Abstract
A systematic review of the English literature over the last 30 years was conducted in order to investigate the correlation of the clinical outcome of different types of pelvic ring injuries to the method of treatment. Three basic therapeutic approaches were analysed: non-operative treatment (group A), stabilisation of anterior pelvis (group B) and internal fixation of posterior pelvis (group C). Of 818 retrieved reports, 27 case series, with 28 groups of patients and 1,641 patients, met our inclusion criteria. The quality of the literature was evaluated using a structured questionnaire. Outcomes of the eligible studies were summarised by the medians of the reported results. Most of the component studies were of fair or poor quality. Certain radiological results (quality of reduction, malunion rates) were significantly better in group C. From the functional point of view only walking capacity was proved to be significantly better in the groups of operative treatment compared to the non-operative group.
Résumé
Une revue systématique de la littérature anglo-saxonne sur les 30 dernières années a été réalisée de façon à analyser les corrélations concernant le devenir clinique des différents traumatismes du bassin et leurs méthodes de traitement. Trois approches thérapeutiques ont été analysées, les traitements orthopédiques (Groupe A), stabilisation du bassin antérieur (Groupe B) et fixation interne du bassin antérieur (Groupe C). 818 articles analysés, 27 séries représentant 28 groupes de patients (1641 patients) ont été inclus. La qualité de la littérature a été évaluée en utilisant un questionnaire structuré. La plupart des études sont de peu d'intérêt. Certains résultats radiologiques, (qualité de la réduction, pseudarthrose) sont significativement meilleur dans le groupe C. Enfin sur le plan fonctionnel et sur le plan de la récupération de la marche, il existe une différence significative bien meilleure dans les groupes ayant bénéficié d'un traitement chirurgical comparé au groupe traité orthopédiquement.
Introduction
Pelvic ring disruptions are relatively uncommon injuries with a prevalence of 20-37/100,000 of the general population [7]. Moreover, in the polytrauma setting their prevalence rises to 20%, contributing significantly to its high morbidity and mortality [21, 29].
Although in the past most of the pelvic fractures were managed non-operatively, advances in fixation techniques and a clearer understanding of biomechanics led to more “aggressive” approaches [36]. Fixation of the anterior ring, particularly with external fixators, gained an invaluable role in acute management. Several authors advocate its use also for the definitive treatment of certain fracture types [34]. The involvement of the posterior osseous-ligamentous elements is often underestimated, according to cadaveric and clinical studies [1]. Therefore, a significant number of surgeons strongly support the fixation of the posterior elements [8, 40].
Many factors have been associated with the long-term disability of pelvic fractures. The type of pelvic injury, the neurovascular status and the associated trauma to different organs precede medical interventions and are out of the control of the surgeon [32]. Conversely, the poor quality of reduction and residual pelvic deformity are associated with the applied treatment methods, produce chronic pain and compromise the final functional outcome [24, 38]. These factors are influenced by the chosen therapeutic strategy and the expertise of the surgeon.
In order to elicit these aspects of pelvic trauma, we conducted a systematic review to investigate the impact of different therapeutic approaches on quality and maintenance of reduction, short-term clinical results and long-term functional outcome.
Patients and methods
An electronic search of MEDLINE between January 1975 and March 2007 was performed, entering the following terms and Boolean operators: pelvic ring fracture AND outcome. We limited our results to “humans” and “English language”. The references of the retrieved articles were also searched for earlier eligible reports. Eligibility was assessed according to specific inclusion and exclusion criteria (Table 1).
Table 1.
Inclusion and exclusion criteria used in the literature review and evaluation scheme on the quality of the reviewed studies (maximum score 12)
| Inclusion criteria | Exclusion criteria | |||
|---|---|---|---|---|
| 1 | Series of at least 15 patients | 1 | Experimental studies | |
| 2 | Clear reporting on the results of treatment | 2 | Paediatric cohorts (age < 14 years) | |
| 3 | Clear description on the method of treatment | 3 | Open pelvic fractures | |
| 4 | Clear description of at least one of the outcomes of interest | 4 | Isolated sacral or acetabular fractures | |
| Questions | Answer yes and RCT | Answer yes and non-RCT | Answer yes and case series | |
| 1 | Were the reviewers of the outcomes blinded to treatment? | 3 | 2 | 1 |
| 2 | Was the follow-up rate > 80%? | 3 | 2 | 1 |
| 3 | Were the follow-up intervals pre-specified? | 3 | 2 | 1 |
| 4 | Was any particular functional score used? | 3 | 2 | 1 |
RCT randomised controlled trial, non-RCT non-randomised controlled trial
Two independently working researchers (CP, NKK) reviewed each retrieved citation. If a citation could not be excluded unequivocally, the two reviewers reviewed the complete report and discussed its eligibility. The search process was not blinded to the authors’ names, institutions or journals to avoid duplication of data.
Three different rationales of pelvic fracture management comprised our comparative groups:
“Non-operative management” (solely non-operative means were used—bed-rest, pelvic sling, skeletal traction, spica casts etc.—irrespective of fracture type).
“Anterior pelvic fixation” (fixation limited to the anterior pelvic ring—external fixators or plate fixation—even in the presence of disruption of the posterior complex).
“Posterior pelvic fixation” (vertically/rotationally unstable pelvic fractures managed with internal fixation of posterior pelvis—with/without supplementary anterior fixation).
Short-term clinical results were evaluated in terms of union, malunion, infection, loss of reduction and implant failure rates. Long-term functional outcome evaluation was based either on validated functional scoring systems or on simple documentation of residual pain, alteration of walking capacity and return of the employed patients to their previous occupation.
Unfortunately, we were unable to locate relevant randomised controlled trials (RCTs) and thus, we had to rely on case series studies. To avoid corruption of our results due to the inherent weaknesses, we established a strict protocol and developed a quality scoring system. The quality of each eligible study was evaluated in respect to the research design and the follow-up process. Evaluation of the follow-up process was based on the answers to four specific questions (maximum score of 12) (Table 1).
Descriptive characteristics recorded were the publication year, study type, sample size, mean age, male/female ratio, follow-up rate, mean time of follow-up, percentage of open pelvic fractures, type of pelvic injury, type of posterior lesion, injury severity score (ISS), mortality, incidence of associated injuries, lumbosacral plexus injury and genitourinary dysfunction. The main outcomes of interest were quality of reduction, rates of union, malunion, infection, pin track infection, loss of reduction, implant failure, pain, walking capacity and return to previous occupation. Clear definitions were used to avoid confusion and inconsistency.
