Abstract
Measurement of leg length discrepancy is an important part in planning a successful total hip arthroplasty (THA). Many clinical and radiological methods with variable degrees of accuracy have been advocated to carry out this measurement. We studied the accuracy of a commonly used clinical method by comparing it to a well-known and reliable radiological method. A total of 139 patients aged 44–89 (mean: 67.5 years) scheduled to undergo THA were examined for clinical and radiological leg length discrepancy measurements before and after the operation by the same observers. There was a poor correlation between the clinical and radiological methods preoperatively [r = 0.21, intra-class correlation coefficient (ICC) = 0.33]. The correlation was better postoperatively (r = 0.45, ICC = 0.62). The clinical method used is not recommended for leg length discrepancy measurement preoperatively. Caution should even be taken when using this method postoperatively. The authors recommend using the radiological method when measuring leg length discrepancy as a part of planning for THA.
Résumé
Objectif: La mesure de l’inégalité de longueur est une part importante de la planification des prothèses totales de hanche. De nombreuses méthodes cliniques et radiologiques ont été utilisées pour permettre de telles mesures. Nous avons voulu étudier une méthode clinique habituelle comparée à une méthode radiologique fiable. Patients et méthode: 139 patients âgés de 44 à 89 ans (en moyenne 67,5 ans) devant bénéficier d’une prothèse totale de hanche ont été examinés sur le plan clinique et radiologique avec mesure de l’inégalité de longueur avant et après l’intervention chirurgicale par les mêmes observateurs. Résultats: il y a peu de corrélations entre les méthodes cliniques et radiologiques pré-opératoires (r = 0.21, ICC = 0.33). La corrélation est bien meilleure en post-opératoire (r = 0.45, ICC = 0.62). En conclusion, la méthode clinique n’est pas recommandée en pré-opératoire, elle doit être utilisée avec méfiance. En post-opératoire il est recommandé d’utiliser une méthode radiologique afin de mesurer l’inégalité de longueur des membres inférieurs. Celle-ci doit faire partie du planning d’une prothèse totale de hanche.
Introduction
The measurement of leg length discrepancy (LLD) represents an important part of the musculoskeletal physical examination. Numerous clinical and radiological methods for measuring LLD have been described in the literature. Evaluation of degree of precision, validity, intra-observer and inter-observer reliability as well as the degree of correlation among these various methods in groups of patients and healthy subjects has shown variable results with a diverging outcome [5, 8, 9, 11, 15]. The choice of methods varies according to the age of the patient, the condition studied, cost, availability as well as personal preference of the investigator.
In patients considered for total hip arthroplasty (THA), the preoperative and postoperative LLD measurement is commonly carried out clinically and/or radiologically. The clinical measurement can be performed with the patient in the supine position using a tape and calculated as the distance between the anterior superior iliac spine (ASIS) and the medial malleolus. Another way is to measure LLD with the patient in a standing position by placing rigid blocks of varying thickness under the foot of the shorter extremity until the iliac crests appear level. The radiological measurement is made on an anteroposterior (AP) view of the pelvis as the distance between a line passing through the teardrop points medial to the acetabula or through the ischial tuberosities to the tip of the lesser trochanter.
Despite the fact that clinicians are not united about which method is most accurate, the radiological method is often the method of choice when templating for a THA operation.
In this study, we evaluated the correlation between commonly practised clinical and radiological methods for measuring LLD before and after THA.
Material and methods
One hundred and thirty-nine patients with osteoarthritis of the hip were studied during the period September 2002 to March 2005. There were 85 women and 54 men with ages ranging from 44 to 89 (mean: 67.5 years). Two to three weeks before the operation patients were examined by the same physiotherapist as part of the preoperative evaluation visit. The physiotherapist measured LLD with the patient supine. The leg length was calculated by tape measure as the distance between the ASIS and the medial malleolus. The length of the contralateral limb was measured using the same technique. During examination both legs were placed in a neutral position and close to each other to make measurement as standardised as possible. As a part of preoperative evaluation patients were examined with plain radiographs of the pelvis and hip joints. These radiographs were standardised by holding the lower limbs together in a neutral position while taking the pictures. On the AP view of the pelvis the LLD was measured, by the same radiologist for all cases, as the perpendicular distance between a line passing through both teardrop points medial to the acetabula to the corresponding tip of the lesser trochanter (Fig. 1). A positive LLD value was used when the operated limb was longer than the contralateral side while a negative value indicated the opposite.
Fig. 1.
