Abstract
This article presents a simple technique for fascia lata lengthening that is less aggressive, can be performed under local anaesthetic with little morbidity and disability, and has excellent results. Eleven patients (13 hips) were enrolled in this study. Mean age was 54.6 years, there was one man and ten women. Outcomes were assessed by using a visual analog pain scale, Harris hip score and Lickert scale (satisfaction). There was a mean follow-up time of 43 months (range 15–84). All patients were scored by the Harris hip scale with a mean improvement from 61 (range 48–77) to 91 (range 76–95) after surgery. The mean visual analogue scale (VAS) score improved from 83 (range 60–99) to 13 (range 0–70). We had 12 of 13 patients reporting a good result. Mean surgical time was 15 min, and only one seroma was reported as a complication. No inpatient management was needed. In conclusion, distal “Z” lengthening of the fascia lata appears to be a good alternative for treatment of this condition.
Résumé
L'allongement du fascia lata distal: une alternative chirurgicale pour le traitement des bursites trochantériennes résistantes au traitement médical. Nous présentons une technique simple, peu agressive qui peut être réalisée sous anesthésie locale avec une morbidité faible et d'excellents résultats. Méthodes: 11 patients (13 hanches) ont été inclus dans cette étude. L'âge moyen était de 54.6 ans, il s'agissait d'un homme et de 10 femmes. Le devenir de ces patients a été évalué à l'aide de l'échelle visuelle analogique des douleurs et du score de Harris et de l'échelle de Licker (satisfaction des patients). Le suivi moyen a été de 43 mois (de 15 à 84). Résultats: tous les patients évalués par l'intermédiaire du score de Harris ont été améliorés de 61 (48 à 77) à 91 (76 à 95) après chirurgie. L'échelle visuelle analogique a également permis de montrer une amélioration des phénomènes douloureux passant de 83 à 13 (60–99 à 0–70). 12 patients sur 13 pensent avoir un très bon résultat. En moyenne, la chirurgie a duré 15 minutes avec seulement un écoulement séreux. Il n'y a pas eu nécessité d'hospitaliser à temps plein ces patients. Conclusion, l'allongement en Z du fascia lata distal apparaît comme une bonne alternative pour le traitement de cette pathologie.
Introduction
Trochanteric bursitis suggests inflammation in one or more of the peritrochanteric bursae; however, there are many anatomical structures beneath this area including muscles, tendons and entheses that can contribute to this condition [1]. Thus, it might be more correct to refer to a greater trochanteric pain syndrome (GTPS) to include all these sources of pain.
The localised inflammation of one or more of these bursae is the most common pathophysiological mechanism leading to this syndrome [2].
Trochanteric bursitis is a common entity encountered by the orthopaedic surgeon and other practitioners [3–5]. Approximately 10–20% of patients have been reported to attend to the primary care practitioner with hip problems [6].
The chief complaint is pain in the region of the greater trochanter at the lateral aspect of the hip joint with pain radiating down the lateral thigh, anterior thigh, or buttocks [5]. In up to 25–40% of cases [7] this can mimic major hip disease, low back pain and nerve root pressure syndrome [8, 9]; this is due to the anatomical overlap of the dermatomes corresponding to the iliotibial tract and the lumbar region [2].
Trauma is also a well known aetiology, whereby 23–64% of patients recall a specific traumatic event. This entity is more often associated with repetitive microtrauma, which is an alteration in the biomechanics of the lower extremity and other factors [7, 10]. Calcification related to a degenerative process and may present in up to 20% of cases [3].
The diagnosis is clinical. Examination for this condition is best done by the Little [10] method. Lumbar pathology, hip conditions, as well as local processes such as soft tissue infection and bone or soft tissue tumours [1] must be excluded. X-ray films, sonography or MRI may be necessary to make the differential diagnosis [7, 9].
Previously reported cases, especially those associated with calcification, have been surgically treated with excision of the bursa and calcifications [7]. Present management consists of a conservative approach that includes: NSAIDs, physiotherapy, bed rest, correction of the suspected although still unproven predisposing factors, and glucocorticoid injections [1, 4, 7, 11]. Surgical procedures such as open supratrochanteric fasciotomy or endoscopic bursectomy have been used successfully in patients failing conservative treatment [1].
