Abstract
A review of prospectively collected data in our trauma unit for the years 1998–2003 was undertaken. Adult patients who suffered multiple trauma with an Injury Severity Score (ISS) of ≥16, admitted to hospital for more than 72 hours and with sustained blunt chest injuries were included in the study. Demographic details including pre-hospital care, trauma history, admission vital signs, blood transfusions, details of injuries and their abbreviated injury scores (AIS), operations, length of intensive care unit and hospital stays, Injury Severity Score (ISS) and mortality were analysed. Fulfilling the inclusion criteria with at least one chest injury were 1,164 patients. The overall mortality reached 18.7%. As expected, patients in the higher AIS groups had both a higher overall ISS and mortality rate with one significant exception; patients with minor chest injuries (AISchest = 1) were associated with mortality comparable to injuries involving an AISchest = 3. Additionally, the vast majority of polytraumatised patients with an AISchest = 1 died in ICU sooner than patients of groups 2–5.
Résumé
Nous avons pratiqué une revue prospective des données de notre unité de traumatologie pour l'année 1998 à 2003. Les patients présentant des polytraumatismes sévères et dont le score ISS était de 16, admis à l'hôpital pour plus de 72 heures et présentant des traumatismes thoraciques ont été inclus dans cette étude. Les détails démographiques, les traitements pratiqués, l'histoire du traumatisme, les signes vitaux, les lésions vitales à l'admission, les transfusions sanguines, le détail des traumatismes selon le score AIS, les traitements en unité de soins intensifs ainsi que la durée de séjour, le score de sévérité des traumatismes et la mortalité ont été analysés. 1 164 patients présentant au moins un traumatisme thoracique ont été inclus. Le taux de mortalité a été de 18,7%. Les patients avec un score AIS élevé, associés à un score ISS élevé avaient un taux de mortalité significatif avec une exception significative pour les patients présentant un traumatisme thoracique minime (AIS thoracique = 1) associés à une mortalité comparable aux traumatismes de score AIS = 3. De plus, la grande majorité des patients polytraumatisés avec un score AIS = 1 sont décédés en unité de soins intensifs de façon plus précoce que les patients des groupes 2 à 5.
Introduction
Blunt chest injuries can potentially pose a threat to the airway, breathing and circulation in the traumatised patient, thus directly affecting the clinical course and outcome [9]. In the United States and Europe, the mortality rate in patients with blunt chest trauma can be as high as 60% [9]. Moreover, 20–25% of deaths in polytrauma patients are attributed to chest injury [9]. These numbers justify the presence of extensive literature related to chest injuries where the difference in epidemiology and clinical outcomes between adults and children has been well documented [23] as well as the effects between patients with flail chest vs. pulmonary contusion [9]. Authors have also effectively analysed the impact of age, rib fractures [4], pulmonary contusion [13], pelvic fractures [11], intramedullary nailing [5] and the role of analgesia [7].
Despite extensive reports relevant to blunt chest trauma in the literature, systematic quantification of the impact of chest injury severity on the outcome of polytraumatised patients has been sparse. Recent evidence has indicated that polytraumatised patients with blunt chest trauma present significant differences in mortality and morbidity among different healthcare systems [12]. This necessitates further analysis of blunt chest trauma and auditing of the factors and treatment strategies that could improve outcome.
The purpose of this study therefore was to investigate the incidence and outcome of chest injuries after blunt trauma in polytrauma patients admitted to a level I trauma centre over a six-year period.
Patients and methods
A review of prospectively collected data in our trauma unit for the years January 1998 through January 2003 was undertaken. This collection of data forms part of the trauma audit and research networks (TARN) ongoing study into the epidemiology of trauma in the United Kingdom. TARN includes data from 50% (n = 121) of all hospitals receiving trauma patients in England and Wales.
For this study, inclusion criteria included adult patients (older than 16 years) who suffered multiple trauma with an Injury Severity Score (ISS) [3] of ≥16, admitted to hospital for more than 72 hours and having sustained chest injuries. Isolated injuries to the head and/or to the abdomen, patients with burns or inhalation injuries as well as patients transferred to other units within 48 hours of admission were excluded.
