Abstract
From January 2004 to July 2007, 21 patients with injuries at the posterior pelvic ring were treated with locking compression plate osteosynthesis through a minimally invasive approach and followed up for a mean of 12.2 months. Preoperative and postoperative radiography was conducted to assess the reduction and union. The mean operation time was 60 minutes (range: 40–80). Intraoperative blood loss was 50–150 ml. All patients achieved union at the final follow-up. The overall radiological results were excellent or good in 17 patients (85%). The functional outcome was excellent or good in 18 patients (90%). There was no iatrogenic nerve injury, deep infection or failure of fixation. We believe that fixation with a locking compression plate is an effective method for the treatment of injuries of the posterior pelvic ring in view of its convenience, minimal traumatic invasion and lower morbidity.
Introduction
Unstable pelvic fracture represents a severe injury associated with high mortality and morbidity and remains a therapeutic challenge. Conservative treatment was usually selected in the past due to a lack of understanding of biomechanics and effective therapeutic tools. With the development of fixation techniques, external fixators are widely used in the treatment of pelvic fractures and play an important role in emergency management of anterior ring injuries [2], but the therapeutic outcomes have been unsatisfactory in the case of vertically and rotationally unstable pelvic fractures, especially in patients whose injury was at the posterior pelvic ring [7, 15]. Previous studies [11] have shown the importance of fixation of the posterior structures in unstable pelvic fractures with injury to the posterior pelvic ring. There are several surgical approaches to the treatment of unstable posterior pelvic ring injury: open or percutaneous screw fixation of the sacroiliac joint [17], anterior plate fixation of the sacroiliac joint [20], dorsal plate fixation of sacral fractures [19] and posterior fixation with transiliac sacral bars [3], each having respective advantages and disadvantages.
Previous studies [21, 24] have shown that posterior plate osteosynthesis can provide sufficient stability similar to other methods of treatment for unstable pelvic fractures. In 1993, Albert et al. [1] described a technique of posterior pelvic fixation using a 4.5-mm reconstruction plate as a transiliac tension band. Krappinger et al. [13] reported that transiliac posterior plate osteosynthesis was an optimal method for the treatment of unstable pelvic ring injuries with a low risk of complications. They also used a pelvic reconstruction plate to stabilise the posterior pelvic ring by a minimally invasive approach.
The locking compression plate (LCP) is a new screw plate system that offers the possibility of inserting conventional and locking head screws into the specially designed combination holes and has proven its worth in complex fracture situations [9]. To our knowledge, there has been no report about the treatment of posterior pelvic ring injury with the LCP. We have treated 21 cases of posterior pelvic ring injury with the LCP and the results are satisfactory. The purpose of this article is to describe the surgical technique and report the preliminary radiological and clinical results.
Materials and methods
Patients
A total of 21 patients (16 men and 5 women) ranging in age from 27 to 59 years (mean: 35.6 years) with posterior pelvic ring injuries were admitted and treated with the LCP in the trauma centre of Changhai Hospital (Shanghai, People’s Republic of China) between January 2004 and July 2007. The causes of injury included motor vehicle accidents in eight patients, falls from a height in four patients and crushing injury in the remaining nine patients. Of the 21 cases, 15 were associated with multiple injuries, including associated head injury in three cases, haemopneumothorax in five, abdominal injury in four and additional injury to the extremities in three. The mean Injury Severity Score (ISS) was 29.2 (range: 14–66). According to the AO classification of pelvic injury, there were four cases of type B1, eleven cases of type B2, two cases of type B3 and five cases of type C1 injury. Of the 12 patients with sacral fracture, eight cases were type I and four cases were type II fracture according to the Denis classification of sacral fracture [8]. The function of the lumbosacral plexus was evaluated clinically at the time of admission. Three patients showed signs of a plexus lesion. All surgical procedures were performed within 18 days of injury (2–18, mean: 5 days) and the timing of surgery depended on the general condition of the patients.