Our technique is based on the reduction of friction between the iliotibial band and the trochanter by distal lengthening. In addition, because the proximal area over the trochanter is not disturbed, fibrosis is reduced and the likelihood of recurrence is diminished [12]. This article presents a different outpatient procedure and a very low complications rate.
Materials and methods
Between October 1999 and February 2006 we treated 11 patients with chronic trochanteric bursitis (13 hips). There was one man and ten women (12 hips). All operations were performed by a single team of surgeons at our hospital. The mean age of the patients at the time of surgery was 54.6 years (range 32–74). The mean BMI was 26.3 (range 21–35). The right hip was most commonly affected with a 61.5% prevalence, and the mean evolution time before surgery was 22 months (range 12–60).
All patients had localised pain and tenderness in the greater trochanter region and achieved partial relief after a glucocorticoid injection. All had full range of motion of the affected hip. Complaints of limitation for usual activities were common. All patients had undergone conservative management for at least one year with NSAIDs, physiotherapy and glucocorticoid injections (with a mean of four injections per patient). There was no previous history of traumatic event. Radiographs of the pelvis and hip showed four patients with calcification without any previous surgery.
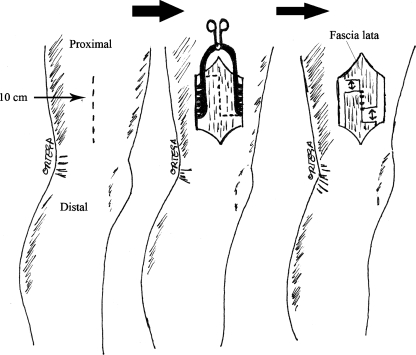
For the operative technique, patients are placed in a lateral position and a longitudinal incision over the distal fascia lata is made (Fig. 1); local anaesthesia is previously administered in all patients. A squared area of the skin must be infiltrated, while the subcutaneous tissue has very few nociceptive receptors and does not need to be infiltrated. Electrocautery is used if needed. Dissection in layers is continued to the fascia lata where a “Z” lengthening is performed. A section of the fascial layer may be a bit uncomfortable for the patient for a few seconds but this is not usually a concern for the procedure. We observe the sliding of the two ends of the “Z”. The fascia is sutured in its new elongated position with reabsorbable sutures. The wound is closed in layers, and an subcuticular skin suture is usually employed. No drain was used.
Fig. 1.
Surgical area where the distal lengthening is made. A squared area of skin is infiltrated with local anaesthesia. Dissection by layers is made until the fascia lata is seen and a “Z” type incision is made observing it’s sliding. The fascia is sutured with reabsorbable sutures
Patients are managed as outpatients and are allowed to bear weight on the first day using a crutch depending on pain.
The outcome is assessed using the Harris hip score, visual analogue scale (VAS), Lickert scale (satisfaction) and surgical duration. Postsurgical complications were recorded.
Results
The mean follow-up was 43 months (range 15–84). All patients were scored according to the Harris hip scale. The mean score improved from 61 (range 48–77) to 91 (range 76–95) after surgery (Table 1).
Table 1.
Details of the 11 patients (13 hips) who underwent distal fascia lata “Z” lengthening as a treatment for refractory trochanteric bursitis (Harris hip score)
| Patients (hips) | Pre-surgery | Post-surgery | Time for resolution of symptoms (mo) | Follow-up period (mo) |
|---|---|---|---|---|
| 1 | 77 | 94 | 4 | 72 |
| 2 | 69 | 91 | 7 | 29 |
| 3 | 63 | 86 | 4 | 35 |
| 4 | 64 | 94 | 2 | 15 |
| 5 | 60 | 94 | 2 | 35 |
| 6 | 69 | 95 | 5 | 72 |
| 7 | 48 | 94 | 4 | 16 |
| 8 | 54 | 95 | 3 | 28 |
| 9a | 50 | 76 | 24 | 36 |
| 10 | 49 | 95 | 2 | 18 |
| 11 | 63 | 82 | 5 | 84 |
| 12 | 69 | 91 | 2 | 62 |
| 13 | 64 | 94 | 2 | 60 |
aProximal “Z” lengthening
The range of motion was normal prior to surgery in all patients. We also used the VAS score to assess pain (range 0–100); the mean score improved from 83 (60–99) to 13 (0–70) (see Table 2).