Lumbosacral plexus injury was considered present if an objective loss of motor function in the lower extremities or of bowel control was documented. Subjective paraesthesias along lower extremities or the perineal region were excluded.
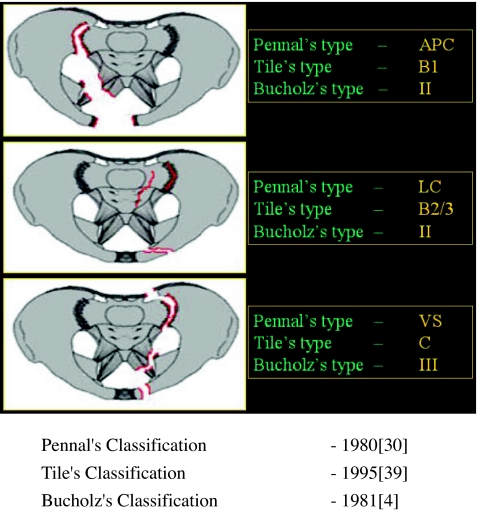
The documentation of the type of pelvic ring injury was based on Pennal’s classification [30]. Several authors reported their results based on either Tile’s [39] or Bucholz’s [4] systems. In such cases we grouped the different subgroups according to the scheme of Fig. 1.
Fig. 1.
The different classification schemes and the correlation of their subgroups between each other
The type of posterior lesion was grouped into four categories: sacral fractures, pure sacroiliac dislocations, sacroiliac fracture-dislocations and transiliac fractures. The incidence of each type was expressed as a proportion (p) to the total number of posterior lesions in each report.
Quality of reduction was graded as excellent, good or poor based on the degree of residual displacement of the hemipelvis or the diastasis of the pubic symphysis. The reduction was “excellent” when anteroposterior translation or vertical displacement was < 5 mm or the symphysis pubis diastasis was < 10 mm. The reduction was “good” or “poor” when displacement was within 5-10 mm or > 10 mm and/or diastasis 10-25 mm or > 25 mm, respectively.
Fracture union was assumed when bone healing progressed uneventfully without secondary interventions. Malunion was considered in cases of leg length discrepancy > 1 cm, obvious malrotation of the lower limbs or when the criteria of “poor” reduction were fulfilled.
The rate of pin track infection was calculated as a percentage of the patients that had been treated with external fixation.
Pain was grouped as: (1) no pain at any level of activity, (2) mild, or intermittent pain, necessitating analgesics occasionally and (3) severe pain restricting normal activity, or continuous pain at rest, needing analgesics regularly.
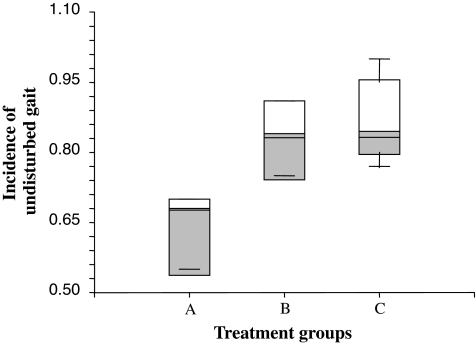
The incidence of undisturbed walking capacity was calculated as the percentage of patients without any alteration of their walking ability compared to their pre-injury status.
Each cohort of patients was assigned to one of the three treatment groups (A-B-C). The median value of each outcome of interest was calculated. The medians across all three groups were compared using the Kruskal-Wallis test (non-parametric one-way analysis of variance). Comparisons across two groups were done using the Mann-Whitney U test. Differences were considered significant at p < 0.05. The agreement between the two reviewers was evaluated by the correlation coefficient (r) for inter-rater agreement and the intraclass correlation coefficient (ICC).
Results
The electronic search yielded 818 citations, but only 17 met the inclusion criteria [5, 6, 9, 10, 12–14, 17–19, 23, 25, 27, 28, 31, 41, 42]. Another ten eligible studies were obtained from the detailed search of the references of the electronically retrieved studies [3, 11, 15, 16, 22, 26, 33, 35, 37, 44]. Two reports represented prospective studies [12, 28], while the remaining 25 were retrospective case series.
One study [22] yielded two eligible patient cohorts (groups A and C). Consequently, a total of 28 “patient cohorts” were identified. Four cohorts [10, 22, 26, 35] (153 patients) were assigned to group A (non-operative treatment), 8 cohorts [6, 15, 18, 19, 25, 27, 37, 44] (640 patients) to group B (anterior pelvic fixation) and 16 cohorts [3, 5, 9, 11–14, 16, 17, 22, 23, 28, 31, 33, 41, 42] (848 patients) to group C (posterior pelvic fixation) (Table 2).
Table 2.