The method used to measure LLD on radiographs. As it is apparent in this figure, pelvic tilt is a common manifestation in these patients and using fixed points on the pelvis (teardrop points) and proximal femur (tip of the lesser trochanter) will minimise the bias encountered in LLD measurements
All operations were via the lateral approach as described by Hardinge [12]. On the third postoperative day, LLD was again measured clinically and radiologically by the same physiotherapist and radiologist using the same method of measurement as preoperatively. The physiotherapist was blinded to the measures achieved by the radiologist and vice versa. In all of the clinical measurements we used a 5-mm precision scale while the radiological measures were achieved with a 1-mm precision scale. Radiographs were calibrated using a radio-opaque ruler to assess the degree of magnification which was taken into consideration when making the measurements.
Statistical analysis To investigate the degree of correlation between the clinical and radiological measurements before and after THA we used Pearson’s correlation and intra-class correlation coefficient (ICC). We measured the degree of difference between the mean values of these measurements with a paired sample test (p < 0.05 was considered as significant).
Ethics This study was approved by the regional Ethics Committee.
Results
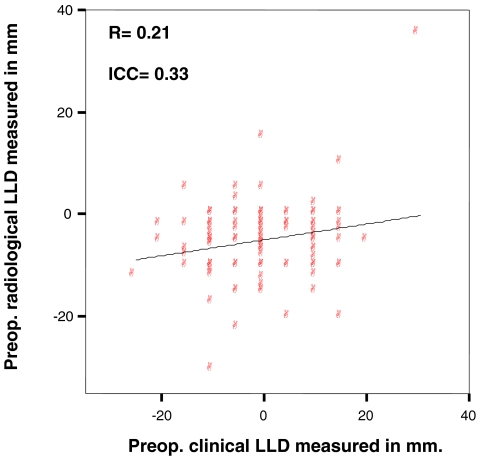
The mean of preoperative clinical LLD measurements was −1 mm (SD = 9 mm) while the mean of preoperative radiological LLD measurements was −5 mm (SD = 7 mm). There was a weak correlation/agreement between these two measurement methods (correlation r = 0.21, ICC = 0.33) (Fig. 2) and the estimated LLD means as evaluated by clinical and radiological methods were significantly different (p < 0.0001).
Fig. 2.
Correlation is weak between preoperative clinical and radiological measurements of LLD
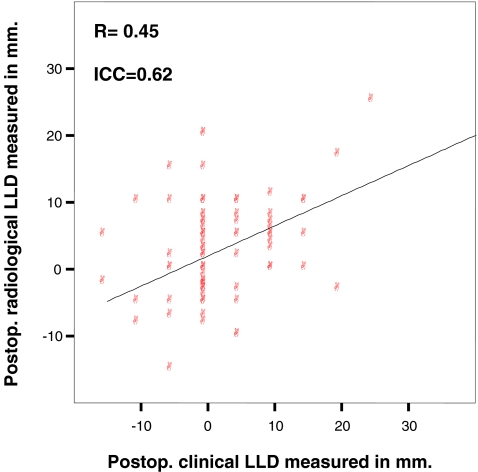
The mean of postoperative clinical LLD measurements was 2 mm (SD = 7 mm) while the mean of postoperative radiological LLD measurements was 3 mm (SD = 7 mm). The correlation/agreement between these measures was better than preoperatively (Fig. 3), but still only fair (r = 0.45, ICC = 0.62). There was no significant difference between the means of the postoperative clinical and radiological measures (p < 0.177).
Fig. 3.
Correlation is fair between postoperative clinical and radiological measurements of LLD
Discussion
Besides relieving the hip and thigh pain, restoration of the hip joint biomechanics with femoral offset and leg length as normal as possible is an important goal of THA. Many techniques to measure these two parameters intraoperatively have been thoroughly discussed in the literature [4, 6, 20].
Leg length discrepancy after THA has been associated with general dissatisfaction [16] as well as other complaints, e.g. gait disorders [17, 21], suspected aseptic loosening [3], greater trochanteric pain [22] and nerve palsy [13]. However, the magnitude of a clinically significant LLD after THA is still a matter of debate and controversy among authors.
Several strategies have been described to assess LLD using different clinical and radiological methods. The degrees of precision and validity of certain methods such as computed tomography (CT) scanogram [1, 2, 14], X-ray scanogram [23] and magnetic resonance imaging (MRI) scanogram [18] are well documented. Unfortunately, the above-mentioned methods cannot be routinely used in THA patients due to the high cost as well as the artefacts encountered with the MRI scanogram because of the presence of a metal in the field of radiation. Instead, it is quite common to use an AP view of a plain radiograph of the pelvis when templating for THA. The measurement of LLD on this view as the distance between a line passing through the lower margin of teardrop points medial to the acetabula to the tip of the lesser trochanter (Fig. 1) was described and used by many authors [16, 19, 20, 24, 25]. This method has been reported to be as reliable as orthoroentgenograms [16]. The inter-observer reliability of this method was tested by Woolson et al. [25] and found to be high (0.5 mm) while the intra-observer reliability was tested by White and Dougall [24] and found to give a measurement error of ± 1 mm. Goodman et al. [10] recommended the use of the teardrop points as a landmark for measurements rather than other points in the pelvis because the vertical position of the teardrop points is not affected significantly by rotation of the pelvis.