Table 2.
Details of the 11 patients (13 hips) who underwent distal fascia lata “Z” lengthening as a treatment for refractory trochanteric bursitis (visual analog scale)
| Patients (hips) | Pre-surgery | Post-surgery | Resolution of symptoms (mo) | Follow-up (mo) |
|---|---|---|---|---|
| 1 | 90 | 15 | 4 | 72 |
| 2 | 80 | 10 | 7 | 29 |
| 3 | 70 | 0 | 4 | 35 |
| 4 | 90 | 15 | 2 | 15 |
| 5 | 95 | 10 | 2 | 35 |
| 6 | 75 | 0 | 5 | 72 |
| 7 | 95 | 10 | 4 | 16 |
| 8 | 90 | 0 | 3 | 28 |
| 9a | 99 | 70 | 24 | 36 |
| 10 | 95 | 0 | 2 | 18 |
| 11 | 60 | 20 | 5 | 84 |
| 12 | 70 | 10 | 2 | 62 |
| 13 | 70 | 10 | 2 | 60 |
aProximal “Z” lengthening
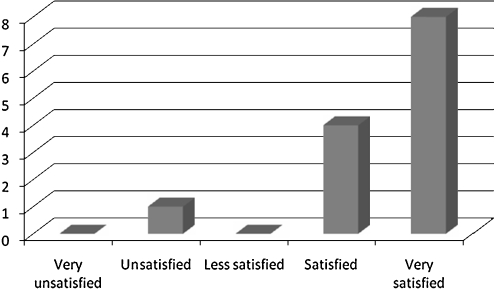
A Lickert scale was used to assess the level of satisfaction; globally there was a good outcome. Twelve of 13 patients reported a good result (including “satisfied” and “very satisfied” patients), and one of 13 reported an unsatisfactory outcome (Fig. 2).
Fig. 2.
Bar chart showing the postoperative Lickert scale of satisfaction
One patient (a female) did not achieve good results in the Harris hip score and VAS; after the distal “Z” lengthening she was treated with glucocorticoid injections (twice) and physiotherapy, with partial relief. Thus, a proximal “Z” lengthening was made with good results. Her Harris score rose from 76 to 94, her VAS decreased from 70 to 20, and she reported a 4 (satisfied) in the Lickert scale
The mean surgical duration of the procedure was 15 min. One case of seroma was reported as a complication, which was surgically drained with good result.
The mean time for resolution of symptoms was five months (range 2–24), including the patient with the additional proximal “Z” lengthening; excluding her the mean time was 3.5 months (range 2–7) (Tables 1 and 2). No recurrences were seen.
Discussion
Trochanteric bursitis is a common clinical entity that can result in severe disabling hip pain [13]. It develops from of repetitive friction between the iliotibial band and the greater trochanter [12]. The conservative approach can achieve success rates exceeding 90%, but for those who do not respond there are many operative procedures.
These procedures can be proximal approaches to the iliotibial band through an open or endoscopic technique. To our knowledge there are no distal approaches to the iliotibial band described for this pathology; our technique is based on the concept that releasing tension of the fascia lata could diminish its friction over the greater trochanter [14].
In 1979, Brooker [3] reported the first true surgical series for refractory trochanteric bursitis. Five patients, all women with severe limiting pain, underwent an excision of the gluteus maximus bursae, debridement and release of the iliotibial band with a simple fenestration or a “T” shaped incision; all patients were satisfied and their Harris hip scores, which improved from 46 before to 88 after the surgical procedure. It is not clearly explained why two different procedures were used in the same series.