Presentation of the reviewed studies grouped into the three different cohorts according to the treatment strategy (“non-operative”, “anterior pelvic fixation” and “posterior pelvic fixation”)
| Pattern of injury | Type of stabilisation of pelvis | Type of surgery | |||||||
|---|---|---|---|---|---|---|---|---|---|
| APC (p) | LC (p) | VS (p) | Anterior (p) | Posterior (p) | Ant. + poster. (p) | Non–operative (p) | EF (p) | IF (p) | |
| Non-operative group | |||||||||
| Monahan and Taylor [26] 1975 | n.d. | n.d. | n.d. | – | – | – | 1 | 0 | 0 |
| Semba et al. [35] 1983 | 0 | 0 | 1 | – | – | – | 1 | 0 | 0 |
| Matta and Saucedo [22] 1989a | 0.08b | 0.92 | – | – | – | 1 | 0 | 0 | |
| Henderson [10] 1989 | 0.15 | 0.65 | 0.19 | – | – | – | 1 | 0 | 0 |
| Anterior pelvic fixation group | |||||||||
| Slatis and Karaharju [37] 1980 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 |
| Wild et al. [44] 1982 | 0.31 | 0.4 | 0.29 | 1 | 0 | 0 | 0 | 1 | 0 |
| Lansinger et al. [15] 1984 | 0.25 | 0.44 | 0.31 | 1 | 0 | 0 | 0 | 1 | 0 |
| Majeed [19] 1990 | 0.48 | 0.26 | 0.26 | 1 | 0 | 0 | 0 | 1 | 0 |
| Miranda et al. [25] 1996 | 0.39b | 0.3c | 0.6 | 0 | 0 | 0.4 | 0.6 | 0 | |
| Dujardin et al. [6] 1998 | 0.41 | 0.25 | 0.34 | 0.59 | 0 | 0 | 0.41 | 0.39 | 0.20 |
| Nepola et al. [27] 1999 | 0 | 0 | 1 | 0.85 | 0 | 0 | 0.15 | 0.85 | 0 |
| Lindahl et al. [18] 1999 | 0.07 | 0.56 | 0.36 | 1 | 0 | 0 | 0 | 1 | 0 |
| Posterior pelvic fixation group | |||||||||
| Browner et al. [3] 1987 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 |
| Matta and Saucedo [22] 1989§ | 0.22b | 0.78 | 0.22 | 0.53 | 0.25 | 0 | 0 | 1 | |
| Leung et al. [16] 1992 | 0.07 | 0.18 | 0.75 | 0.07 | 0 | 0.93 | 0 | 0.5 | 0.93 |
| Ragnarsson et al. [33] 1993 | 0 | 0 | 1 | 0 | 0.14 | 0.86 | 0 | 0.57 | 1 |
| Hirvensalo et al. [11] 1993 | 0.17 | 0.44 | 0.39 | 0.61 | 0 | 0.39 | 0 | 0 | 1 |
| Pohlemann et al. [31] 1994 | 0.48b | 0.52 | 0.48 | 0 | 0.52 | 0 | n.d. | n.d. | |
| Gruen et al. [9] 1995 | 0.19 | 0.15 | 0.17 | 0 | 0.71 | 0.29 | 0 | 0 | 1 |
| Tornetta and Matta [41] 1996 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 |
| Matta and Tornetta [23] 1996 | 0.36b | 0.64 | 0.29 | 0.40 | 0.31 | 0 | 0 | 1 | |
| Cole et al. [5] 1996 | 0 | 0 | 1 | 0 | 0.91 | 0.09 | 0 | 0.05 | 1 |
| Oliver et al. [28] 1996 | 0.14 | 0.17 | 0.69 | 0.06 | 0.11 | 0.83 | 0 | 0 | 1 |
| Keating et al. [13] 1999 | 0 | 0 | 1 | 0 | 0.18 | 0.82 | 0 | 0.39 | 1 |
| Van den Bosch et al. [42] 1999 | 0.08 | 0.35 | 0.57 | 0.43 | 0 | 0.57 | 0 | 0.30 | 1 |
| Korovessis et al. [14] 2000 | 0.03 | 0.36 | 0.61 | 0 | 0 | 1 | 0 | 0.08 | 1 |
| Kabak et al. [12] 2003 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 |
| Lindahl and Hirvensalo [17] 2005 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 |
APC anteroposterior compression, p proportion of fractures, LC lateral compression, VS vertical shear, EF external fixation, IF internal fixation, n.d. not defined
aPatient cohorts of conservative treatment and posterior pelvic internal fixation, respectively
bBucholz type II
cAnother proportion of 0.31 of undisplaced fractures were included in this series
Quality of reviewed studies
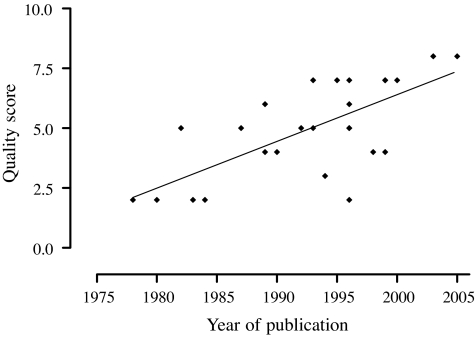
The median quality score was 5 points (range: 2-8). The correlation coefficient for inter-rater agreement was 0.78 (p < 0.05). The intraclass correlation coefficient (ICC) was 0.79 [95% confidence interval (CI): 0.59-0.90]. Study quality improved by about 0.2 points per year, as indicated by linear regression analysis (p < 0.001) (Fig. 2).
Fig. 2.
The improvement of the reported data of the reviewed studies in time. The linear regression analysis of the quality score of these studies showed an increase of 0.2 points per year (median score: 5, range: 2-8). In Table 3 the median score is presented grouped per different method of treatment (groups A, B and C)
Descriptive characteristics
The three treatment groups were similar with respect to all but two of the descriptive characteristics (“publication year” and “mean age”) (Table 3).
Table 3.
General characteristics of the reviewed studies including year of publication, quality of reviewed studies, demographics, type of pelvic injury, associated injuries, injury severity and follow-up period
| Group A (non-operative treatment) | Group B (anterior pelvic fixation) | Group C (internal fixation of posterior pelvis) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Parameter | No. of studies (pts) | Median value | Range | No. of studies (pts) | Median value | Range | No. of studies (pts) | Median value | Range | p value |