Data collected included demographic details, pre-hospital care, trauma history, admission vital signs, fluid and blood product resuscitation requirements, details of injuries and their severity scores (Abbreviated Injury Score, AIS) [1], operations, length of intensive care unit and hospital stays, the overall Injury Severity Score (ISS) [3] and mortality.
The SPSS v. 11, (SPSS Inc., Chicago, IL, USA) software was used for statistical analysis (Chicago, IL). Parametric and non-parametric tests were used as appropriate to assess continuous variables for significant differences between groups. The Students t-test and Mann-Whitney U tests were employed. Dichotomous variables were assessed using a chi-squared test. For all outcomes statistical significance was assumed at the p < 0.05 level.
Results
Over the six-year period, out of 25,467 trauma patients admitted in our institution there were 1,164 (4.57%) patients with at least one chest injury who fulfilled the inclusion criteria of this study, of which 838 were male and 326 female. The mean age was 40.8 years (median 37, range 16–100; Table 1).
Table 1.
Summary of the patients' demographics and the main findings of this study
| Chest AIS 1 | Chest AIS 2 | Chest AIS 3 | Chest AIS 4 | Chest AIS 5 | Chest AIS 6 | TOTAL | |
|---|---|---|---|---|---|---|---|
| Number of patients | 51 | 234 | 492 | 261 | 121 | 5 | 1,164 |
| Gender (M/F) | 38/13 | 133/101 | 370/122 | 188/73 | 105/16 | 4/1 | 838/326 |
| Age (y) | 43.3 | 47.3 | 37.8 | 42.1 | 37.5 | 21.6 | 40.8 |
| ISS (mean ± SD) | 15.7 ± 8.8 | 11.3 ± 8.3 | 21 ± 11.7 | 30.4 ± 13 | 39.3 ± 11.8 | 75 ± 0 | 26.7 |
| Admission pulse | 86 | 89.7 | 94.7 | 88.7 | 88.1 | 24 | |
| Admission blood pressure | 134.3 | 137 | 128.1 | 116.4 | 102.9 | 20 | |
| Admission GCS | 10.8 | 13.6 | 10.9 | 9.9 | 9.2 | 4.4 | |
| Blood transfused in A&E | 0.45 | 0.1 | 0.36 | 1 | 1.75 | 2.6 | |
| No. receiving transfusion (%) | 6 (11.8) | 12 (5.1) | 50 (10.2) | 56 (21.5) | 35 (30) | 3 (60) | |
| Mean no. of chest injuries | 1.04 | 1.17 | 1.4 | 1.93 | 2.6 | 3.2 | 1.6 |
| No. with head injury (%) | 26 (50.1) | 44 (18.8) | 171 (34.8) | 102 (39.1) | 51 (42.1) | 2 (40) | 397 (34.1) |
| Head AIS (mean) | 3.6 | 3.7 | 3.8 | 3.8 | 3.4 | 4 | 3.7 |
| No. with extremity injury (%) | 37 (72) | 109 (46.6) | 236 (48) | 164 (62.8) | 71 (58.7) | 4 (80) | 621 (53.4) |
| Extremity AIS (mean) | 2.7 | 2.5 | 2.7 | 2.7 | 2.8 | 2.8 | 2.7 |
| No. with ABDO injury (%) | 12 (23.5) | 49 (20.9) | 119 (45.6) | 83 (31) | 55 (45) | 3 (60) | 321 (27.6) |
| ABDO AIS (mean) | 2.4 | 2.4 | 2.9 | 3 | 3 | 2.3 | 2.8 |
| ARDS | 0 | 3 (2) | 6 (3) | 10 (4) | 3 (1) | 0 | 22 (10) |
| Pneumonia | 0 | 4 | 6 | 4 | 5 | 0 | 19 |
| MOF | 0 | 0 | 1 | 3 | 1 | 0 | 5 |
| Renal failure | 0 | 2 | 5 | 4 | 2 | 0 | 13 |
| Operations on chest injury | 0 | 10 | 32 | 28 | 39 | 2 | 111 |