Zoltan et al. [15] reported a new procedure based on an excision of an ellipsoid-shaped portion of the iliotibial band overlying the greater trochanter and removal of the bursa. Seven patients with painful hip due to snapping of the iliotibial band were included, and five were evaluated at the time of the report. Four significantly improved, while the fifth underwent an additional procedure and was asymptomatic one year later. But in this study there was no standardised hip score and the snapping hip shouldn’t be confused with trochanteric bursitis, because not all snapping hips will develop a trochanteric bursitis. In our study these patients were excluded, but we think that theoretically this technique could be use in those cases where excessive tightness of the fascia lata is observed [14].
Slawski et al. [5] reported on seven hips in five patients who underwent a simple longitudinal release of the iliotibial band over the greater trochanter and excision of the subgluteal bursa, with a mean follow-up of 20 months. The mean Harris hip score improved from 51.7 before to 95 after surgery; all were satisfied.
In 2003, Govaert et al. [12] described a technique for patients with chronic trochanteric bursitis involving a trochanteric reduction osteotomy in ten patients (12 hips). The mean follow-up was 23.5 months, and a mean improvement of the Merle d´Aubigné and Postel score from 15.8 to 27.5 after surgery was achieved. They had a low complication rate. They concluded that it was a safe and effective procedure.
In recent years arthroscopic techniques have advanced. Fox et al. [13] presented an arthroscopic bursectomy in 27 patients. They had good or excellent results in 23 of 27 patients. At one year, one had experienced recurrence and two had recurred at five years. All except one were satisfied with the outcome. It seems to be a minimally invasive technique, which is safe and effective.
Wiese et al. [16] also performed endoscopic bursectomies. He reported 45 bursectomies in 42 patients; bursae were removed using a synovial resector. Thirty-seven patients were followed for 12–48 months. The mean Japanese Orthopedic Association (JOA) disability hip score improved from 40.5 before to 72.6 after surgery with a mean follow-up of 25 months. No complications were reported. This technique requires only stab incisions and immobilisation and hospital stay are minimal.
Baker et al. [17] presented a prospective study with endoscopic bursectomy. Thirty patients were enrolled, among these, twenty-five were available for a mean follow-up of 26.1 months. The mean Harris hip score improved from 51 before to 77 after surgery (p = 0.0001), and the VAS improved from 7.2 to 3.1 (p = 0.0001). Only one seroma was observed. Improvement in patient status was usually evident by one to three months after surgery and appeared to last over time.
In 2007, Craig et al. [18] reported a proximal “Z” lengthening of the iliotibial band that leaves a 5 cm defect over the posterior aspect of the greater trochanter. Fifteen patients (17 hips) were enrolled with a mean follow-up of 47 months. Eight patients reported excellent results with complete resolution of symptoms; there were eight good results and one poor result. The mean Harris hip score improved from 46 to 82.
The characteristics of the patients in our study are very similar to the ones reported in the literature. The mean follow-up is also similar. The parameters of outcome used in the majority of papers are the Harris hip score and VAS score, which were also used in our study. All of our patients had experienced no significative improvement after a previous long and intensive period of conservative treatment. After the procedure described in this article almost all patients achieved a significant improvement in Harris hip score and VAS score similar to other studies. Almost all patients referred a high degree of satisfaction after the procedure. We consider that the advantages of our technique are the minimal surgical aggression, the brevity of the procedure (mean of 15 min), the low morbility (one seroma), the low disability (the patient leaves the hospital in the afternoon by his own means), that no hospital admission is required, and that few materials are needed.
Although the conservative management of trochanteric bursitis achieves excellent results, distal “Z” lengthening of the fascia lata appears to be a good alternative for the management of recalcitrant trochanteric bursitis.