Many surgeons even use clinical methods of measuring LLD despite general agreement that radiological measurements are more accurate and reliable than clinical measurements [7, 23]. However, Gogia et al. [9] reported acceptable inter-observer reliability of using clinical LLD measurement (ASIS-medial malleolus). The correlation between this method and a radiological measurement was excellent (ICC = 0.99). Beattie et al. [5] compared LLD measurement using the same clinical method with a radiographic method. They found an ICC value of 0.68. Friberg et al. [8] found that ASIS-medial malleolus measurement differed by ± 8.6 mm from standing radiographic measurement.
The aim of our study was to investigate the degree of accuracy of the clinical method used by comparing it to a well-known and reliable radiological method in patients before and after THA.
One limitation of this study was the difference in the precision degree between the methods investigated (5 mm in the clinical and 1 mm in the radiological). We tried to decrease the effect of this limitation by standardising the method of examination.
We found shortening of the affected limb preoperatively. This is a common finding and is usually secondary to loss of hip joint space with or without cranial migration of the femoral head as well as soft tissue involvement with adduction/abduction and flexion contractures of the affected hip. The weak correlation between the clinical and radiological measurements is probably due to the fact that the radiological measurement was more accurate and easily standardised than clinical examination. The shortening was less apparent clinically than radiologically and this might be due to the painful contracture of the affected hip with a compensating pelvic tilt/obliquity that minimised the apparent shortening. This phenomenon was also described by Ranawat et al. [20]. Postoperatively, and contrary to the preoperative results, there was a lengthening of the operated leg. This is also a common outcome after THA since many surgeons tend to lengthen the operated leg as they try to achieve good stability around the implant. The correlation between the clinical and radiological measurement was better than preoperatively. This could be the result of the THA which minimised soft tissue contracture allowing the patient to lie on the examination table with less pain.
Conclusion
The clinical method of LLD measurement described in this study is not recommended for the evaluation of preoperative LLD in patients considered for THA. In this case a more reliable method such as radiological measurement may be used. Postoperatively, caution should be taken when using the clinical method of LLD measurement despite better correlation with the radiological measurement. In cases were LLD measurement can give rise to further intervention such as revision surgery, the authors recommend the use of a well-documented method with a high degree of precision such as a CT scanogram.
References
- 1.Aaron A, Weinstein D, Thickman D, Eilert R. Comparison of orthoroentgenography and computed tomography in the measurement of limb-length discrepancy. J Bone Joint Surg Am. 1992;74(6):897–902. [PubMed] [Google Scholar]
- 2.Aitken AG, Flodmark O, Newman DE, Kilcoyne RF, Shuman WP, Mark LA. Leg length determination by CT digital radiography. AJR Am J Roentgenol. 1985;144(3):613–615. doi: 10.2214/ajr.144.3.613. [DOI] [PubMed] [Google Scholar]
- 3.Amstutz HC, Ma SM, Jinnah RH, Mai L. Revision of aseptic loose total hip arthroplasties. Clin Orthop Relat Res. 1982;170:21–33. [PubMed] [Google Scholar]
- 4.Bal BS. A technique for comparison of leg lengths during total hip replacement. Am J Orthop. 1996;25(1):61–62. [PubMed] [Google Scholar]
- 5.Beattie P, Isaacson K, Riddle DL, Rothstein JM. Validity of derived measurements of leg-length differences obtained by use of a tape measure. Phys Ther. 1990;70(3):150–157. doi: 10.1093/ptj/70.3.150. [DOI] [PubMed] [Google Scholar]
- 6.Bose WJ. Accurate limb-length equalization during total hip arthroplasty. Orthopedics. 2000;23(5):433–436. [PubMed] [Google Scholar]