Surgical techniques
All of the surgical procedures were performed under general anaesthesia with the patients lying in a semidecubitus position with the injured side bolstered up by 40–50°. Bilateral incisions from the lateral posterior superior iliac spine along the iliac crest were made (6–8 cm long on the affected side and 4–6 cm long on the contralateral side). If both posterior pelvic rings were injured, a 6- to 8-cm incision was made on both sides. The skin and subcutaneous tissue were incised to the periosteum, and soft tissue close to the periosteum was dissected to expose the site of fracture or dislocation. The displacement or dislocation was reduced first: the vertical displacement of the sacroiliac joint was reduced by traction and rotational displacement by compressing the iliac wing (for open-book fracture) or distracting (for closed-book fracture). A 4.5-mm locking compression plate (Synthes® Inc.) of appropriate length (usually 10–12 holes) was used to maintain the reduction. The plate was pre-contoured, but it was not necessary to strictly match with the iliac anatomy. The contoured LCP was placed along the posterior lateral ilium from the affected side to the contralateral side under the fascia. As the fascia was strongly attached to the spinous process of the sacrum, an additional midline incision about 1.5 cm was made to assist insertion of the plate. Three screws were needed for fixation of each ilium and usually one compression screw was first inserted medially, and then two locking head screws were applied. Before and after fixation of the screws, intraoperative fluoroscopy (anteroposterior, inlet and outlet views) was used to assess the reduction and fixation. If the reduction and fixation were successful, the incision was irrigated and sutured. The fascia was sutured first, and then the subcutaneous tissue and skin were closed (Fig. 1). For some cases complicated by unstable anterior pelvic fracture, internal fixation with a reconstruction plate was performed in addition. Usually the posterior injury was treated first, and then the patient was turned over for management of the anterior injury.
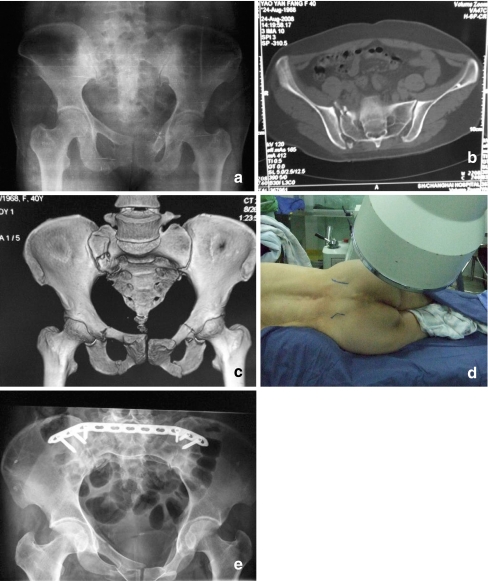
Fig. 1.
A case using the LCP in the treatment of a B2-type pelvic fracture. Preoperative X-ray film (a) and CT scan (b) showing typical closed-book injury of the pelvic ring: compression fracture of the sacral wing and avulsion fracture of the posterior iliosacral ligament. c Three-dimensional CT reconstruction. d The patient lay in a semidecubitus position with the injured side bolstered up by 40–50° during the operation. e Radiograph 2 weeks after surgery
Postoperative rehabilitation and functional exercises
A lateral decubitus or semi-sitting position was allowed postoperatively. The patients were encouraged to take active or passive functional exercises three days after the operation. Crutch-assisted walking was allowed three weeks after the operation. Partial weight-bearing was allowed in a month and full weight-bearing in three months.
Patient evaluation
All of the injured patients received routine X-ray (anteroposterior, inlet and outlet views) and computed tomography (CT) examinations of the pelvis preoperatively. Postoperative radiography (anteroposterior, inlet and outlet views) was conducted to assess the reduction and union within one week postoperatively and at the time of follow-up (one, three, six months, one year and final follow-up). The radiological result of the final follow-up was graded by the maximal residual displacement at the posterior injury of the pelvic ring as: excellent 0–5 mm, good 6–10 mm, fair 11–15 mm and poor more than 15 mm [23].
The functional outcome was measured using a scoring system described by Lindahl et al. [14]. The scoring system was based on clinical findings and focused on the possible handicap caused by the pelvic trauma and neglecting the effect of other injuries.
Results
Of the 21 patients, 20 were followed up for 6–21 months (mean: 12.2 months), and the remaining patient was lost to the follow-up postoperatively (because some patients underwent follow-up at hospitals close to their respective residences and some others did not come to visit doctors any longer when they had recovered from the injury without any discomfort, so far the maximum follow-up actually available in our study was only 21 months). The operation time was 40–80 min (mean: 60 min). Intraoperative blood loss was 50–150 ml, and therefore no blood transfusion was needed in any patient during the operation. No surgical neurovascular injury occurred. All incisions healed primarily well. All patients achieved union at the final follow-up.