References
- 1.Alvarez-Nemegyei J, Canoso JJ. Evidence-based soft tissue rheumatology III: trochanteric bursitis. J Clin Rheumatol. 2004;10(3):123–124. doi: 10.1097/01.rhu.0000129089.57719.16. [DOI] [PubMed] [Google Scholar]
- 2.Justin P, Carbone J, Quartararo L. Greater trochanteric pain syndrome in patients referred to orthopedic spine specialists. Spine J. 2002;2(4):251–254. doi: 10.1016/S1529-9430(02)00198-5. [DOI] [PubMed] [Google Scholar]
- 3.Brooker A. The surgical approach to refractory trochanteric bursitis. The Johns Hopkins Med J. 1979;145(3):98–100. [PubMed] [Google Scholar]
- 4.Farr D, Selesnick H, Janecki C, Cordas D. Arthroscopic bursectomy with concomitant iliotibial band release for the treatment of recalcitrant trochanteric bursitis. Arthroscopy. 2007;23(8):905. doi: 10.1016/j.arthro.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 5.Slawski DP, Howard RF. Surgical management of refractory trochanteric bursitis. Am J Sports Med. 1997;25(1):86–89. doi: 10.1177/036354659702500117. [DOI] [PubMed] [Google Scholar]
- 6.Lievense A, Bierma-Zeinstra S, Schouten B, Bohnen A, Verhaar J, Koes B. Prognosis of trochanteric pain in primary care. Br J Gen Pract. 2005;55(512):199–204. [PMC free article] [PubMed] [Google Scholar]
- 7.Shbeeb MI, Matteson EL. Trochanteric bursitis (greater trochanter pain syndrome) Mayo Clin Pro. 1996;71(6):565–569. doi: 10.4065/71.6.565. [DOI] [PubMed] [Google Scholar]
- 8.Sayegh F, Potoupnis M, Kapetanos G. Greater trochanter bursitis pain syndrome in females with chronic low back pain and sciatica. Acta Orthop Belg. 2004;70(5):423–428. [PubMed] [Google Scholar]
- 9.Walsh G, Archibald CG. MRI in greater trochanter pain syndrome. Australas Radiol. 2003;47(1):85–87. doi: 10.1046/j.1440-1673.2003.01113.x. [DOI] [PubMed] [Google Scholar]
- 10.Cohen SP, Narvaez JC, Lebovits AH, Stojanovic MP. Corticosteroid injections for trochanteric bursitis: is fluoroscopy necessary? A pilot study. Br J Anaesth. 2005;94(1):100–106. doi: 10.1093/bja/aei012. [DOI] [PubMed] [Google Scholar]
- 11.Little H. Trochanteric bursitis: a common cause of pelvic girdle pain. Can Med Assoc J. 1979;120(4):456–458. [PMC free article] [PubMed] [Google Scholar]
- 12.Govaert LH, Vis HM, Marti RK, Albers GH. Trochanteric reduction osteotomy as a treatment for refractory trochanteric bursitis. J Bone Joint Surg Br. 2003;85(2):199–203. doi: 10.1302/0301-620X.85B2.13474. [DOI] [PubMed] [Google Scholar]
- 13.Fox JL. The role of arthroscopic bursectomy in the treatment of trochanteric bursitis. Arthroscopy. 2002;18(7):E34. doi: 10.1053/jars.2002.35143. [DOI] [PubMed] [Google Scholar]
- 14.Pecina M, Bojanic I, Haspl M. The snapping hip. Hip Int. 1994;4(3/4):133–136. [Google Scholar]
- 15.Zoltan DJ, Clancy WG, Jr, Keene JS. A new operative approach to snapping hip and refractory trochanteric bursitis in athletes. Am J Sports Med. 1986;14(3):201–204. doi: 10.1177/036354658601400304. [DOI] [PubMed] [Google Scholar]
- 16.Wiese M, Rubenthaler F, Willburger RE, Fennes S, Haaker R. Early results of endoscopic trochanter bursectomy. Int Orthop. 2004;28(4):218–221. doi: 10.1007/s00264-004-0569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baker CL, Jr, Massie RV, Hurt WG, Savory CG. Arthroscopic bursectomy for recalcitrant trochanteric bursitis. Arthroscopy. 2007;23(8):827–832. doi: 10.1016/j.arthro.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 18.Craig RA, Jones DP, Oakley AP, Dunbar JD. Iliotibial band Z-lengthening for refractory trochanteric bursitis (greater trochanteric pain syndrome) ANZ J Surg. 2007;77(11):996–998. doi: 10.1111/j.1445-2197.2007.04298.x. [DOI] [PubMed] [Google Scholar]