| % taken to theatre from A&E | N/A | 0 | 28.1 | 39.3 | 43.6 | 100 | |
| Mortality in the operated patients | N/A | 0 | 3.1 | 17.9 | 38.5 | 100 | 20.7 |
| Mortality in those operated as an emergency | N/A | 0 | 11.11 | 45.5 | 47.1 | 100 | |
| No. admitted to ICU | 13 | 43 | 211 | 115 | 55 | 0 | 437 |
| % admitted to ICU | 25 | 18 | 42.9 | 44 | 45.5 | 0 | 37.5 |
| Mean ICU stay | 4.5 | 4 | 5.3 | 6.3 | 6.1 | 0 | 5.5 |
| Hospital stay | 12.6 | 14.6 | 19.9 | 17.1 | 16.7 | 0 | 17.5 |
| No. deaths | 8 | 12 | 74 | 76 | 43 | 5 | 218 |
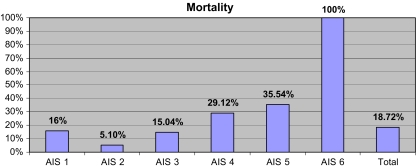
| % mortality | 16% | 5.10% | 15.04% | 29.12% | 35.54% | 100% | 18.72% |
| Timing of deaths (days) | 2.5 | 10.25 | 8.7 | 5.2 | 4.4 | 1 | |
| No. (%) admitted to ICU | 6 (75) | 3 (25) | 42 ( 56.8) | 33 (43.4) | 15 (34.9) | 0 (0) | 99 |
| Length of ICU stay | 3.2 | 3 | 4.7 | 5.4 | 3.5 | 0 |
GCS Glasgow Coma Score, A&E Accident and Emergency, ABDO abdominal, AIS Abbreviated Injury Severity, MOF multi-organ failure, ICU intensive care unit, N/A not applicable
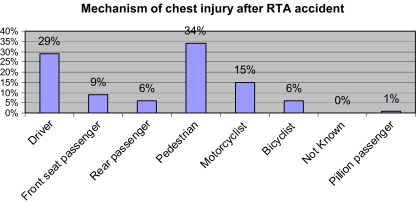
Mechanism of injury
Road traffic accidents (RTA) were overall the most common mechanism of injury accounting for 57.01% of the patients. Of these, 19.4% were pedestrians, 16.5% drivers of a motor vehicle and 8.6% were motorcyclists (Chart 1). Falls accounted for 22.96% and 10.06% were due to assaults. Other causes included sports injuries (1.38%) and non-accidental injuries (0.77%). In 7.82% of the cases the mechanism of injury was not clear (Table 2).
Chart 1.
Mechanism of chest injury after road traffic accident (RTA)
Table 2.
Mechanism of injury and outcome
| Accident description | Died | Lived | Total |
|---|---|---|---|
| Assault | 13 | 105 | 118 |
| Fall <2 m | 15 | 85 | 100 |
| Fall >2 m | 25 | 142 | 167 |
| Not available | 9 | 9 | |
| Other | 15 | 76 | 91 |
| RTA | 149 | 514 | 663 |
| Sport | 1 | 15 | 16 |
| Total | 218 | 946 | 1164 |
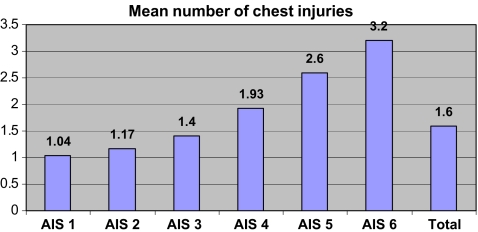
Chest injuries
The chest injuries were classified according to the Abbreviated Injury Severity score (AIS) [1]. The distribution of patients in each group, their associated vital signs on admission and mortality rates are shown in Table 1. Each patient had at least one chest injury (Chart 2). The most severe of these contributed to the patients overall Injury Severity Score (ISS). The most common injury was single or multiple rib fractures (33.3%) followed by lung contusion (15.5%). A simple or tension pneumothorax was present in 10% of the patients whereas a flail segment was present in 7% of the cases. Five percent had an injury to the heart or a large vessel in the chest and 4% had a haemothorax. A further 4% had a sternal fracture. Other injuries included injuries to the airways and thoracic spine (Table 3).
