12, 13] and could be an option for patients with fixed shoulder dislocation in combination with large humeral head defects. For stabilisation of a dislocated shoulder joint with large bone defects it is crucial to restore joint congruency in combination with reconstruction of concomitant soft tissue pathologies, i.e. subscapularis elongation or rupture.
Therefore, the aim of this study was to present cementless humeral surface replacement arthroplasty (CHSRA) as a viable treatment option in cases with fixed anterior shoulder dislocation in combination with large humeral head defects.
Materials and methods
Between January 2003 and August 2006, ten patients (ten shoulders) with fixed anterior glenohumeral dislocation and large humeral head defects were treated with CHSRA at our institution. There were six females and four males. The dominant shoulder was involved in six cases. Mean age at the time of arthroplasty was 67 years (range 51–75 years). In all cases a traumatic anterior shoulder dislocation of longer than six weeks in duration was treated. One patient had diagnostic arthroscopic surgery before shoulder arthroplasty. Additional rotator cuff lesions were found in six cases, including three supraspinatus and three subscapularis tears. If possible, rotator cuff repair was performed during the same operation. In one case a Bankart fracture was treated by an extraatricular screw in the same session. Only in this case was glenoid articular cartilage found to be severely involved in pathology. In five cases a Copeland Shoulder prosthesis (Biomet Europe, Dordrecht, Netherlands) was used. The following five cases were treated with an Epoca RH Cup (Argomedical, Cham, Switzerland).
Intraoperative joint status was recorded for the glenoid according to Walch [22]. In six cases a type A1 glenoid was found, in two cases a type A2, and in two cases a type C.
All patients were evaluated preoperatively using the Constant score adjusted for age and gender [2, 3]. Preoperative patient data can be found in Table 1. Radiographs of the shoulder were taken in anteriorposterior and axillary views (Figs. 1 and 2). Additionally, active shoulder motion was recorded (flexion, abduction, rotation in neutral position). Shoulder flexion, abduction, and external rotation were recorded in degrees; internal rotation was graded according to the posterior spinal region the thumb could reach. Pain was graded using the Constant score (0 points [severe pain] to 15 points [no pain]).
Table 1.
Preoperative patient data
| Patient | Age at surgery (years) | Additional lesions | Additional procedures | Implant | Size of bone defect(%) | Preoperative Constant score | Preoperative range of motion | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Absolute (points) | Adjusted (%) | Pain (points) | Flexion (°) | Abduction (°) | External rotation (°) | Internal rotation (region) | ||||||
| 1 | 51 | Capsular shift | Copeland | 17 | 38 | 52 | 5 | 80 | 70 | 30 | Sacrum | |
| 2 | 72 | Subscapularis tear | Refixation subscapularis | Copeland | 41 | 52 | 75 | 10 | 100 | 90 | 20 | L3 |
| 3 | 64 | Bankart fracture | ORIF | Copeland | 20 | 44 | 63 | 5 | 0 | 0 | 0 | Lateral thigh |
| 4 | 75 | Subscapularis tear | Refixation subscapularis and capsular shift | Copeland | 15 | 0 | 0 | 0 | 0 | 0 | 0 | Gluteal muscle |
| 5 | 70 | Supraspinatus tear | Labrum refixation | Copeland | 11 | 0 | 0 | 0 | 20 | 10 | 0 | Gluteal muscle |
| 6 | 63 | Labrum refixation | Epoca | 33 | 12 | 15 | 5 | 40 | 30 | 0 | Lateral thigh | |
| 7 | 68 | Supraspinatus tear | Refixation supraspinatus | Epoca | 25 | 25 | 30 | 5 | 70 | 40 | 0 | Sacrum |
| 8 | 75 | Subscapularis tear | Refixation subscapularis | Epoca | 10 | 9 | 13 | 5 | 40 | 10 | 0 | Lateral thigh |
| 9 | 67 | Supraspinatus tear | Epoca | 12 | 0 | 0 | 0 | 20 | 20 | 20 | Gluteal muscle | |
| 10 | 65 | Capsular shift | Epoca | 26 | 2 | 2 | 0 | 40 | 10 | 0 | Lateral thigh | |
| Mean | 67 | 21 | 18.2 | 25 | 3.5 | 41 | 28 | 7 | Gluteal muscle | |||
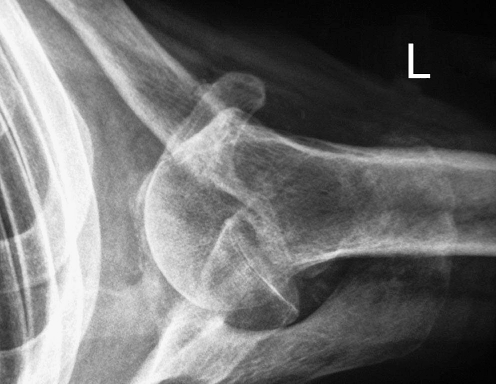
Fig. 1.