| Quality score | 4 [10, 22, 26, 35] (n = 153) | 3 | 2-6 | 8 [6, 15, 18, 19, 25, 27, 37, 44] (n = 640) | 4.5 | 2-7 | 16 [3, 5, 9, 11–14, 16, 17, 22, 23, 28, 31, 33, 41, 42] (n = 848) | 5.5 | 2-8 | 0.10 |
| Year of publication | 4 [10, 22, 26, 35] (n = 153) | 1986 | 1978-1989 | 8 [6, 15, 18, 19, 25, 27, 37, 44] (n = 640) | 1993 | 1980-1999 | 16 [3, 5, 9, 11–14, 16, 17, 22, 23, 28, 31, 33, 41, 42] (n = 848) | 1996 | 1987-2005 | 0.03 |
| No. of patients | 4 [10, 22, 26, 35] (n = 153) | 38 | 24-53 | 8 [6, 15, 18, 19, 25, 27, 37, 44] (n = 640) | 56 | 17-180 | 16 [3, 5, 9, 11–14, 16, 17, 22, 23, 28, 31, 33, 41, 42] (n = 848) | 47 | 15-222 | 0.53 |
| Fup rates | 4 [10, 22, 26, 35] (n = 153) | 73% | 57-94% | 8 [6, 15, 18, 19, 25, 27, 37, 44] (n = 640) | 75% | 44-100 | 16 [3, 5, 9, 11–14, 16, 17, 22, 23, 28, 31, 33, 41, 42] (n = 848) | 84% | 64-100% | 0.13 |
| Mean Fup (months) | 3 [10, 22, 26] (n = 100) | 42 | 15-96 | 6 [6, 15, 18, 19, 25, 27] (n = 566) | 52.1 | 36-86.4 | 13 [5, 9, 11, 12, 14, 16, 17, 22, 28, 31, 33, 41, 42] (n = 688) | 26.4 | 15-71 | 0.1 |
| Mean age (years) | 4 [10, 22, 26, 35] (n = 153) | 30.7 | 27-30.9 | 7 [6, 15, 18, 19, 25, 27, 37] (n = 595) | 37 | 26-39 | 15 [3, 5, 9, 11–14, 16, 17, 22, 28, 31, 33, 41, 42] (n = 741) | 33 | 29-37 | 0.02 |
| Gender M/F ratio | 4 [10, 22, 26, 35] (n = 153) | 1.53 | 1.41-7.6 | 8 [6, 15, 18, 19, 25, 27, 37, 44] (n = 640) | 1.46 | 0.8-4.3 | 14 [3, 5, 9, 11–14, 16, 17, 22, 28, 31, 33, 42] (n = 672) | 1.85 | 1.2-3.7 | 0.5 |
| % Open fractures | 2 [10, 22] (n = 57) | 12% | 9-15% | 2 [18, 44] (n = 177) | 4% | 4-4% | 12 [3, 5, 9, 12–14, 16, 17, 22, 23, 28, 42] (n = 667) | 7.5% | 3-26% | 0.16 |
| ISS | 0 | 2 [18, 25] (n = 312) | 24.5 | 24-25 | 9 [3, 5, 9, 12, 13, 16, 17, 28, 42] (n = 454) | 27 | 16.7-30.4 | 0.34 | ||
| Mortality | 2 [26, 35] (n = 96) | 13% | 9-17% | 6 [6, 15, 18, 19, 37, 44] (n = 427) | 6.5% | 3-12% | 9 [9, 12–14, 16, 17, 28, 31, 42] (n = 522) | 4% | 3-11% | 0.13 |
| Incidence of associated injuries | 3 [22, 26, 35] (n = 120) | 51% | 43-91% | 5 [6, 15, 19, 37, 44] (n = 295) | 74% | 49-84% | 6 [9, 13, 14, 22, 23, 33] (n = 326) | 82.5% | 43-90% | 0.73 |
| Incidence of L/S plexus injury | 4 [10, 22, 26, 35] (n = 153) | 39.5% | 30-43% | 4 [15, 18, 19, 37] (n = 244) | 29.5% | 5-42% | 15 [3, 5, 9, 11–14, 16, 17, 23, 28, 31, 33, 41, 42] (n = 830) | 30% | 8-47% | 0.26 |
| Incidence of G/U dysfunction | 2 [26, 35] (n = 96) | 8.5% | 0-17% | 2 [25, 27] (n = 213) | 34.5% | 33-36% | 10 [5, 12, 13, 16, 17, 28, 31, 33, 41, 42] (n = 548) | 15% | 4-29% | 0.12 |
| Type of injury | ||||||||||
| % APC | 2 [10, 35] (n = 86) | 7.5% | 0-15% | 7 [6, 15, 18, 19, 27, 37, 44] (n = 460) | 25% | 0-48 | 13 [3, 5, 9, 11–14, 16, 17, 28, 33, 41, 42] (n = 636) | 0% | 0-19% | 0.18 |
| % LC | 2 [10, 35] (n = 86) | 32.5% | 0-65% | 7 [6, 15, 18, 19, 27, 37, 44] (n = 460) | 26% | 0-56% | 13 [3, 5, 9, 11–14, 16, 17, 28, 33, 41, 42] (n = 636) | 0% | 0-44% | 0.29 |
| % VS | 3 [10, 22, 35] (n = 110) | 92% | 19-100% | 8 [6, 15, 18, 19, 25, 27, 37, 44] (n = 640) | 33% | 26-100% | 16 [3, 5, 9, 11–14, 16, 17, 22, 23, 28, 31, 33, 41, 42] (n = 848) | 77% | 39-100% | 0.08 |
| Type of posterior lesion | ||||||||||
| p-Sacral fractures | 3 [10, 26, 35] (n = 129) | 0.4 | 0.26-0.42 | 3 [6, 27, 44] (n = 216) | 0.34 | 0.29-0.42 | 6 [5, 11, 12, 13, 23, 41] (n = 336) | 0.23 | 0.05-0.58 | 0.28 |
| p-SI dislocations | 2 [10, 35] (n = 86) | 0.36 | 0.26-0.45 | 1 [6] (n = 138) | 0.38 | 6 [5, 11, 12, 13, 23, 41] (n = 336) | 0.32 | 0.11-0.42 | 0.86 | |
| p-SI fracture/dislocations | 1 [10] (n = 33) | 0.29 | 2 [6, 44] (n = 183) | 0.17 | 0.16-0.17 | 4 [5, 12, 23, 41] (n = 280) | 0.46 | 0.26-0.5 | 0.13 | |
| p-Transiliac fractures | 2 [10, 35] (n = 86) | 0.09 | 0.03-0.15 | 2 [6, 44] (n = 183) | 0.18 | 0.11-0.24 | 4 [5, 12, 23, 41] (n = 229) | 0.06 | 0.05-0.15 | 0.4 |
APC anteroposterior compression, F female, Fup follow-up, G/U genitourinary, ISS Injury Severity Score, LC lateral compression, L/S: lumbosacral, M male, n number, p-SI proportion of sacroiliac, pts patients, VS vertical shear
The median year of publication for group A was 1986 (1978-1989), 1993 for group B (1980-1999) and 1996 for group C (1987-2005) (p = 0.03).
Mean age was documented in all papers of group A [10, 22, 26, 35], in 7 of group B [6, 15, 18, 19, 25, 27, 37] and in 15 of group C [3, 5, 9, 11–14, 16, 17, 22, 28, 31, 33, 41, 42]. The median values were 30.7, 37 and 33 years, respectively (p = 0.02).
The proportion of vertical shear injuries also differed in the three treatment groups. In group A the median value was 92%, in group B 33% and in group C 77%. However, this difference did not surpass the threshold of statistical significance (p = 0.08).