Chart 2.
Mean number of chest injuries
Table 3.
Major chest injury in patients forming the study group
| Chest injury | Number of patients (%) |
|---|---|
| Single or multiple rib fracture | 387 (33.3 %) |
| Lung contusion | 181 (15.5 %) |
| Pneumothorax | 116 (10%) |
| Flail chest | 85 (7%) |
| Heart or large vessel injury | 58 (5%) |
| Sternal fracture | 47 (4%) |
| Other injury | 290 (25%) |
Complications
The incidence of adult respiratory distress syndrome (ARDS), multi-organ failure (MOF), pneumonia and acute renal failure (ARF) was analysed (Table 1). Patients with AISchest score of 1 or 6 did not have any of the above complications. In the AISchest 2 group, three had ARDS, four had pneumonia and two had acute renal failure (ARF). From the patients of the AISchest 3 group, six had ARDS, six had pneumonia, five ARF and one patient had MOF. In the AISchest 4 patient group, ten had ARDS, four had pneumonia, three had MOF and four had ARF. Finally, there were three ARDS, five pneumonias, one MOF and two ARF in those patients with an AISchest of 5.
Admission to the intensive care unit
Of patients with an AISchest 1 score, 25% were admitted to the ICU. The mean length of stay was 4.5 days. Similarly, 18% of the AISchest 2 group of patients were admitted to the ICU for a mean length of stay of four days. Although the mean length of stay was similar in AISchest groups 3, 4 and 5 (5.3, 6.3 and 6.1 days, respectively), the percentage of the patients admitted to ICU in these groups was significantly higher than the previous two groups (AISchest 1 + AISchest 2) (18% and 25% versus 42.9%, 44% and 45.5%, respectively). No patients with an AISchest of 6 were admitted to the ICU (Table 1).
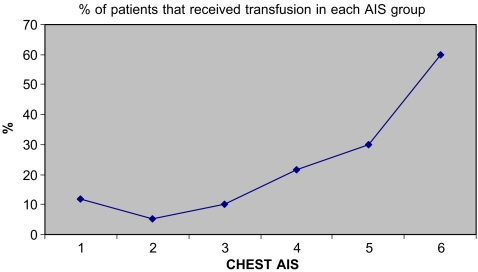
Blood transfusion requirements trauma room
There was no statistical difference between the six patient groups regarding the amount of blood transfused in the A&E Department (p > 0.05). The units of blood transfused among the different AISchest groups are shown in Table 4 and in Chart 3.
Table 4.
Mean units of blood transfused in each AISchest group
| Chest Abbreviated Injury Severity (AIS) | Mean units of blood transfused (SD) | No. receiving transfusion |
|---|---|---|
| 1 | 3.83 ± 2.99 | 6 |
| 2 | 2.08 ± 1.78 | 12 |
| 3 | 3.52 ± 2.47 | 50 |
| 4 | 4.66 ± 3.56 | 56 |
| 5 | 6.05 ± 6.27 | 35 |
| 6 | 4.33 ± 1.52 | 3 |
Chart 3.
% of patients that received transfusion in each Abbreviated Injury Severity (AIS) group
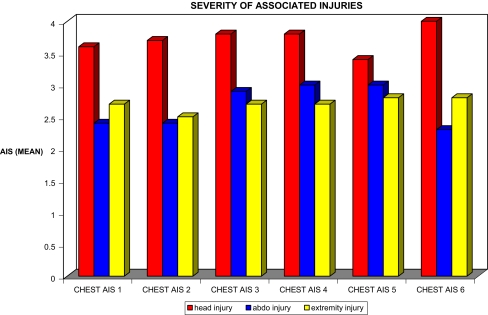
Associated injuries
Chart 4 demonstrates the severity of the associated head, abdominal and extremities injuries in each group of patients.
Chart 4.