Anteriorposterior radiograph of a 65-year-old male 8 weeks after trauma with a fixed anterior glenohumeral dislocation (patient 10, Table 1)
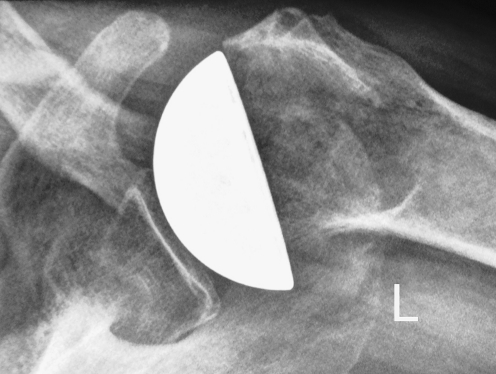
Fig. 2.
Axillary radiograph of a 65-year-old male 8 weeks after trauma with a fixed anterior glenohumeral dislocation (patient 10, Table 1)
Postoperatively, all patients were evaluated routinely at yearly intervals with the same clinical and radiographic protocol (c.f. Figs. 5 and 6). Postoperative patient data can be found in Table 2. Mean follow-up was 24 months (range, 12–42 months). The subjective result after surgery was rated in categories of “very satisfied”, “satisfied”, somewhat “disappointed”, or “very disappointed”.
Fig. 5.
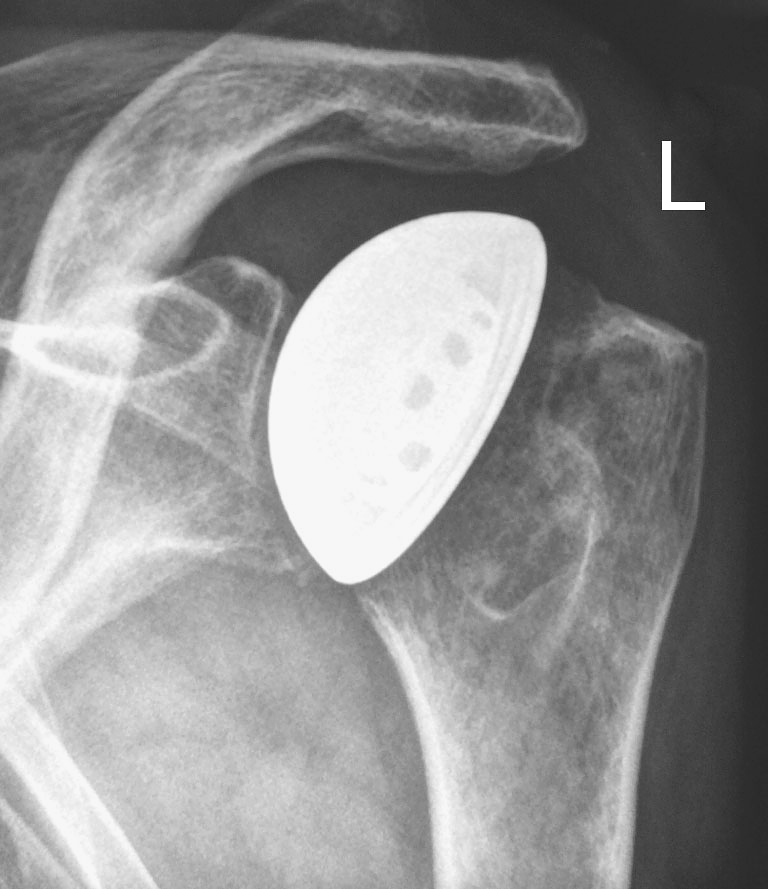
Anteriorposterior radiograph of patient 10 (Table 1), 12 months after arthroplasty
Fig. 6.