Outcome measures
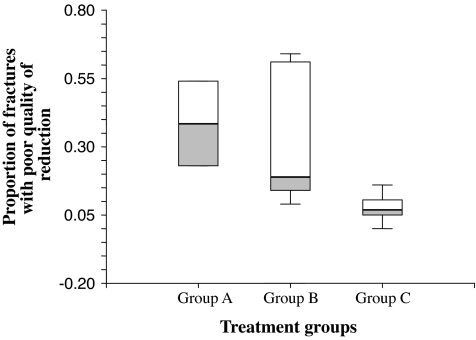
Quality of reduction
Excellent quality of reduction was observed in 46% of 33 patients [10] of group A, in 43.5% of 415 patients [6, 15, 18, 19, 27, 37] of group B and in 73% of 652 patients [3, 5, 9, 11, 12, 14, 17, 23, 31, 33, 41] of group C (p = 0.06). Excluding the “non-operative group”, we found a statistically significant difference between groups B and C (p = 0.04) (Fig. 3).
Fig. 3.
The incidence of poor residual reduction (anteroposterior translation or vertical displacement > 10 mm and/or diastasis of pubic symphysis > 25 mm) in the three different groups showed statistical significant differences (p = 0.004). In the non-operative group (group A) poor quality reduction was recorded in 38.5%, in comparison to 19% in the “anterior pelvic fixation” (group B), and only 7% in the “posterior fixation group (group C). The grey areas on the chart represent the above rates of poor quality of reduction in the three groups
Good quality of reduction was documented as 40% in group A [10], 23% in group B [15, 18, 19, 27, 37] and 19% in group C [3, 5, 9, 11, 12, 14, 17, 23, 31, 33, 41] (p = 0.28).
Poor quality of reduction was observed in 38.5% of group A [10, 22], 19% of group B [15, 18, 19, 27, 37] and 7% in group C [3, 5, 9, 11–14, 16, 17, 22, 23, 31, 33, 41] (p = 0.004).
Short-term clinical results
Union rates
Union rates were recorded in only one study [22] of group A and reached 83%; it was 100% in five studies [15, 18, 19, 27, 37] of group B (95-100%) and in 12 studies [5, 9, 11–14, 16, 17, 22, 23, 33, 42] of group C (93-100%) (p = 0.14) (Table 4).
Table 4.
Short-term clinical results reported in the reviewed studies expressed in terms of union, malunion, infection, loss of reduction and implant failure rates
| Group A (non-operative treatment) | Group B (anterior pelvic fixation) | Group C (internal fixation of posterior pelvis) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | No. of studies (pts) | Median value | Range | No. of studies (pts) | Median value | Range | No. of studies (pts) | Median value | Range | p value |
| Quality of reduction | ||||||||||
| % Excellent | 1 [10] (n = 33) | 46% | 46% | 6 [6, 15, 18, 19, 27, 37] (n = 415) | 43.5% | 9-68% | 11 [3, 5, 9, 11, 12, 14, 17, 23, 31, 33, 41] (n = 652) | 73% | 20-100% | 0.06 |
| 0.04a | ||||||||||
| % Good | 1 [10] (n = 33) | 31% | 31% | 5 [15, 18, 19, 27, 37] (n = 277) | 23% | 15-37% | 11 [3, 5, 9, 11, 12, 14, 17, 23, 31, 33, 41] (n = 652) | 19% | 0-70% | 0.28 |
| % Poor | 2 [10, 22] (n = 57) | 38.5% | 23-54% | 5 [15, 18, 19, 27, 37] (n = 277) | 19% | 9-64% | 14 [3, 5, 9, 11, 12–14, 16, 17, 22, 23, 31, 33, 41] (n = 756) | 7% | 0-16% | 0.004 |
| Union rates | 1 [22] (n = 24) | 83% | 83% | 5 [15, 18, 19, 27, 37] (n = 277) | 100% | 95-100% | 12 [5, 9, 11, 12–14, 16, 17, 23, 22, 33, 42] (n = 636) | 100% | 93-100% | 0.14 |
| Malunion rates | 2 [10, 22] (n = 57) | 30.3% | 23-37.5% | 5 [15, 18, 19, 27, 37] (n = 277) | 42% | 9-64% | 10 [3, 9, 11–14, 17, 22, 23, 33] (n = 516) | 7% | 0-44% | 0.02 |
| Infection rates | 2 [10, 35] (n = 86) | 6.7% | 1.9-11.5% | 2 [15, 44] (n = 61) | 0% | 0% | 12 [3, 5, 9, 11, 12–14, 16, 17, 22, 23, 42] (n = 544) | 5.5% | 0-12.5% | 0.15 |
| Pin track infection rates | 4 [15, 18, 19, 44] (n = 260) | 22.9% | 0-33.3% | 4 [5, 13, 14, 16] (n = 210) | 20.6% | 5.8-33.3% | 1a | |||
| Loss of reduction rates | 4 [15, 18, 37, 44] (n = 222) | 8.5% | 0-57% | 8 [3, 11–14, 17, 23, 33] (n = 430) | 5% | 0-26% | 0.6a | |||
| Implant failure rates | 2 [15, 44] (n = 148) | 1% | 0-2% | 7 [5, 12, 14, 17, 22, 23, 28] (n = 455) | 5% | 2-17.3% | 0.07a | |||
n number, p proportion of pelvic fractures, pts patients
aMann-Whitney U test between groups B and C
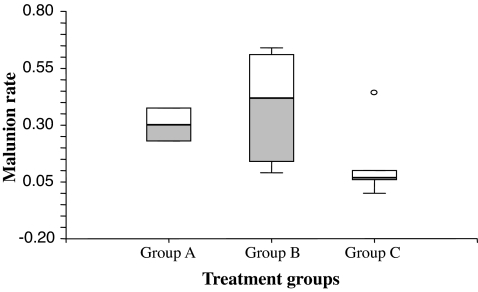
Complications
Malunion rate was documented in 57 patients of group A [10, 22], 277 patients of group B [15, 18, 19, 27, 37] and 516 patients of group C [3, 9, 11–14, 17, 22, 23, 33]. Malunion median rates were 30.3, 42 and 7%, respectively (p = 0.02) (Fig. 4).
Fig. 4.
The incidence of malunions (leg length discrepancy > 1 cm, obvious malrotation or “poor” quality of reduction) as recorded in the three different treatment groups showed statistically significant differences (p = 0.02). In the non-operative group (group A) malunions were recorded in 30.3%, in comparison to 42% in the “anterior pelvic fixation” (group B), and only 7% in the “posterior fixation group (group C). The grey areas on the chart represent the above rates of malunion in the three groups
Data regarding infection rates (median: 6.7%, range: 1.9-11.5%) were provided in two [10, 35] group A papers. In this particular treatment group the cause of infection was the presence of open pelvic injuries. Only two [15, 44] group B papers yielded relative information. In both studies infection rate was 0%. Twelve [3, 5, 9, 11–14, 16, 17, 22, 33, 42] group C papers reported a median infection rate of 5.5% (range: 0-12.5%) (p = 0.15).