Severity of associated injuries
An associated head injury was found in 50.1% of the patients with an AISchest = 1. This figure was significantly higher than all the other groups (p < 0.05). The lowest percentage was noted in those patients with an AISchest of 2 (18.8%). The percentages in AISchest groups 3, 4, 5, and 6 were 34.8%, 39.1%, 42.1% and 40%, respectively. The mean GCS score in each patient group is summarised in Table 5.
Table 5.
Number of patients with head injury and mean GCS in each AISchest group
| Chest AIS | Number of patients with head injury | Mean GCS (SD) |
|---|---|---|
| 1 | 51 | 10.82 ± 5.52 |
| 2 | 233 | 13.64 ± 3.41 |
| 3 | 489 | 10.89 ± 5.36 |
| 4 | 257 | 9.89 ± 5.62 |
| 5 | 121 | 9.16 ± 5.53 |
| 6 | 5 | 4.40 ± 3.13 |
GCS Glasgow Coma Score, AIS Abbreviated Injury Severity
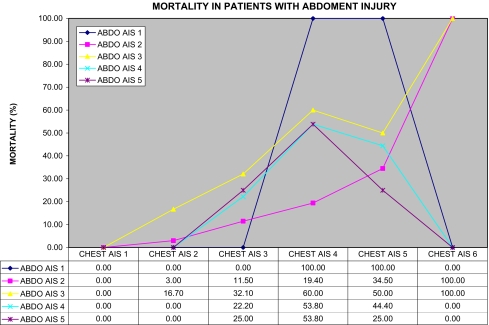
Of those with an AISchest = 1 score, 23.5% had associated abdominal injuries. The percentage in AISchest group 2 was similar (20.9%), and groups 3 and 5 had 45.6% and 45% abdominal injuries, respectively. The incidence was 31% in group 4. The highest incidence was 60% in group 5.
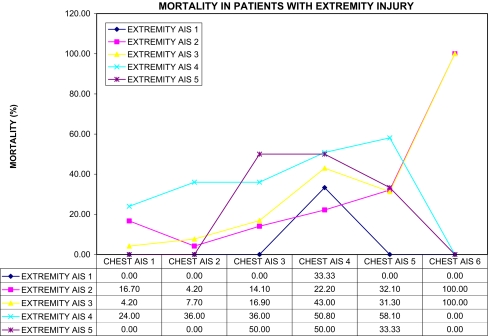
Patients in AISchest group 6 had the highest incidence (80%) of associated extremity injuries, followed by group 1 (72%). Groups 2 and 3 were similar (46.6% and 48%, respectively). The percentage in group 4 was 62.8% and that in group 5 was 58.7%.
Operations and investigations
A total of 111 (9.5%) patients underwent surgical treatment or specialist investigation of their chest injury. There were no patients in the chest AISchest = 1 group who underwent treatment. In group 2, 26 (11.1 %) patients underwent an arch aortogram. They were all negative. Four people in this group underwent internal fixation of thoracic spine fractures. Two patients underwent thoracotomies for uncontrolled haemorrhage.
Sixteen patients in the AISchest 3 group had negative arch aortograms, and one had a positive aortogram. This was subsequently treated nonoperatively. There were three thoracic spine fixations and nine thoracotomies. Two patients had surgical repair of injuries to their tracheas.
There were 12 negative aortograms in the AISchest 4 group. Seven people underwent thoracic spine fracture fixation. Overall, there were eight thoracotomies.
Nine people had negative aortograms and nine had positive aortograms in the AISchest 5 group. All the patients with positive results had surgical treatment of their aortic injuries. Fifteen patients underwent thoracotomies.
Two patients from the AISchest 6 group that were transferred to the operating room died due to uncontrolled haemorrhage.
The outcome of the operated patients in all AISchest groups is demonstrated in Table 6.
Table 6.
Mortality rate of operated patients in each AISchest group
| Category | Chest AIS group | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| % taken to theatre from A&E | N/A | 0 | 28.1 | 39.3 | 43.6 | 100 |
| Mortality in the operated patients | N/A | 0 | 3.1 | 17.9 | 38.5 | 100 |
| Mortality in those operated as an emergency | N/A | 0 | 11.1 | 45.5 | 47.1 | 100 |
AIS Abbreviated Injury Severity, N/A not applicable
Mortality
The overall mortality in patients with blunt chest trauma reached 218 (18.7%). As expected, patients of group 6 had the highest mortality rate (100%). Interestingly, patients of group 1 (chest AIS = 1) had a higher mortality rate than group 2 and 3 patients (Chart 5).
