Abstract
In this prospective study, our aim was to compare the functional results and radiographic outcomes of fusion and Bryan Cervical Disc replacement in the treatment of two-level cervical disc disease. A total of 65 patients with two-level cervical disc disease were randomly assigned to two groups, those operated on with Bryan Cervical Disc replacement (31) and those operated on with anterior cervical fusion with an iliac crest autograft and plate (34). Clinical evaluation was carried out using the visual analogue scale (VAS), the Short Form 36 (SF-36) and the neck disability index (NDI) during a two year follow-up. Radiological evaluation sought evidence of range of motion, stability and subsidence of the prosthesis. Substantial reduction in NDI scores occurred in both groups, with greater percent improvement in the Bryan group (P = 0.023). The arm pain VAS score improvement was substantial in both groups. Bryan artificial cervical disc replacement seems reliable and safe in the treatment of patients with two-level cervical disc disease.
Résumé
Cette étude prospective a pour but de comparer les résultats fonctionnels et radiographiques des patients ayant bénéficié soit d’une fusion, soit d’une athrodèse, soit d’une prothèse discale dans le traitement des lésions dégénératives des disques cervicaux portant sur deux niveaux. 65 patients présentant de telles lésions ont été randomisés en deux groupes, ceux traités par la prothèse discale de Bryan (31) et ceux traités par ostéosynthèse antérieure avec autogreffe illiaque et plaque (34). L’évaluation clinique a été réalisée en utilisant le score douleur VAS, (échelle analogique), le score SF-36, la raideur de la nuque index NDI, après deux ans de recul. L’évaluation radiologique permet de mettre en évidence les secteurs de mobilité de stabilité et la migration de la prothèse. Une diminution significative du score NDI est observée dans les deux groupes avec un pourcentage plus important d’amélioration dans le groupe des prothèses de type Bryan (p = 0.023). Le score douleur est nettement amélioré dans les deux groupes néanmoins il semble que la prothèse de type Bryan permet d’avoir des résultats beaucoup plus fiables et beaucoup plus sûrs dans le traitement de ces patients présentant des lésions discales dégénératives cervicales sur deux niveaux.
Introduction
Cervical myelopathy is a relatively common spinal condition. The current standard of care for this is anterior cervical discectomy and fusion (ACDF), usually with an iliac crest autograft, with or without plating. Anterior cervical fusion provides excellent symptomatic relief in the short term. Evidence has recently accumulated to suggest that surgical fusion results in increased biomechanical stresses and accelerated degeneration of the neighbouring spinal motion segments [6, 19]. Other limitations of fusion are a 10–30% perioperative morbidity rate from pseudarthrosis, morbidity from bone grafting or use of allograft, complications relating to plating and adverse muscular effects induced by immobilisation [1, 12, 18]. Shortcomings of ACDF remain including hardware failures.
How to prevent transitional-level disease and maintain normal cervical motion after discectomy is currently an area of intense scientific investigation in the treatment of cervical myelopathy. The Bryan Cervical Disc Prosthesis is designed to preserve motion, avoid limitation of fusion and allow patients to quickly return to routine activities. It also avoids the morbidity of bone graft harvest.
This study was carried out between December 2004 and April 2006. This prospective, controlled, randomised clinical trial was conducted to evaluate the safety and effectiveness of the Bryan Cervical Disc in patients with myelopathy caused by two-level cervical disc disease in Han Nationality.
Material and methods
This was a prospective, randomised and controlled study, approved by the local Ethics Committee of Qilu Hospital of ShanDong University (People’s Rebulic of China). The study consisted of 65 patients with spondylotic myelopathy or cervical radiculopathy. The patients were randomised into two treatment groups: (1) a two-level cervical arthroplasty with the Bryan Cervical Disc (Medtronic Sofamor Danek, Memphis, TN, USA) (investigational group, N = 31,) or (2) a two-level ACDF with an iliac crest autograft and plate (control group, N = 34). All patients had intractable cervical radiculopathy or myelopathy resulting from a disc herniation or stenosis at two adjacent levels from C3–4 to C6–7. And patients had to fail conservative care for 12 weeks.
All patients were evaluated serially by neurological examination as well as pain and functional outcome instruments. An independent radiologist performed radiographic assessment of motion and device stability. The modified Odom’s criteria were used to measure overall results.