Pin track infection was recorded in a median incidence of 22.9% (range: 0-33.3%) in 260 patients of group B [15, 18, 19, 44] and of 20.6% (5.8-33.3%) in 210 patients of group C [5, 13, 14, 16] (p = 1).
Loss of reduction was 8.5% (range: 0-57%) in four group B [15, 18, 37, 44] and 5% (0-26%) in eight group C manuscripts [3, 11–14, 17, 23, 33] (p = 0.6).
Implant failure was documented in only two group B studies [15, 17] and was found in 1% of 148 patients (range: 0-2%). Seven group C studies [5, 12, 14, 17, 22, 23, 33] revealed this complication in 5% of 455 patients (range: 2-17.3%) (p = 0.07).
Long-term functional results
The three groups did not differ significantly regarding mild/moderate pain or pain in general. In contrast, the incidence of severe pain differed among the groups, with marginal statistical significance (p = 0.06). Group C presented the lowest incidence of severe pain (1% incidence in 308 patients) [3, 11–13, 16, 31, 33, 41], and group A presented the highest (27% in 129 patients) [10, 26, 35]. In group B the median rate of severe pain was 5% in 222 patients [15, 18, 37, 44](Table 5).
Table 5.
Long-term functional outcomes of the reviewed studies based either on validated outcome scores or on the incidence of pain, walking difficulties and return to work
| Group A (non-operative treatment) | Group B (anterior pelvic fixation) | Group C (internal fixation of posterior pelvis) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | No. of studies (pts) | Median value | Range | No. of studies (pts) | Median value | Range | No. of studies (pts) | Median value | Range | p value |
| Incidence of pain | 3 [10, 26, 35] (n = 129) | 63% | 45-73% | 3 [15, 18, 44] (n = 193) | 25% | 10-63% | 9 [3, 11–13, 16, 17, 31, 33, 41] (n = 425) | 34% | 11-85% | 0.18 |
| Incidence of mild/moderate pain | 3 [10, 26, 35] (n = 129) | 37% | 23-38% | 3 [15, 18, 44] (n = 193) | 25% | 5-56% | 8 [3, 11–13, 16, 31, 33, 41] (n = 308) | 34% | 11-73% | 0.88 |
| Incidence of severe pain | 3 [10, 26, 35] (n = 129) | 27% | 7-50% | 4 [15, 18, 37, 44] (n = 222) | 5% | 0-7% | 8 [3, 11–13, 16, 31, 33, 41] (n = 308) | 1% | 0-12% | 0.06 |
| Incidence of undisturbed gait | 3 [10, 26, 35] (n = 129) | 68% | 55-70% | 3 [15, 37, 44] (n = 90) | 84% | 75-91% | 6 [9, 11, 12, 16, 33, 42] (n = 204) | 84.5% | 77-100% | 0.04 |
| Rate of return to previous employment | 2 [10, 26] (n = 76) | 75.5 | 62-89% | 2 [25, 37] (n = 209) | 69.5% | 55-84% | 10 [3, 5, 9, 12–14, 16, 33, 41, 42] (n = 446) | 66% | 45-77% | 0.54 |
| Functional scores | ||||||||||
| Majeed score [20] (% excellent/good results) | 0 | 3 [6, 18, 19] (n = 337) | 51% | 48-100% | 2 [17, 42] (n = 154) | 81.3 | 78.6-84% | 0.77 | ||
| PCS (SF-36) [43] | 0 | 1 [27] (n = 33) | 71.7 | 5 [5, 13, 14, 28, 42] (n = 268) | 64 | 55.5-75.3 | 0.56 | |||
| MCS (SF-36) [43] | 0 | 1 [27] (n = 33) | 75.4 | 5 [5, 13, 14, 28, 42] (n = 268) | 71.1 | 64-74.8 | 0.24 | |||
MCS mental component score (of SF-36), n number, pts patients, PCS physical component score (of SF-36)
The incidence of undisturbed gait was documented in three group A papers (100 patients) [10, 26, 35], three group B papers [15, 37, 44] (90 patients) and six group C papers [9, 11, 12, 16, 33, 42] (204 patients). Groups B and C, with median rates of undisturbed walking capacity at 84 and 84.5%, respectively, differed significantly (p = 0.04) from group A (median value: 68%) (Fig. 5).
Fig. 5.
The incidence of undisturbed gait was evaluated as one of the criteria of long-term functional outcome. A comparison between the two operative groups (B and C) and the non-operative group A showed a statistically significant difference (p = 0.04). In the non-operative group (group A) undisturbed gait was recorded in only 68%, in comparison to 84 and 84.5%, respectively. The grey areas on the chart represent the above rates of undisturbed gait in the three groups
The return to previous employment was analysed in relatively few papers: two in group A [10, 26] (76 patients), two in group B [25, 37] (209 patients) and ten in group C [3, 5, 9, 12–14, 16, 33, 41, 42] (446 patients) with a median incidence of 75.5, 69.5 and 66%, respectively (p = 0.2).
Only 14 studies [5, 6, 9, 12–14, 17–19, 25, 27, 28, 33, 42] assigned to the two groups of operative treatment (B, C) provided data on validated functional scoring systems. The Majeed score [20] and the SF-36 [43] were the most commonly used. Majeed score was documented in three group B [6, 18, 19] and two group C studies [17, 42]. A median value of “excellent/good” results of 51% (range: 48-100%) was recorded in group B and 81.3% (range: 78.6-84%) in group C. The above difference was not statistically significant (p = 0.77), probably due to the small number of available studies.
The two components of SF-36 [physical component score (PCS) and mental component score (MCS)] were analysed separately. PCS was 71.7 and MCS 75.4 in one study of group B [27]. In group C [5, 13, 14, 28, 42] the median PCS was 64 (55.5-75.3) and the median MCS 71.1 (64-74.8). No statistically significant difference of either PCS (p = 0.56) or MCS (p = 0.24) was detected.
Discussion
The aim of this study was to compare the anatomical and functional results, as well as the major complication rates of three different methods of management of pelvic ring disruptions, and subsequently aid clinical decision making.