Chart 5.
Mortality
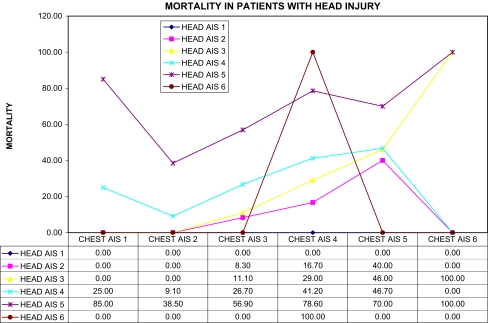
Charts 6–8 demonstrate the correlation between chest AIS, associated injuries and mortality.
Chart 7.
Mortality in patients with head injury
Chart 6.
Mortality in patients with abdomen injury
Chart 8.
Mortality in patients with extremity injury
Discussion
The systematic stratification of trauma by means of different scores is continuously validated and updated [19]. AIS-based systems (Abbreviated Injury Scale) have been extensively used in the literature, estimating ISS (Injury Severity Score) as a classical method of assessment of injury severity. There is an ongoing debate among alternative grading scores including the International Classification of Diseases (ICD-based systems), New Injury Severity Score (NISS) [18], Thoracic Trauma Severity Score (TTS) [19], Hannover Polytrauma Score (PTS) [20] and systems that include physiological data such as the Trauma Injury Severity (TRISS) [6] or the Acute Physiology and Chronic Health Evaluation (APACHE) [15] score. However, the superiority of these grading scores in predicting outcome is restricted by their complexity [10].
The severity of the specific injuries in this study was graded according to the Abbreviated Injury Scale which has been validated to correlate with the impact of the injury to the overall survival of the patient [10]. This is also borne out in this study with the patients in the higher AIS groups having both a higher overall ISS and mortality rate. However, the efficiency of AIS has been extensively debated [2, 8, 10, 16]. One of the characteristics of the ISS is that it does not always have a linear relationship with mortality [8].
Clarke et al. [10] in a series of 41,364 patients, concluded that ICD-9 coding adequately predicts survival based on anatomical injury alone, with no advantage from extra coding of AIS codes. The same authors have noticed that although the mortality rate was related to AIS score, as expected, there was one exception, that is, patients with a single injury and an AIS score of 1 had a higher mortality rate than patients whose single injury had an AIS score of 2, 3 or 4. This was thought to be associated with incomplete diagnostic workup that could only be verified by autopsy. In our series, the unexpected finding was the higher ISS and significantly higher mortality in those with AISchest score of 1 compared to those with AISchest score of 2. This was a running theme throughout the other parameters investigated.
Our review of the literature has yielded a small number of sound reports specifically looking at the effects of thoracic trauma on injury severity and outcome [9, 11, 13, 19, 20, 22]. Thoracic trauma bears a significant weight in the debate as to the fundamental decision between early total care (ETC) versus damage control orthopaedics (DCO) [16].
In their series of 1,495 blunt polytrauma patients with thoracic injury, Pape et al. [19] concluded that radiographically determined injuries to the lung parenchyma have a closer association with adverse outcome than chest wall injuries but are often not diagnosed 24 hours after injury. However, they stressed the fact that decisions for early total care, such as surgery for long bone fractures, may be flawed if this information is used alone. Consequently, they have introduced a thoracic trauma severity score (TTS) [19] in order to improve the accuracy of prediction of outcome.
Richter et al. [20] examined 581 car occupants who sustained a thoracic injury. They averaged an AISchest = 2.5 and ISS = 24.2. Although less severe chest injuries were included in this series (in our series AISchest = 3.15 ± 1.01 and ISS = 26.7), their results are also in keeping with the finding that the severity of thoracic injury is a prognostic factor of clinical course.