The exclusion criteria were the presence of significant anatomical deformity and previous cervical procedure and patients with severe osteoporosis or spinal infection.
The pre- and postoperative, neutral-position, lateral radiographs were evaluated for sagittal alignment in all patients. Preoperative magnetic resonance (MR) imaging and computed tomography were performed in all patients to determine the origin of radiculopathy and myelopathy. The patient demographic data are shown in Table 1.
Table 1.
Demographic information
| Variable | Control (N = 34) | Investigational (N = 31) | P |
|---|---|---|---|
| Mean age | 47 | 45 | 0.385 |
| Men | 50.0% (17/34) | 51.6% (16/31) | 0.902 |
| Marital status | |||
| Divorced | 5.8% (2/34) | 6.3% (2/31) | 1.000 |
| Married | 94.2% (32/34) | 93.7% (19/31) | 1.000 |
| Smokers | 20.6% (7/34) | 19.7% (6/31) | 0.930 |
| Race (Han nationality) | 100% (34/34) | 100% (31/31) | |
| Arm pain VAS | 7.2 | 7.1 | 0.827 |
| Neck pain VAS | 7.1 | 7.3 | 0.6631 |
| NDI | 51 | 50 | 0.805 |
| SF-36 physical component | 34 | 35 | 0.485 |
Surgical technique: investigational group
A transverse incision is made in a skin crease at the appropriate disc level on the right side of the neck. After exposure of the disc space, table-mounted retractors provide stability and visualisation for insertion of the milling guide. Discectomy is performed and the disc space distracted. The guide is fixed to the vertebral bodies above and below the distracted disc at the appropriate sagittal angle (perfectly parallel to the disc space) as measured by the preoperative fluoroscopic image. A final check of the correct size is made, and the end plates are smoothed out with a burr. The end plates are then machined with a milling tool that matches the size and contour of the prosthesis. The guide is removed with the distractor pins remaining. Decompression of the spinal canal and neuroforamen is then performed. The artificial disc is filled with saline and the seal plugs are tightened. The prosthesis is then gently placed into the milled interspace. The distractor is removed and final fluoroscopic images are obtained. Then another prosthesis is placed following the same procedure; all procedures were performed by one surgeon (LN).
Surgical technique: control group
A transverse incision is used. Using optical magnification and by passing medially from the carotid sheath and laterally from the oesophagus and trachea, the anterior aspect of the cervical spine can be reached. After identification of the correct level, the anterior longitudinal ligament is cut and the intervertebral disc excised. Finally, the end plates are removed from the cartilage and an appropriately sized iliac crest autograft is placed in the interspace, and patients undergo anterior cervical plating with the Orion Cervical Plate System (Medtronic Sofamor Danek, Memphis, TN, USA).
Assessment of results
The data collected were demographic data and outcomes data. Clinical evaluation included Odom’s criteria by the surgeon, arm pain score (VAS), neck pain score (VAS) and neck disability index (NDI) by the patient. The Short Form 36 (SF-36) outcomes assessments were made before surgery and at one and six weeks, three, six and 12 months and two years.
Radiographic evaluation included static and dynamic flexion-extension lateral images in standing position. These were assessed preoperatively and postoperatively at one, three, six, 12 and 24 months. The pre- and postoperative angular motion at target level was examined. Radiographic measurement data were collected from three observers. Each of them measured twice, and the mean value was used for analysis.
Statistical assessments
The Mann-Whitney U test was used to assess the statistical significance of postoperative score change from the preoperative in NDI, VAS and SF-36. It was also used to assess the change of motion scores at target level; categorical variables data were analysed using chi-square tests for continuous variables. Statistical comparisons between the treatment groups were performed by using analysis of variance. The 0.05 value was used to define statistical significance. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS Version 12.0) software.
Results
A total of 65 patients were enrolled in this study; there were 19 men and 12 women in the Bryan group (N = 31) and 20 men and 14 women in the control group (N = 34). No differences in demographics were present between the groups (P > 0.05) (Table 1).
One patient from the study group (prosthesis) and two patients from the control group were lost to follow-up.