Axillary radiograph of patient 10 (Table 1), 12 months after arthroplasty
Table 2.
Postoperative patient data
| Patient | Duration of follow-up (months) | Postoperative Constant score | Postoperative range of motion | Subjective result | Complications | Reoperation | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Absolute (points) | Adjusted (%) | Pain (points) | Flexion (°) | Abduction (°) | External rotation (°) | Internal rotation (region) | |||||
| 1 | 27 | 35 | 48 | 3 | 70 | 40 | 10 | Gluteal muscle | Very disappointed | Glenoidabrasion/ pain | Total shoulder |
| 2 | 42 | 87 | 126 | 15 | 170 | 170 | 30 | Th 7 | Very satisfied | ||
| 3 | 19 | 55 | 79 | 10 | 110 | 110 | 50 | Th 12 | Satisfied | ||
| 4 | 21 | 35 | 51 | 5 | 110 | 90 | 30 | Gluteal muscle | Satisfied | ||
| 5 | 38 | 62 | 83 | 10 | 100 | 150 | 60 | Sacrum | Satisfied | ||
| 6 | 26 | 76 | 92 | 15 | 140 | 120 | 20 | Sacrum | Very satisfied | ||
| 7 | 17 | 81 | 98 | 15 | 160 | 160 | 30 | L3 | Very satisfied | ||
| 8 | 24 | 47 | 68 | 10 | 90 | 80 | 30 | L3 | Somewhat disappointed | Redislocation with rerupture of the tendon M. subscapularis | Refixation subscapularis, coracoid transfer |
| 9 | 12 | 63 | 90 | 15 | 140 | 110 | 20 | Sacrum | Very satisfied | ||
| 10 | 12 | 65 | 78 | 13 | 130 | 120 | 30 | Sacrum | Satisfied | ||
| Mean | 23.8 | 60.6 | 81.3 | 11.1 | 122 | 115 | 31 | Sacrum/L3 | Satisfied | ||
In all cases CT or MRI scans were available (Fig. 3). The sizes of the humeral head defects were calculated with an image processing program (Image J, version 1.38x, National Institute of Health, Bethesda, Maryland, USA). Therefore, the axial CT or MR image with the largest humeral head defect was evaluated in every single case. The program calculated the size of the humeral head bone stock and the size of the bone defect. The sizes of the defects were stated in percent (Tables 1 and 2).
Fig. 3.

Preoperative CT scan of a fixed anterior glenohumeral dislocation; size of the humeral head defect was calculated as 25% (patient 7, Table 1)
Operative technique and implants
In all shoulders a deltopectoral approach was used as described by Neer [16]. After detaching the subscapularis tendon and a capsular release, the joint was exposed. In all cases a large humeral head defect was found. The humeral head was reamed with hemispherical reamers decreasing in size (Fig. 4). The uncemented resurfacing implant was placed using a press-fit technique. In all cases primary stability of the implant was achieved despite the presence of the humeral head bone defect. In five cases a Copeland Shoulder (Biomet Europe, Dordrecht, Netherlands) was used and in the subsequent five cases the Epoca RH Cup (Argomedical, Cham, Switzerland) was implanted. All implants were coated with hydroxyapatite on the inner surface. All implant designs offered a spherical joint surface. Primary stability in the humeral epiphysis was achieved using a centred peg in the Copeland Shoulders; whereas, for the Epoca RH Cup, primary stability was ensured using a conical crown-shaped ring (Figs. 5 and 6). Both implants are bone sparing options for reconstruction of the humeral head surface.