The overall radiological result was excellent or good in 17 patients (85%) and moderate or poor in three patients (15%). The functional outcome was excellent or good in 18 patients (90%) and moderate in two patients (10%). The three patients whose preoperative condition was complicated by a lumbosacral plexus injury recovered well three weeks after the operation, though one patient still complained of persistent pain. Loss of reduction was observed in two patients. There was no deep infection, no wound complication or failure of fixation.
Discussion
Posterior pelvic ring injury usually involves the complex structure of the sacroiliac joint and is often associated with other damage. The goal of surgery is to recover stability of the injured pelvic ring and eliminate or prevent further nerve injury. Several surgical methods can be used in the treatment of posterior pelvic ring injury; these are mainly categorised into anterior or posterior approaches. The anterior approach is often used for dislocation of the sacroiliac joint, for which two dynamic compression plates are used, or a 4-hole tetragonal plate is often used to connect the sacral wing and the ilium. As only one screw is allowed to be placed in the sacrum, fixation is neither rigid nor strong. The anterior approach to treat sacroiliac injury demands high surgical skills. In addition, it is not easy to achieve good fixation, intraoperative blood loss is often tremendous and early postoperative weight-bearing is not allowed.
The posterior approach can be used to treat sacral fracture, iliac fracture and sacroiliac dislocation. Surgical methods include: (1) Open fixation with lag screws, which can be used to treat iliac fracture and sacroiliac dislocation. The injured site can be approached directly. The fracture or dislocation is fixed by compression screw. Additionally, posterior injury also can be treated with closed reduction and percutaneous iliosacral screw fixation [12]. However, the iliosacral screws may cause severe complications such as injury to the cauda equina or sacral nerve or blood vessel due to screw malpositioning [5]. Therefore, some researchers have performed the operation under the guidance of somatosensory evoked potential (SEP), electromyelography or electroneurography to reduce the incidence of nerve injury [6]. Nevertheless, nerve injury due to the guide pin, drill bit and screws can not be effectively prevented [16], and doctors are constantly exposed to radiation during the operation. What’s more, extensive anatomical knowledge and surgical skills are needed for this operation. In recent years, CT-based navigation system has been used to place iliosacral screws, making the operation much easier [4], but the equipment is expensive limiting its widespread use. (2) Fixation with transiliac sacral bars: fixation with transiliac sacral bars via the posterior approach is safe, convenient and less invasive [10]. The disadvantages include over-compression of the ilium, which may aggravate displacement of the fragments and cause damage to the sacral nerves. It is not applicable in patients with bilateral sacroiliac joint fracture dislocation or with fracture of the posterior superior iliac spine. Fixation with transiliac sacral bars is suitable for the treatment of sacral fractures at Denis zone I, but for patients with a fracture at Denis zones II or III, sacral nerve injury may be aggravated due to the horizontal compression of the iliac bars. (3) Additionally, a posterior approach with triangular vertebropelvic stabilisation is also available now, but the procedure is complex and more invasive and may even disrupt the lumbosacral joint. Moreover, it cannot be used in patients with poor soft tissues [22].
We believe there is a convenient and safe fixation method for injury to the posterior pelvic ring, especially for patients with bilateral injury to the sacroiliac joint and adjacent ilium fracture or sacral comminuted fracture. We think that the LCP is the preferred choice. Functioning as an internal fixator in a bridging fashion as an extramedullary splint, the LCP provides a new treatment option for many fractures. It has been beneficially used for the treatment of complex fractures in long bones of the extremities.
We advocate the following conditions as indications for LCP fixation as a means of controlling injury to the posterior pelvic ring: (1) injury to the compound bilateral sacroiliac structure, (2) injury or dislocation of the sacroiliac joint associated with sacroiliac ligament injury resulting in instability of the pelvis, (3) fractures at Denis zones II or III resulting in instability of the pelvis and probably leading to subsequent nerve injury, (4) dislocation of the sacroiliac joint associated with sacral or iliac fracture and sacroiliac ligament injury and (5) comminuted sacral fractures.
The LCP is advantageous for the treatment of posterior pelvic ring injury. The structure of the posterior pelvic ring is not only relatively irregular and complex but a crucial weight-bearing part. It is therefore difficult to fix it stably. Based on the special locking mechanism and angular stability design of the LCP that integrates the plate with screws, fixation with the LCP is strong enough even for osteoporotic patients. The LCP can serve as an internal fixator and does not need to be contoured exactly to the anatomy. For fixation of bilateral or severe injuries to the sacroiliac compound structure, the LCP can maintain reduction without compressing the comminuted fragments, thus avoiding nerve injury due to over-compression. It is especially useful for sacral fractures at Denis zones II or III.