Clinical study results
Preoperatively, there was no statistical difference in symptoms between the two groups (P = 0.10). NDI and VAS improved significantly from before surgery to the two year follow-up in both groups (P < 0.001).
Neck pain VAS before surgery was 7.1 (control group) and 7.3 (Bryan group). At the 12-month follow-up it was 2.5 (control group) and 1.9 (Bryan group). At the two year follow-up it was 2.6 (control group) and 1.5 (Bryan group) (P = 0.012).
Arm pain VAS before surgery was 7.2 (control group) and 7.1 (Bryan group). At the 12-month follow-up it was 2.4 (control group) and 1.8 (Bryan group). At the two year follow-up it was 2.7 (control group) and 1.4 (Bryan group) (P = 0.013).
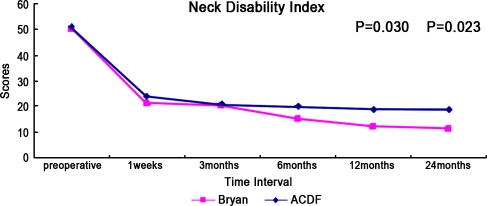
NDI before surgery was 51 (control group) and 50 (Bryan group). At the 12-month follow-up it was 18 (control group) and 12 (Bryan group) (P = 0.030). At the two year follow-up it was 19 (control group) and 11 (Bryan group) (P = 0.023) (Fig. 1).
Fig. 1.
Neck disability index
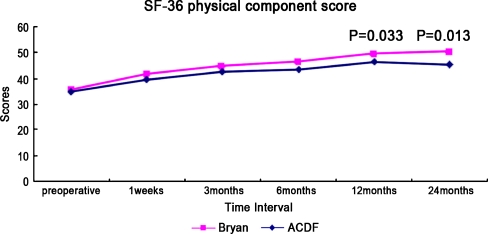
The preoperative SF-36 physical component score was 34 (control group) and 35 (Bryan group). At the 12-month follow-up it was 46 (control group) and 49 (Bryan group) (P = 0.033). At the two year follow-up it was 45 (control group) and 50 (Bryan group) (P = 0.013) (Fig. 2).
Fig. 2.
SF-36 physical component score
According to Odom’s scale, the outcomes of 30 patients in the Bryan group followed up at 24 months were rated as excellent in 24, good in five and fair in one. In the control group all 32 patients were followed up at 24 months with outcomes rated as excellent in 22, good in five, fair in four and poor in one.
Radiographic analysis showed no evidence of subsidence or excursion in the Bryan group. The Bryan group retained an average of 7.9° of flexion-extension at 24 months; this did not represent a statistically significant change from the preoperative measurements (P = 0.35). In contrast, the average range of motion in the fusion group was 0.5° at 24 months, a significant change from the preoperative measurements (P < 0.001).
Complications
No cerebrospinal fluid leak or wound haematomas were observed in this study. There were no vascular or neurological complications, no spontaneous fusions and no device failures or explantations in the Bryan cohort. One patient has a deep vein thrombosis in the Bryan cohort, and one patient has dysphagia in the control group.
Discussion
Anterior cervical discectomy and fusion (ACDF) may be considered to be the standard procedure for treatment of degenerative disc disease of the cervical spine [4, 5]. However, there are clues that ACDF may result in progressive degeneration of the adjacent segments [10, 15]. To avoid this, there have been numerous attempts to develop and use artificial cervical discs [3, 9]. Compared with cervical fusion, disc replacement offers the theoretical biomechanical advantage of preservation of motion at the operative level which reduces stresses at the adjacent level [6]. Maintenance of physiological motion, and prevention of increased stresses, may protect the adjacent level from late degeneration [2]. Additionally, postoperative immobilisation is avoided, allowing earlier return to function, including work. Other complications of fusions, such as pseudarthrosis, bone grafting and morbidity of plating, are avoided.
The Bryan Cervical Disc Prosthesis was first reported as being used for the management of cervical spondylotic disease in 2002 by Goffin et al. [8]. This multicentre, prospective study described preliminary results with insertion of the disc following anterior cervical discectomy for single-level degenerative disease. The outcome tools that were used included the Cervical Spine Research Society Assessment Scale and the SF-36.Results were reported using modified Odom’s criteria. Success, defined by the investigators as excellent, good or fair, was reported in 86% of patients at six months and 90% at one year. respectively, exceeding the study’s targeted success rate of 85%.