Fig. 4.
Intraoperative documentation of a bone defect after preparing the humeral head with hemispherical reamers
Soft tissue reconstruction was done by a capsular shift in three cases [15]. In only two cases was the ventral labrum not destroyed but detached from its insertion at the glenoid; a reattachment with two Panalock anchors (DePuy Mitek, Inc., Raynham, MA, USA) was performed in each case. In all cases the subscapularis tendon was reattached to its insertion at the lesser tuberosity using 5–6 non-resorbable sutures. Additionally, the rotator cuff interval was reattached with resorbable sutures in two cases. Postoperatively the patients were immobilised for three weeks in a Gilchrist bandage and mobilised subsequently in the fourth and fifth weeks with shoulder flexion and abduction of 90° and 0° of external rotation. Free range of motion was allowed six weeks after operation.
Statistics
For statistical analysis the Wilcoxon signed-rank test was used to assess paired preoperative and postoperative Constant scores, range of motion, and pain measurements where P < 0.05 was considered significant.
Results
Survival and complications
In one case an additional supraspinatus tendon tear was treated in the same operation and in three cases the subscapularis tendon was repaired. In one case a re-rupture of the subscapularis tendon occurred after redislocation two weeks after arthroplasty (patient 8, Table 1). This patient was treated by a coracoid transfer and reconstruction of the subscapularis tendon; no painful complete redislocation occurred after the second operation. However, in this case a radiological anterior migration of the humeral head remained. There were no further dislocations after surgery.
In one case an erosion of the glenoid cartilage was associated with severe pain leading to revision with total shoulder arthroplasty (patient 1, Table 1).
Clinical results and patients’ satisfaction
The mean Constant score improved from 20 points preoperatively (range 0–52 points) to 61 points (range 35–87 points) postoperatively (p < 0.007), adjusted by age and gender from 25% (range 0–75%) to 81% (range 48–126%). Significant differences between pre- to postoperative Constant scores were also found for pain relief (p < 0.006), shoulder flexion and abduction (p < 0.007), and external rotation (p < 0.017). The results of clinical examinations pre- and postoperatively are shown in Table 1.
Eight patients were satisfied (n = 4) or very satisfied (n = 4) with the procedure. The patient with radiological recurrent anterior migration of the humeral head was somewhat disappointed with the result of surgery (patient 8, Table 1). One patient was very disappointed 27 months after surgery. A revision to total shoulder arthroplasty was performed (patient 1, Table 1). Thereafter, the patient was very satisfied.
Imaging results
We did not find any clinical or radiographical signs of implant loosening. The mean size of the humeral head defect was 21% (range, 10–41%). The results for all patients are shown in Table 1.
Discussion
Dislocation of the humeral head can lead to large posterior superior bone defects [25]. As presented in this study, the amount of bone loss can often exceed 10% of the humeral joint surface. These defects can mechanically lead to recurrent or permanent dislocation [8, 20]. Multiple surgical techniques have been described to avoid redislocation of the humeral head. Rotational humeral osteotomy in recurrent anterior dislocations of the shoulder was first described in 1984 by Weber [23] and Kronberg et al. [9, 10]. As an alternative treatment option, filling of the defect with humeral allograft has been proposed [5, 18]. In the treatment of larger defects caused by anterior or posterior dislocation of the humeral head, hemi- or total shoulder arthroplasty has already been described [1, 6, 14, 17, 19, 21]. Until now, there is no standard procedure for these types of lesions.