Owing to the special locking design of the LCP, a mono-cortex screw can be used. Neurovascular and visceral complications due to cortical penetration from the screws can be avoided. As it is not necessary to insert the screws into the sacrum, nerve injury associated with sacroiliac screw insertion can be avoided. Treatment of posterior pelvic ring injury with the LCP is time saving and less invasive and with few complications.
The disadvantages of the LCP for the treatment of posterior pelvic ring injury include higher cost of the implant plate and contraindiction for posterior pelvic ring injury with transverse sacral fracture and comminuted iliac wing fracture. Some patients may feel uncomfortable due to its presence when lying supine.
Usually, placement of three screws on each side can achieve effective fixation. If the plate is contoured care must be taken not to damage the threads of the screw hole in the plate. If compression is needed, compression screws are placed before insertion of the locking screws. The soft tissue of the outer periosteum should be stripped off from the posterior iliac wing carefully to avoid injury to the superior gluteal nerve and blood vessel. Proportionate traction of the lower extremities is advised preoperatively to help intraoperative reduction.
Nerve injuries associated with posterior pelvic ring injury mainly happen in patients with sacral fractures. Some authors [18] claimed that temporary nerve dysfunction of conduction due to nerve contusion, compression by haematoma and traction injury can recover by conservative treatment in patients with sacral fractures without significant displacement. Zelle et al. [25] asserted that surgical decompression in patients with displaced sacral fracture associated with neurological deficits could achieve better neurological improvement and better functional results. We suggest that it is not necessary to advocate decompression during the operation for simple contusion or compression of nerves. Nerve function can recover automatically after reduction and internal fixation of the fracture. The compressing fragments confirmed by CT examination should be decompressed during the operation.
Because of the wedge shape of the posterior sacrum, the whole structure is strong and stable after reduction and fixation. Moreover, the posterior sacroiliac ligaments can be repaired, which benefits recovery of stability. Therefore, we believe that LCP fixation can ensure stability of the posterior pelvis. Nevertheless, further study and long-term clinical follow-up are needed before a final conclusion can be drawn.
Conclusion
Fixation with the locking compression plate is an effective method for the treatment of injuries of the posterior pelvic ring in view of its convenience, minimal traumatic invasion and lower morbidity.
Footnotes
Tang Hao and Yang Changwei contributed equally to this paper.
Contributor Information
Yang Changwei, Email: changwei_y@qq.com.
Zhang Qiulin, Email: zql@133sh.com.
References
- 1.Albert MJ, Miller ME, MacNaughton M, Hutton WC. Posterior pelvic fixation using a transiliac 4.5-mm reconstruction plate: a clinical and biomechanical study. J Orthop Trauma. 1993;7:226–232. doi: 10.1097/00005131-199306000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Alexa O, Iancu C, Veliceasa B, Puha B, Georgescu N. Results of external fixation in pelvic ring fractures (in Romanian) Rev Med Chir Soc Med Nat Iasi. 2007;111:428–434. [PubMed] [Google Scholar]
- 3.Atlihan D, Bozkurt M, Turanli S, Dogan M, Tekdemir I, Elhan A. Anatomy of the posterior iliac crest as a reference to sacral bar insertion. Clin Orthop Relat Res. 2004;19:141–145. doi: 10.1097/00003086-200401000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Bale RJ, Kovacs P, Dolati B, Hinterleithner C, Rosenberger RE. Stereotactic CT-guided percutaneous stabilization of posterior pelvic ring fractures: a preclinical cadaver study. J Vasc Interv Radiol. 2008;19:1093–1098. doi: 10.1016/j.jvir.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Baumgaertner MR, Wegner D, Booke J. SSEP monitoring during pelvic and acetabular fracture surgery. J Orthop Trauma. 1994;8:127–133. doi: 10.1097/00005131-199404000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Carlson DA, Scheid DK, Maar DC, Baele JR, Kaehr DM. Safe placement of S1 and S2 iliosacral screws: the “vestibule” concept. J Orthop Trauma. 2000;14:264–269. doi: 10.1097/00005131-200005000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Chiu FY, Chuang TY, Lo WH. Treatment of unstable pelvic fractures: use of a transiliac sacral rod for posterior lesions and an external fixator for anterior lesions. J Trauma. 2004;57:141–144. doi: 10.1097/01.TA.0000123040.23231.EB. [DOI] [PubMed] [Google Scholar]