There are few reports about two-level Bryan Disc replacement [1, 9]. Our study demonstrates significant improvement (Bryan group vs ACDF group) in outcome measures at 24 months, including arm pain VAS, neck pain VAS, NDI and SF-36 physical component score. Although both surgical groups had statistically significant improvement in all outcome measures at two years with respect to their preoperative scores, the Bryan group showed better clinical outcomes in comparison to the ACDF group. The results of the our study are similar to the study of Sasso et al. [16], a large prospective, controlled, randomised study on Bryan Cervical Disc arthroplasty for patients with one-level cervical disc disease followed to 24 months.
Goffin et al. [9] reported early clinical results with two-level implantation of the Bryan Cervical Disc at one year. The success rate was 82% at six months and 96% at one year; no device failures or subsidence were observed in any patient. At the one year follow-up, flexion-extension range of motion per level averaged 7.4° in the two-level group. Anderson et al. [1] reported early clinical results of 39 patients with the Bryan Cervical Disc implanted at two adjacent levels. Thirty patients have reached the one year endpoint; 21 of the patients were rated as excellent, two as good, five as fair and one as poor. SF-36 functional outcome measures similarly improved postoperatively. The physical component summary averaged 37.3 preoperatively and 46.8 at the 12-month follow-up. The mental component summary averaged 35.4 preoperatively and improved to 45.2 one year after surgery.
The use of the Bryan Disc prosthesis has also been recently described for the management of spondylotic myelopathy in single-level disease. Sekhon reported early results of nine cases of spondylotic myelopathy which were treated with Bryan Disc prosthesis replacement. Follow-up ranged from one to 17 months. On average, Oswestry NDI scores improved by 51.4 points. Duggal et al. [7] also compared outcomes in patients suffering from soft disc herniations with those patients with spondylotic ridging causing foraminal stenosis. No statistically significant difference was found with respect to outcome scores between the two groups.
Although there are several reports of well-known side effects such as heterotopic ossification after Bryan Disc insertion, we did not encounter notable heterotopic ossification or spontaneous fusion in the follow-up period of our study. The incidence varies and the cause remains to be seen in further follow-up [13, 14, 17].
One of the potential criticisms of artificial discs is that in the absence of fusion there may be further pain. Our analysis of VAS and NDI shows that this has not been a problem in our patients. The radiological results showed that 93.3% of 30 patients retained motion at the target segment at two years. Our results compare favourably with the experience of Lafuente et al. [11], in which 91% of 42 patients had evidence of movement in the prosthesis at one year.
It is extremely important to understand the appropriate indication for two-level cervical arthroplasty. The indications for two-level disc replacement are in patients who are undergoing anterior cervical discectomy and fusion for two-level degenerative disc disease associated with symptomatic nerve root and/or spinal cord compression. This includes patients with disc herniation, cervical foraminal stenosis and myelopathy. Contraindications to two-level disc replacement include prior laminectomy, osteoporosis, severe facet joint arthrosis, infection and cervical instability.
This research demonstrated that the Bryan Cervical Disc replacement was shown to be reliable and safe for the treatment of patients with two-level cervical disc disease. It should be considered that our patient population is small and follow-up period is short, and long-term outcome data collected five to ten years after prosthesis implantation will be necessary to demonstrate the putative advantages of disc arthroplasty in two-level cervical disc disease.