Matsoukis et al. [14] described a series of 11 patients with fixed anterior glenohumeral dislocation treated with hemi- or total shoulder arthroplasty. Seven complications in five shoulders were observed in this series with a mean follow-up of 48 months. In four cases recurrent anterior dislocation took place, and in two of these cases glenoid loosening occurred. Bone graft migration was described in one case. In another case removal of a screw was performed, and in one case removal of a glenoid component was performed in a revision surgery. The authors report an age and gender adjusted Constant score of 60% 48 months after operation with a mean active shoulder abduction of 90° and a mean active external rotation of 26°.
In this study good functional results were found after resurfacing the humeral head. At 24 months postoperatively, a mean age and gender adjusted Constant score of 81% was measured in this cohort, which can be considered as a good result after this type of injury. Moreover, a significant improvement of the Constant score for shoulder flexion, abduction, rotation, and pain was found. Out of ten patients, two complications in two shoulders were observed, both treated by revision surgery.
We were able to successfully avoid the mechanism of redislocation by restoration of the joint congruency using CHSRA and reconstruction of the anterior part of the force couple in most cases.
We did not observe any clinical or radiographical signs of implant loosening in our group. Obviously, the uncemented implant gained sufficient primary stability for secondary osteointegration even in the presence of a large humeral head defect. However, sufficient humeral bone stock is crucial for adequate primary stability of the CHSRA for secondary osteointegration. In bone defects of more than 45% of the humeral surface we believe that adequate stability will be hard to achieve with CHSRA and suggest treatment with a conventional hemiarthroplasty. In younger patients (<50 years) we would suggest humeral head preserving surgery techniques such as reorientation of the humeral head [9, 23] or filling the defect with humeral allograft [18]. In our opinion, reconstruction of the rotator cuff, especially of the subscapularis tendon, is crucial to avoid redislocation and gain good clinical results.
The weakness of this study is the relatively low number of cases. However, fixed anterior glenohumeral dislocation in combination with large humeral defects is a rare condition. The above-mentioned studies [14, 21] also presented low numbers with a maximum of 11 [14] patients for anterior dislocation and 12 patients [21] for posterior dislocation treated with shoulder arthroplasty.
In this study we were able to present CHSRA as a viable and bone preserving treatment option for joint congruency and stability restoration in elderly patients with fixed anterior shoulder dislocation with large humeral head defects. Later conversion to total shoulder replacement in cases of secondary glenoid erosion is possible. Mid- and long-term results are necessary to confirm these observations.
Acknowledgements
This study was supported by the “Deutsche Arthrose-Hilfe e.V.”
Footnotes
The first and second authors contributed equally to this study.
References
- 1.Cheng SL, Mackay MB, Richards RR. Treatment of locked posterior fracture-dislocations of the shoulder by total shoulder arthroplasty. J Shoulder Elbow Surg. 1997;6:11–17. doi: 10.1016/S1058-2746(97)90065-3. [DOI] [PubMed] [Google Scholar]
- 2.Constant CR. An evaluation of the Constant-Murley shoulder assessment. J Bone Joint Surg Br. 1997;79:695–696. [PubMed] [Google Scholar]
- 3.Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–165 [PubMed]
- 4.Gebhard F, Draeger M, Steinmann R, Hoellen I, Hartel W. Functional outcome of Eden-Hybinette-Lange operation in post-traumatic recurrent shoulder dislocation. Unfallchirurg. 1997;100:770–775. doi: 10.1007/s001130050191. [DOI] [PubMed] [Google Scholar]