- 7.Cleveland RH, Kushner DC, Ogden MC, Herman TE, Kermond W, Correia JA. Determination of leg length discrepancy. A comparison of weight-bearing and supine imaging. Invest Radiol. 1988;23(4):301–304. doi: 10.1097/00004424-198804000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Friberg O, Nurminen M, Korhonen K, Soininen E, Mänttäri T. Accuracy and precision of clinical estimation of leg length inequality and lumbar scoliosis: comparison of clinical and radiological measurements. Int Disabil Stud. 1988;10(2):49–53. doi: 10.3109/09638288809164098. [DOI] [PubMed] [Google Scholar]
- 9.Gogia PP, Braatz JH. Validity and reliability of leg length measurements. J Orthop Sports Phys Ther. 1986;8(4):185–188. doi: 10.2519/jospt.1986.8.4.185. [DOI] [PubMed] [Google Scholar]
- 10.Goodman SB, Adler SJ, Fyhrie DP, Schurman DJ. The acetabular teardrop and its relevance to acetabular migration. Clin Orthop. 1988;236:199–204. [PubMed] [Google Scholar]
- 11.Gross MT, Burns CB, Chapman SW, Hudson CJ, Curtis HS, Lehmann JR, Renner JB. Reliability and validity of rigid lift and pelvic leveling device method in assessing functional leg length inequality. J Orthop Sports Phys Ther. 1998;27(4):285–294. doi: 10.2519/jospt.1998.27.4.285. [DOI] [PubMed] [Google Scholar]
- 12.Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br. 1982;64(1):17–19. doi: 10.1302/0301-620X.64B1.7068713. [DOI] [PubMed] [Google Scholar]
- 13.Hofmann AA, Skrzynski MC. Leg-length inequality and nerve palsy in total hip arthroplasty: a lawyer awaits! Orthopedics. 2000;23(9):943–944. doi: 10.3928/0147-7447-20000901-20. [DOI] [PubMed] [Google Scholar]
- 14.Huurman WW, Jacobsen FS, Anderson JC, Chu WK. Limb-length discrepancy measured with computerized axial tomographic equipment. J Bone Joint Surg Am. 1987;69(5):699–705. [PubMed] [Google Scholar]
- 15.Jonson SR, Gross MT. Intraexaminer reliability, interexaminer reliability, and mean values for nine lower extremity skeletal measures in healthy naval midshipmen. J Orthop Sports Phys Ther. 1997;25:253–263. doi: 10.2519/jospt.1997.25.4.253. [DOI] [PubMed] [Google Scholar]
- 16.Konyves A, Bannister GC. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005;87(2):155–157. doi: 10.1302/0301-620X.87B2.14878. [DOI] [PubMed] [Google Scholar]
- 17.Lai KA, Lin CJ, Jou IM, Su FC. Gait analysis after total hip arthroplasty with leg-length equalization in women with unilateral congenital complete dislocation of the hip–comparison with untreated patients. J Orthop Res. 2001;19(6):1147–1152. doi: 10.1016/S0736-0266(01)00032-8. [DOI] [PubMed] [Google Scholar]
- 18.Leitzes AH, Potter HG, Amaral T, Marx RG, Lyman S, Widmann RF. Reliability and accuracy of MRI scanogram in the evaluation of limb length discrepancy. J Pediatr Orthop. 2005;25(6):747–749. doi: 10.1097/01.bpo.0000173246.12184.a5. [DOI] [PubMed] [Google Scholar]
- 19.Matsuda K, Nakamura S, Matsushita T. A simple method to minimize limb-length discrepancy after hip arthroplasty. Acta Orthop. 2006;77(3):375–379. doi: 10.1080/17453670610046280. [DOI] [PubMed] [Google Scholar]
- 20.Ranawat CS, Rao RR, Rodriguez JA, Bhende HS. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty. 2001;16(6):715–720. doi: 10.1054/arth.2001.24442. [DOI] [PubMed] [Google Scholar]
- 21.Rösler J, Perka C. The effect of anatomical positional relationships on kinetic parameters after total hip replacement. Int Orthop. 2000;24(1):23–27. doi: 10.1007/s002640050006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sayed-Noor AS, Sjödén GO. Greater trochanteric pain after total hip arthroplasty: the incidence, clinical outcome and associated factors. Hip Int. 2006;16:202–206. doi: 10.1177/112070000601600304. [DOI] [PubMed] [Google Scholar]
- 23.Terry MA, Winell JJ, Green DW, Schneider R, Peterson M, Marx RG, Widmann RF. Measurement variance in limb length discrepancy: clinical and radiographic assessment of interobserver and intraobserver variability. J Pediatr Orthop. 2005;25(2):197–201. doi: 10.1097/01.bpo.0000148496.97556.9f. [DOI] [PubMed] [Google Scholar]
- 24.White TO, Dougall TW. Arthroplasty of the hip. Leg length is not important. J Bone Joint Surg Br. 2002;84:335–338. doi: 10.1302/0301-620X.84B3.12460. [DOI] [PubMed] [Google Scholar]
- 25.Woolson ST, Hartford JM, Sawyer A. Results of a method of leg-length equalization for patients undergoing primary total hip replacement. J Arthroplasty. 1999;14:159–164. doi: 10.1016/S0883-5403(99)90119-5. [DOI] [PubMed] [Google Scholar]