References
- 1.Anderson PA, Sasso RC, Rouleau JP. The Bryan Cervical Disc: wear properties and early clinical results. Spine J. 2004;4(6 Suppl):303S–309S. doi: 10.1016/j.spinee.2004.07.026. [DOI] [PubMed] [Google Scholar]
- 2.Auerbach JD, Wills BP, McIntosh TC. Evaluation of spinal kinematics following lumbar total disc replacement and circumferential fusion using in vivo fluoroscopy. Spine. 2007;32(5):527–536. doi: 10.1097/01.brs.0000256915.90236.17. [DOI] [PubMed] [Google Scholar]
- 3.Bertagnoli R, Yue JJ, Pfeiffer F. Early results after ProDisc-C cervical disc replacement. J Neurosurg Spine. 2005;2:403–410. doi: 10.3171/spi.2005.2.4.0403. [DOI] [PubMed] [Google Scholar]
- 4.Bohlman HH, Emery SE, Goodfellow DB. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Caspar W, Geisler FH, Pitzen T, et al. Anterior cervical plate stabilization in one- and two-level degenerative disease: overtreatment or benefit? J Spinal Disord. 1998;11:1–11. doi: 10.1097/00002517-199802000-00001. [DOI] [PubMed] [Google Scholar]
- 6.DiAngelo D, Foley K, Vossel K, et al. Anterior cervical plating reverses load transfer through multilevel strut-grafts. Spine. 2000;25:783–795. doi: 10.1097/00007632-200004010-00005. [DOI] [PubMed] [Google Scholar]
- 7.Duggal N, Pickett GE, Mitsis DK, et al. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus. 2004;17:E9. doi: 10.3171/foc.2004.17.3.9. [DOI] [PubMed] [Google Scholar]
- 8.Goffin J, Casey A, Kehr P, et al. Preliminary clinical experience with the Bryan Cervical Disc Prosthesis. Neurosurgery. 2002;51:840–845. doi: 10.1097/00006123-200209000-00048. [DOI] [PubMed] [Google Scholar]
- 9.Goffin J, Calenbergh V, Loon J, et al. Intermediate follow-up after treatment of degenerative disc disease with the Bryan Cervical Disc Prosthesis: single-level and bi-level. Spine. 2003;28:2673–2678. doi: 10.1097/01.BRS.0000099392.90849.AA. [DOI] [PubMed] [Google Scholar]
- 10.Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004;4(6 Suppl):190S–194S. doi: 10.1016/j.spinee.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Lafuente J, Casey ATH, Petzold A, et al. The Bryan cervical disc prosthesis as an alternative to arthrodesis in the treatment cervical spondylosis: 46 consecutive cases. J Bone Joint Surg Br. 2005;87(4):508–512. doi: 10.1302/0301-620X.87B4.15436. [DOI] [PubMed] [Google Scholar]
- 12.Silber JS, Anderson DG, Daffner SD, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine. 2003;28:134–139. doi: 10.1097/00007632-200301150-00008. [DOI] [PubMed] [Google Scholar]
- 13.Mehren C, Suchomel P, Grochulla F, et al. Heterotopic ossification in total cervical artificial disc replacement. Spine. 2006;31:2802–2806. doi: 10.1097/01.brs.0000245852.70594.d5. [DOI] [PubMed] [Google Scholar]
- 14.Pickett GE, Sekhon LH, Sears WR, et al. Complications with cervical arthroplasty. J Neurosurg Spine. 2006;4:98–105. doi: 10.3171/spi.2006.4.2.98. [DOI] [PubMed] [Google Scholar]
- 15.Reitman CA, Hipp JA, Nguyen L, et al. Changes in segmental intervertebral motion adjacent to cervical arthrodesis: a prospective study. Spine. 2004;29:E221–E226. doi: 10.1097/00007632-200406010-00022. [DOI] [PubMed] [Google Scholar]
- 16.Sasso RC, Smucker JD, Hacker RJ, et al. Artificial disc versus fusion: a prospective, randomized study with 2-year follow-up on 99 patients. Spine. 2007;32:2933–2940. doi: 10.1097/BRS.0b013e31815d0034. [DOI] [PubMed] [Google Scholar]
- 17.Peng-Fei S, Yu-Hua J. Cervical disc prosthesis replacement and interbody fusion: a comparative study. Int Orthop. 2008;32(1):103–106. doi: 10.1007/s00264-006-0287-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.St John TA, Vaccaro AR, Sah AP, et al. Physical and monetary costs associated with autogenous bone graft harvesting. Am J Orthop. 2003;32:18–23. [PubMed] [Google Scholar]
- 19.Wigfield C, Gill S, Nelson R, et al. Influence of an artificial cervical joint compared with fusion on adjacent-level motion in the treatment of degenerative cervical disease. J Neurosurg. 2002;96(1 Suppl):17–21. doi: 10.3171/spi.2002.96.1.0017. [DOI] [PubMed] [Google Scholar]