- 8.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67–81. [PubMed] [Google Scholar]
- 9.Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18:488–493. doi: 10.1097/00005131-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Gänsslen A, Pohlemann T, Krettek C. Internal fixation of sacroiliac joint disruption (in German) Oper Orthop Traumatol. 2005;17:281–295. doi: 10.1007/s00064-005-1133-3. [DOI] [PubMed] [Google Scholar]
- 11.Goldstein A, Phillips T, Sclafani SJ, Scalea T, Duncan A, Goldstein J, Panetta T, Shaftan G. Early open reduction and internal fixation of the disrupted pelvic ring. J Trauma. 1986;26:325–333. doi: 10.1097/00005373-198604000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Griffin DR, Starr AJ, Reinert CM, Jones AL, Whitlock S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma. 2006;20:S30–S36. [PubMed] [Google Scholar]
- 13.Krappinger D, Larndorfer R, Struve P, Rosenberger R, Arora R, Blauth M. Minimally invasive transiliac plate osteosynthesis for type C injuries of the pelvic ring: a clinical and radiological follow-up. J Orthop Trauma. 2007;21:595–602. doi: 10.1097/BOT.0b013e318158abcf. [DOI] [PubMed] [Google Scholar]
- 14.Lindahl J, Hirvensalo E. Outcome of operatively treated type-C injuries of the pelvic ring. Acta Orthop. 2005;76:667–678. doi: 10.1080/17453670510041754. [DOI] [PubMed] [Google Scholar]
- 15.Mason WT, Khan SN, James CL, Chesser TJ, Ward AJ. Complications of temporary and definitive external fixation of pelvic ring injuries. Injury. 2005;36:599–604. doi: 10.1016/j.injury.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 16.Moed BR, Ahmad BK, Craig JG, Jacobson GP, Anders MJ. Intraoperative monitoring with stimulus-evoked electromyography during placement of iliosacral screws. An initial clinical study. J Bone Joint Surg Am. 1998;80:537–546. doi: 10.2106/00004623-199804000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Moed BR, Geer BL. S2 iliosacral screw fixation for disruptions of the posterior pelvic ring: a report of 49 cases. J Orthop Trauma. 2006;20:378–383. doi: 10.1097/00005131-200607000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Phelan ST, Jones DA, Bishay M. Conservative management of transverse fractures of the sacrum with neurological features. A report of four cases. J Bone Joint Surg Br. 1991;73:969–971. doi: 10.1302/0301-620X.73B6.1955446. [DOI] [PubMed] [Google Scholar]
- 19.Pohlemann T, Gänsslen A, Tscherne H. Fracture of the sacrum (in German) Unfallchirurg. 2000;103:769–786. doi: 10.1007/s001130050617. [DOI] [PubMed] [Google Scholar]
- 20.Reilly MC, Bono CM, Litkouhi B, Sirkin M, Behrens FF. The effect of sacral fracture malreduction on the safe placement of iliosacral screws. J Orthop Trauma. 2006;20:S37–S43. doi: 10.1097/01.bot.0000199854.47953.2a. [DOI] [PubMed] [Google Scholar]
- 21.Simonain PT, Routt C, Jr, Harrington RM, Tencer AF. Internal fixation for the transforaminal sacral fracture. Clin Orthop Relat Res. 1996;323:202–209. doi: 10.1097/00003086-199602000-00028. [DOI] [PubMed] [Google Scholar]
- 22.Tiemann AH, Schmidt C, Josten C. Triangular vertebropelvine stabilisation of unstable posterior pelvic ring fractures (in German) Zentralbl Chir. 2003;128:202–208. doi: 10.1055/s-2003-38533. [DOI] [PubMed] [Google Scholar]
- 23.Tornetta P, 3rd, Matta JM. Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop Relat Res. 1996;329:186–193. doi: 10.1097/00003086-199608000-00022. [DOI] [PubMed] [Google Scholar]
- 24.Yinger K, Scalise J, Olson SA, Bay BK, Finkemeier CG. Biomechanical comparison of posterior pelvic ring fixation. J Orthop Trauma. 2003;17:481–487. doi: 10.1097/00005131-200308000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Zelle BA, Gruen GS, Hunt T, Speth SR. Sacral fractures with neurological injury: is early decompression beneficial? Int Orthop. 2004;28:244–251. doi: 10.1007/s00264-004-0557-y. [DOI] [PMC free article] [PubMed] [Google Scholar]