Most of the relevant reviewed studies received a poor quality score and none of them was graded as excellent (Fig. 2). The main causes for the low quality scores were the study design, lack of blinding, low follow-up rates and lack of active follow-up at pre-specified intervals.
We tried to eliminate systematic error by adhering to clearly defined inclusion and exclusion criteria. We used standard definitions for the outcomes of interest to ensure consistency of the results across all included studies. We tried to avoid random error by including only sizeable reports. Nevertheless, the results of systematic reviews based on observational studies should be interpreted with caution. Such studies differ in design, quality, follow-up process, patients’ demographics, various specific characteristics of the populations studied and outcomes.
We examined 15 characteristics in each treatment group (Table 3), and the statistical differences detected regarded the mean age and the publication year of the reports. As for the mean age, given the fact that the population in all the studies included young adults with a mean age ranging from 26 to 39 years, we do not feel that the detected statistical difference was of any clinical importance. The detected differences in publication year among the three “treatment groups” reflect the evolution of pelvic trauma management, with a gradual shift from conservative to more aggressive rationales.
Three outcomes of interest showed statistically significant differences: the quality of reduction, the gait disturbance and the malunion rates. The best quality of reduction and lowest malunion rates were achieved in the “posterior pelvic internal fixation” group, despite the fact that it included the largest proportion of rotationally and vertically unstable fractures. Several authors have associated anatomical reduction with favourable long-term results. Ragnarsson et al. [33] reported 6 and 25% incidences of severe pain among patients with excellent and satisfactory reductions, respectively. McLaren et al. [24] reported no severe pain in the group of patients with < 1 cm residual pelvic displacement, whereas in the group of poor pelvic reduction it was estimated as to be high as 23%. In the same series, undisturbed gait was documented in 82% of patients with < 1 cm pelvic displacement, and in only 31% of patients with “poor” pelvic reductions. Lindahl et al. [17] also documented a significant association between radiological and functional results. Moreover, permanent neurological injury, female gender and age (< 33 years) were documented as prognostic factors. Other authors [27, 44], however, have failed to establish a clear relationship between quality of pelvic reduction and final functional outcome.
Gait disturbance was found to occur more frequently in the “non-operative group” compared with the others. In one study [24] gait disturbance was associated with a poor anatomical outcome, whereas in another study [2] it was associated with the type of pelvic injury (28% for Tile B and 71% for Tile C).
Although we managed to recruit 27 papers including 1,641 patients with pelvic ring disruptions only a well-designed RCT should be able to detect a true difference with 0.80 probability, accepting a type I error at 0.05. To detect the same difference in the median value of the percentage of poor quality of reduction between group B (19%) and group C (7%) a RCT would require approximately 112 patients in each arm.
In conclusion, our results suggest that fixation of all the injured elements of the pelvic ring yield better anatomical results (expressed as a better quality of reduction and lower malunion rate) compared to more non-operative therapeutic strategies. However, no “clear” advantage of any of the assessed treatment options regarding patient-reported or functional outcomes could be established. We therefore conclude that the current literature is insufficient to provide “clear” evidence for clinical decision making in regards to the optimal treatment of unstable pelvic ring injuries.
References
- 1.Berg EE, Chebuhar C, Bell RM. Pelvic trauma imaging: a blinded comparison of computed tomography and roentgenograms. J Trauma. 1996;41:994–998. doi: 10.1097/00005373-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Broos P, Vanderschot P, Craninx L, Rommens P. The operative treatment of unstable pelvic ring fractures. Int Surg. 1992;77:303–308. [PubMed] [Google Scholar]
- 3.Browner BD, Cole JD, Graham JM, et al. Delayed posterior internal fixation of unstable pelvic fractures. J Trauma. 1987;27:998–1006. doi: 10.1097/00005373-198709000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Bucholz RW. The pathological anatomy of Malgaigne fracture-dislocations of the pelvis. J Bone Joint Surg Am. 1981;63:400–404. [PubMed] [Google Scholar]
- 5.Cole JD, Blum DA, Ansel LJ. Outcome after fixation of unstable posterior pelvic ring injuries. Clin Orthop Relat Res. 1996;329:160–179. doi: 10.1097/00003086-199608000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Dujardin FH, Hossenbaccus M, Duparc F, et al. Long-term functional prognosis of posterior injuries in high-energy pelvic disruption. J Orthop Trauma. 1998;12:145–150. doi: 10.1097/00005131-199803000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Gansslen A, Pohlemann T, Paul C, et al. Epidemiology of pelvic ring injuries. Injury. 1996;27(Suppl 1):S-A13–S-A20. [PubMed] [Google Scholar]
- 8.Goldstein A, Phillips T, Sclafani SJ, et al. Early open reduction and internal fixation of the disrupted pelvic ring. J Trauma. 1986;26:325–333. doi: 10.1097/00005373-198604000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Gruen GS, Leit ME, Gruen RJ, et al. Functional outcome of patients with unstable pelvic ring fractures stabilized with open reduction and internal fixation. J Trauma. 1995;39:838–844. doi: 10.1097/00005373-199511000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Henderson RC. The long-term results of nonoperatively treated major pelvic disruptions. J Orthop Trauma. 1989;3:41–47. doi: 10.1097/00005131-198903010-00008. [DOI] [PubMed] [Google Scholar]
- 11.Hirvensalo E, Lindahl J, Bostman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993;297:28–32. [PubMed] [Google Scholar]