Clark et al. [9] reviewed 144 trauma patients with flail chest and/or pulmonary contusion. In this series the mortality rate was more than doubled when a combined pulmonary contusion and flail chest (42%) were present. Overall, factors found to be associated with a higher morbidity and mortality included severe associated thoracic injuries, a high ISS, the presence of shock, falls from heights, and the combination of pulmonary contusion and flail chest.
Chest trauma (AIS > 2) was also among the factors associated with increased mortality in patients with pelvic fractures, as has been shown in the study of Gustavo Parreira et al. [11]. In the same study, interestingly, the severity of the pelvic fracture itself, in terms of characteristics of or the type, didn’t significantly correlate with the mortality rate.
Recent evidence by Hildebrand et al. [12] has shown that polytraumatised patients with blunt chest trauma have shown significant differences in mortality and morbidity between two separate groups of patients treated in Germany and the United Kingdom, respectively. Even though demographic data and injury pattern of the two patient populations did not significantly differ, mortality in the United Kingdom was 9% higher than in Germany. The authors postulated that treatment could be more beneficial with: (a) more aggressive initial blood transfusion protocols, (b) kinetic therapy in ICU, and (c) prolonged ICU versus HDU treatment.
Our study attempts to present significant data as to the epidemiology and outcome of blunt chest injuries to overall severity and outcome of polytraumatised patients. A weak point is the inability to draw sufficient conclusions as to the aetiology of the results (especially regarding mortality of the AISchest1 group), due to the lack of trauma scoring by systems that include physiological parameters. Despite this limitation, our study has a significant exception to add, that is, minor chest injuries (AISchest = 1) were associated with mortality comparable to injuries involving an AISchest = 3. Additionally, the vast majority of polytraumatised patients with an AISchest = 1 died in ICU soon after admission (time to death of 2.5 days on average is only longer than AISchest = 6). Admission GCS was also comparable to AISchest = 3. Overall, apart from AISchest = 6, the most lethal combination of injuries involved an AIShead = 5 with an AISchest = 1.
The distribution of associated injuries was independent of the injury severity of the chest. This can be seen from the balanced distribution of the head, abdominal, and extremities injuries in the six AISchest groups. As a result, the blood transfused to the patients of the six groups did not differ significantly. The high percentage of head injuries in AISchest 1 group can be attributed to the initial absorption of the impact of injury by the head. However, the mean GCS score didn’t significantly differ among the six groups.
Patients that were transferred to the operating theatre acutely had higher mortality rate than those who where operated in a later stage. The only exception is that patients of the AISchest 6 group died irrespective of the timing of surgery. Even though we have no specific data to clarify the reasons why some patients went acutely to the operating room and others did not, it seems that the concept of “early total care” [14] is once again under reconsideration. Studies have shown that “borderline patients“, that is, patients with severe head, thoracic or chest trauma and patients with high Injury Severity Score [17], have better chances of survival when the treatment approach of “damage control” [21] is applied.
Conclusions
Patients with blunt chest trauma in the higher AIS groups had both a higher overall ISS and mortality rate. In contrast to the impact of higher severity, minimal chest injury severity (AISchest1) showed higher ISS and significantly higher mortality compared with AISchest2 or 3. In these groups of patients we speculate that the chest was spared, as most of the impact during the course of the accident was absorbed by the head (head injury). This theory also explains the shorter time period before death seen in patients belonging to the AISchest1 group.
Acknowledgments
Conflict of interest The authors declare that there is no conflict of interest.