- 5.Gerber C, Lambert SM. Allograft reconstruction of segmental defects of the humeral head for the treatment of chronic locked posterior dislocation of the shoulder. J Bone Joint Surg Am. 1996;78:376–382. doi: 10.2106/00004623-199603000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Hawkins RJ, Neer CS, Pianta RM, Mendoza FX. Locked posterior dislocation of the shoulder. J Bone Joint Surg Am. 1987;69:9–18. [PubMed] [Google Scholar]
- 7.Helfet AJ. Coracoid transplantation for recurring dislocation of the shoulder. J Bone Joint Surg Br. 1958;40B:198–202. doi: 10.1302/0301-620X.40B2.198. [DOI] [PubMed] [Google Scholar]
- 8.Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg Am. 1996;78:1677–1684. doi: 10.2106/00004623-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Kronberg M, Brostrom LA. Proximal humeral osteotomy to correct the anatomy in patients with recurrent shoulder dislocations. J Orthop Trauma. 1991;5:129–133. doi: 10.1097/00005131-199105020-00002. [DOI] [PubMed] [Google Scholar]
- 10.Kronberg M, Brostrom LA. Rotation osteotomy of the proximal humerus to stabilise the shoulder. Five years' experience. J Bone Joint Surg Br. 1995;77:924–927. [PubMed] [Google Scholar]
- 11.Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49:994–997. [PubMed] [Google Scholar]
- 12.Levy O, Copeland SA. Cementless surface replacement arthroplasty of the shoulder. 5- to 10-year results with the Copeland mark-2 prosthesis. J Bone Joint Surg Br. 2001;83:213–221. doi: 10.1302/0301-620X.83B2.11238. [DOI] [PubMed] [Google Scholar]
- 13.Levy O, Copeland SA. Cementless surface replacement arthroplasty (Copeland CSRA) for osteoarthritis of the shoulder. J Shoulder Elbow Surg. 2004;13:266–271. doi: 10.1016/j.jse.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 14.Matsoukis J, Tabib W, Guiffault P, Mandelbaum A, Walch G, Nemoz C, Cortes ZE, Edwards TB. Primary unconstrained shoulder arthroplasty in patients with a fixed anterior glenohumeral dislocation. J Bone Joint Surg Am. 2006;88:547–552. doi: 10.2106/JBJS.E.00368. [DOI] [PubMed] [Google Scholar]
- 15.Neer CS, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am. 1980;62:897–908. [PubMed] [Google Scholar]
- 16.Neer CS, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982;64:319–337. [PubMed] [Google Scholar]
- 17.Pritchett JW, Clark JM (1987) Prosthetic replacement for chronic unreduced dislocations of the shoulder. Clin Orthop Relat Res 89–93 [PubMed]
- 18.Re P, Gallo RA, Richmond JC. Transhumeral head plasty for large Hill-Sachs lesions. Arthroscopy. 2006;22:798. doi: 10.1016/j.arthro.2005.12.038. [DOI] [PubMed] [Google Scholar]
- 19.Rowe CR, Zarins B. Chronic unreduced dislocations of the shoulder. J Bone Joint Surg Am. 1982;64:494–505. [PubMed] [Google Scholar]
- 20.Rowe CR, Zarins B, Ciullo JV. Recurrent anterior dislocation of the shoulder after surgical repair. Apparent causes of failure and treatment. J Bone Joint Surg Am. 1984;66:159–168. [PubMed] [Google Scholar]
- 21.Sperling JW, Pring M, Antuna SA, Cofield RH. Shoulder arthroplasty for locked posterior dislocation of the shoulder. J Shoulder Elbow Surg. 2004;13:522–527. doi: 10.1016/j.jse.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 22.Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999;14:756–760. doi: 10.1016/S0883-5403(99)90232-2. [DOI] [PubMed] [Google Scholar]
- 23.Weber BG, Simpson LA, Hardegger F. Rotational humeral osteotomy for recurrent anterior dislocation of the shoulder associated with a large Hill-Sachs lesion. J Bone Joint Surg Am. 1984;66:1443–1450. [PubMed] [Google Scholar]
- 24.Wehner W. Eden-Hybinette-Lange surgical treatment of habitual shoulder dislocation. Zentralbl Chir. 1972;97:837–842. [PubMed] [Google Scholar]
- 25.Widjaja AB, Tran A, Bailey M, Proper S. Correlation between Bankart and Hill-Sachs lesions in anterior shoulder dislocation. ANZ J Surg. 2006;76:436–438. doi: 10.1111/j.1445-2197.2006.03760.x. [DOI] [PubMed] [Google Scholar]