- 12.Kabak S, Halici M, Tuncel M, et al. Functional outcome of open reduction and internal fixation for completely unstable pelvic ring fractures (type C): a report of 40 cases. J Orthop Trauma. 2003;17:555–562. doi: 10.1097/00005131-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Keating JF, Werier J, Blachut P, et al. Early fixation of the vertically unstable pelvis: the role of iliosacral screw fixation of the posterior lesion. J Orthop Trauma. 1999;13:107–113. doi: 10.1097/00005131-199902000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Korovessis P, Baikousis A, Stamatakis M, Katonis P. Medium- and long-term results of open reduction and internal fixation for unstable pelvic ring fractures. Orthopedics. 2000;23:1165–1171. doi: 10.3928/0147-7447-20001101-15. [DOI] [PubMed] [Google Scholar]
- 15.Lansinger O, Karlsson J, Berg U, Mare K. Unstable fractures of the pelvis treated with a trapezoid compression frame. Acta Orthop Scand. 1984;55:325–329. doi: 10.3109/17453678408992366. [DOI] [PubMed] [Google Scholar]
- 16.Leung KS, Chien P, Shen WY, So WS. Operative treatment of unstable pelvic fractures. Injury. 1992;23:31–37. doi: 10.1016/0020-1383(92)90122-9. [DOI] [PubMed] [Google Scholar]
- 17.Lindahl J, Hirvensalo E. Outcome of operatively treated type-C injuries of the pelvic ring. Acta Orthop. 2005;76:667–678. doi: 10.1080/17453670510041754. [DOI] [PubMed] [Google Scholar]
- 18.Lindahl J, Hirvensalo E, Bostman O, Santavirta S. Failure of reduction with an external fixator in the management of injuries of the pelvic ring. Long-term evaluation of 110 patients. J Bone Joint Surg Br. 1999;81:955–962. doi: 10.1302/0301-620X.81B6.8571. [DOI] [PubMed] [Google Scholar]
- 19.Majeed SA. External fixation of the injured pelvis. The functional outcome. J Bone Joint Surg Br. 1990;72:612–614. doi: 10.1302/0301-620X.72B4.2380212. [DOI] [PubMed] [Google Scholar]
- 20.Majeed SA. Grading the outcome of pelvic fractures. J Bone Joint Surg Br. 1989;71:304–306. doi: 10.1302/0301-620X.71B2.2925751. [DOI] [PubMed] [Google Scholar]
- 21.Matewski D, Szymkowiak E, Bilinski P (2007) Analysis of management of patients with multiple injuries of the locomotor system. Int Orthop Jul 3 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 22.Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop Relat Res. 1989;242:83–97. [PubMed] [Google Scholar]
- 23.Matta JM, Tornetta P., 3rd Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res. 1996;329:129–140. doi: 10.1097/00003086-199608000-00016. [DOI] [PubMed] [Google Scholar]
- 24.McLaren AC, Rorabeck CH, Halpenny J. Long-term pain and disability in relation to residual deformity after displaced pelvic ring fractures. Can J Surg. 1990;33:492–494. [PubMed] [Google Scholar]
- 25.Miranda MA, Riemer BL, Butterfield SL, Burke CJ., 3rd Pelvic ring injuries. A long term functional outcome study. Clin Orthop Relat Res. 1996;329:152–159. doi: 10.1097/00003086-199608000-00019. [DOI] [PubMed] [Google Scholar]
- 26.Monahan PR, Taylor RG. Dislocation and fracture-dislocation of the pelvis. Injury. 1975;6:325–333. doi: 10.1016/0020-1383(75)90183-7. [DOI] [PubMed] [Google Scholar]
- 27.Nepola JV, Trenhaile SW, Miranda MA, et al. Vertical shear injuries: is there a relationship between residual displacement and functional outcome? J Trauma. 1999;46:1024–1029. doi: 10.1097/00005373-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Oliver CW, Twaddle B, Agel J, Routt ML., Jr Outcome after pelvic ring fractures: evaluation using the medical outcomes short form SF-36. Injury. 1996;27:635–641. doi: 10.1016/S0020-1383(96)00100-3. [DOI] [PubMed] [Google Scholar]
- 29.Papadopoulos IN, Kanakaris N, Bonovas S, et al. Auditing 655 fatalities with pelvic fractures by autopsy as a basis to evaluate trauma care. J Am Coll Surg. 2006;203:30–43. doi: 10.1016/j.jamcollsurg.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 30.Pennal GF, Tile M, Waddell JP, Garside H. Pelvic disruption: assessment and classification. Clin Orthop Relat Res. 1980;151:12–21. [PubMed] [Google Scholar]
- 31.Pohlemann T, Bosch U, Gansslen A, Tscherne H. The Hannover experience in management of pelvic fractures. Clin Orthop Relat Res. 1994;305:69–80. doi: 10.1097/00003086-199408000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Poole GV, Ward EF, Muakkassa FF, et al. Pelvic fracture from major blunt trauma. Outcome is determined by associated injuries. Ann Surg. 1991;213:532–538. doi: 10.1097/00000658-199106000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ragnarsson B, Olerud C, Olerud S. Anterior square-plate fixation of sacroiliac disruption. 2-8 years follow-up of 23 consecutive cases. Acta Orthop Scand. 1993;64:138–142. doi: 10.3109/17453679308994554. [DOI] [PubMed] [Google Scholar]
- 34.Riska EB, Bonsdorff H, Hakkinen S, et al. External fixation of unstable pelvic fractures. Int Orthop. 1979;3:183–188. doi: 10.1007/BF00265710. [DOI] [PubMed] [Google Scholar]
- 35.Semba RT, Yasukawa K, Gustilo RB. Critical analysis of results of 53 Malgaigne fractures of the pelvis. J Trauma. 1983;23:535–537. doi: 10.1097/00005373-198306000-00016. [DOI] [PubMed] [Google Scholar]
- 36.Simonian PT, Routt ML., Jr Biomechanics of pelvic fixation. Orthop Clin North Am. 1997;28:351–367. doi: 10.1016/S0030-5898(05)70294-7. [DOI] [PubMed] [Google Scholar]
- 37.Slatis P, Karaharju EO. External fixation of unstable pelvic fractures: experiences in 22 patients treated with a trapezoid compression frame. Clin Orthop Relat Res. 1980;151:73–80. [PubMed] [Google Scholar]
- 38.Taguchi T, Kawai S, Kaneko K, Yugue D. Surgical treatment of old pelvic fractures. Int Orthop. 2000;24:28–32. doi: 10.1007/s002640050007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tile M. Classification. In: Tile M, editor. Fractures of the pelvis and acetabulum. Baltimore: Williams and Wilkins; 1995. pp. 66–101. [Google Scholar]
- 40.Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988;70:1–12. doi: 10.1302/0301-620X.70B1.3276697. [DOI] [PubMed] [Google Scholar]
- 41.Tornetta P, 3rd, Matta JM. Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop Relat Res. 1996;329:186–193. doi: 10.1097/00003086-199608000-00022. [DOI] [PubMed] [Google Scholar]
- 42.Bosch EW, Kleyn R, Hogervorst M, Vugt AB. Functional outcome of internal fixation for pelvic ring fractures. J Trauma. 1999;47:365–371. doi: 10.1097/00005373-199908000-00026. [DOI] [PubMed] [Google Scholar]
- 43.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 44.Wild JJ, Hanson GW, Tullos HS. Unstable fractures of the pelvis treated by external fixation. J Bone Joint Surg Am. 1982;64:1010–1020. [PubMed] [Google Scholar]