References
- 1.AAAM (1998) The Abbreviated Injury Scale, 1990 revision. American Association for the Advancement of Automotive Medicine, Des Plaines, Illinois
- 2.Adams VI, Carrubba C. The Abbreviated Injury Scale: application to autopsy data. Am J Forensic Med Pathol. 1998;19:246–251. doi: 10.1097/00000433-199809000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Baker SP, O’Neill B, Haddon W, Jr., Long WB. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. doi: 10.1097/00005373-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Bergeron E, Lavoie A, Clas D, et al. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54:478–485. doi: 10.1097/01.TA.0000037095.83469.4C. [DOI] [PubMed] [Google Scholar]
- 5.Boulanger BR, Stephen D, Brenneman FD. Thoracic trauma and early intramedullary nailing of femur fractures: are we doing harm? J Trauma. 1997;43:24–28. doi: 10.1097/00005373-199707000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma score and the Injury Severity Score. J Trauma. 1987;27:370–378. doi: 10.1097/00005373-198704000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Bulger EM, Edwards T, Klotz P, Jurkovich GJ. Epidural analgesia improves outcome after multiple rib fractures. Surgery. 2004;136:426–430. doi: 10.1016/j.surg.2004.05.019. [DOI] [PubMed] [Google Scholar]
- 8.Bull JP. Measures of severity of injury. Injury. 1978;9:184–187. doi: 10.1016/0020-1383(78)90004-9. [DOI] [PubMed] [Google Scholar]
- 9.Clark GC, Schecter WP, Trunkey DD. Variables affecting outcome in blunt chest trauma: flail chest vs. pulmonary contusion. J Trauma. 1988;28:298–304. doi: 10.1097/00005373-198803000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Clarke JR, Ragone AV, Greenwald L. Comparisons of survival predictions using survival risk ratios based on International Classification of Diseases, 9th revision and Abbreviated Injury Scale trauma diagnosis codes. J Trauma. 2005;59:563–567. [PubMed] [Google Scholar]
- 11.Gustavo Parreira J, Coimbra R, Rasslan S, et al. The role of associated injuries on outcome of blunt trauma patients sustaining pelvic fractures. Injury. 2000;31:677–682. doi: 10.1016/S0020-1383(00)00074-7. [DOI] [PubMed] [Google Scholar]
- 12.Hildebrand F, Giannoudis PV, Griensven M, et al. Management of polytraumatized patients with associated blunt chest trauma: a comparison of two European countries. Injury. 2005;36:293–302. doi: 10.1016/j.injury.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 13.Johnson JA, Cogbill TH, Winga ER. Determinants of outcome after pulmonary contusion. J Trauma. 1986;26:695–697. doi: 10.1097/00005373-198608000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Johnson KD, Cadambi A, Seibert GB. Incidence of adult respiratory distress syndrome in patients with multiple musculoskeletal injuries: effect of early operative stabilization of fractures. J Trauma. 1985;25:375–384. doi: 10.1097/00005373-198505000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. doi: 10.1097/00003246-198510000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Linn S. The Injury Severity Score—importance and uses. Ann Epidemiol. 1995;5:440–446. doi: 10.1016/1047-2797(95)00059-3. [DOI] [PubMed] [Google Scholar]
- 17.Nast-Kolb D, Waydhas C, Jochum M, et al. Is there a favorable time for the management of femoral shaft fractures in polytrauma? Chirurg. 1990;61:259–265. [PubMed] [Google Scholar]
- 18.Osler T, Baker SP, Long W. A modification of the Injury Severity Score that both improves accuracy and simplifies scoring. J Trauma. 1997;43:922–925. doi: 10.1097/00005373-199712000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Pape HC, Remmers D, Rice J, et al. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49:496–504. doi: 10.1097/00005373-200009000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Richter M, Krettek C, Otte D, et al. Correlation between crash severity, injury severity, and clinical course in car occupants with thoracic trauma: a technical and medical study. J Trauma. 2001;51:10–16. doi: 10.1097/00005373-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Scalea TM, Boswell SA, Scott JD, et al. External fixation as a bridge to intramedullary nailing for patients with multiple injuries and with femur fractures: damage control orthopedics. J Trauma. 2000;48:613–621. doi: 10.1097/00005373-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Schulman AM, Claridge JA, Carr G, et al. Predictors of patients who will develop prolonged occult hypoperfusion following blunt trauma. J Trauma. 2004;57:795–800. doi: 10.1097/01.TA.0000140835.65944.54. [DOI] [PubMed] [Google Scholar]
- 23.Snyder CL, Jain VN, Saltzman DA, et al. Blunt trauma in adults and children: a comparative analysis. J Trauma. 1990;30:1239–1245. doi: 10.1097/00005373-199010000-00008. [DOI] [PubMed] [Google Scholar]