Abstract
The goal of this study was to assess the efficacy of one-stage surgical management for children with spinal tuberculosis by anterior decompression, bone grafting, posterior instrumentation, and fusion. Between January 2002 and December 2006, 15 cases with spinal tuberculosis were treated with one-stage posterior internal fixation and anterior debridement. All cases were followed-up for an average of 30.3 months (range 12–48 months). The average neurological recovery in the patients was 0.93 grades on the scale of Frankel et al. (Paraplegia 7:179–192, 1969). The average preoperative kyphosis was 36° (range 19–59°), and the average postoperative kyphosis was 23° (range 15–38°) at final follow-up. At final follow-up, minimal progression of kyphosis was seen, with an average kyphosis of 27° (range 16–40°). An average loss of correction of 4° was seen at final follow-up. One-stage surgical management for children with spinal tuberculosis by anterior decompression, bone grafting, posterior instrumentation, and fusion was feasible and effective.
Introduction
Tuberculosis of the spine is still prevalent in many parts of the world and is an important orthopaedic problem [12]. It is known that spinal tuberculosis is more severe, dangerous and disabling in children than it is in adults. Children represent a high-risk group for acquiring the disease, and it still remains a leading cause of paraplegia in developing nations [19, 21, 22, 24]. It is believed that aggressive surgical treatment should be adopted in the management of such patients with spinal tuberculosis [8, 25]. We report here a group of 15 children with spinal tuberculosis treated by one-stage anterior interbody autologous bone grafts and posterior instrumentation. The aim of this clinical study is not only to verify the importance of early reconstruction of spinal stability, but also to evaluate the results of this method.
Patient population
From January 2002 to December 2006, 15 consecutive children with spinal tuberculosis were enrolled in the study. There were seven males and eight females. The mean age at the time of diagnosis and treatment initiation was 10.3 years (range 5–16 years). Diagnosis was based on clinical and haematological criteria. All patients had the symptoms of tuberculosis, such as weight loss, moderate fever, and fatigue. The patients were admitted due to severe back pain or paraparesis, with mean symptom duration of 3.63 months (range 1–5 months). The thoracic spine was involved in six patients, the thoraco-lumbar spine (T11-L2) in four and the lower lumbar spine in five. The ESR was used to evaluate whether the lesion was “active” or not, and whether the disease was healed. The angle of the kyphosis was measured on lateral radiographs by drawing a line on the upper surface of the first normal vertebra above the lesion and one through the lower surface of the first normal vertebra below the lesion, measured with an average of 36° (range 19–59°). The classification of Frankel et al. [4] was used to assess the neurological compromise, resulting in two patients with grade B, three with grade C, six grade D and four grade E (normal neurological status.)
Preoperative
All patients received routine chest X-rays and sputum examination for the tubercle bacillus, but all were found to be without open tuberculosis or acute miliary pulmonary tuberculosis (Fig. 1). Except for cases which required emergency operations due to severe neurological deficit, all patients received standard antituberculous chemotherapy. Antitubercular therapy was started immediately after the preliminary diagnosis of tuberculous spondylitis. All patients received four first-line antitubercular drugs (i.e. isoniazid, rifampicin, ethambutol, and pyrazinamide) for 4–12 weeks before operation and bed rest for at least three weeks before surgery. Surgery was planned only if there was no evidence of recovery. Intraoperative specimens taken from the lesion site revealed tuberculous spondylitis by histological analysis or a positive acid-fast stain or culture in all patients. Pathological evaluation revealed typical caseating necrosis and granulomatous formation in all patients. Acid-fast stains from the local lesion sites or culture for the mycobacterium were positive in fourteen patients. When the patients regained normal appetite without low fever, anaemia and hypoproteinemia, surgery was carried out.
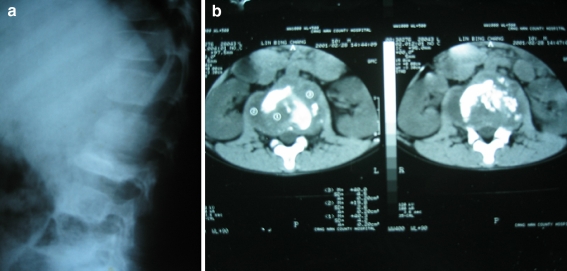
Fig. 1.
Preoperative radiographs showing an anterior segmentation defect at L3
Operative
The operation was carried out in two steps. The surgery was performed under general endotracheal anaesthesia. All patients were operated upon in the lateral position. Normally, the approach was from the severely damaged side of the spine. In the first step all patients underwent anterior radical debridement, decompression and autogenous bone grafting, as described by Hodgson and Stock [6]. The abscess was drained and the necrotic material within the body and disc above and below the affected vertebral bodies was identified and resected with conventional rongeurs and curettes down to bleeding normal bone. The decompressive procedure was performed down to the epidural space. After careful haemostasis, a quantity of normal saline was used for space irrigation to eliminate residual tuberculous tissue. Then, 3–4 g of streptomycin was placed in the operation area. Slots were made in healthy bleeding bone of the vertebral bodies above and below the affected levels, and the spinal defect was measured. The resultant gap was repaired with suitable-length bone grafts. Bone grafts were harvested from the iliac crest or rib in this procedure. The interbody fusion technique was initiated using an autografting bone applied between the vertebrae by means of an elongated bone impactor, and a local drainage tube was inserted routinely before the incision was closed. After the anterior surgical procedure, the patient’s position was changed to prone and a posterior midline incision was made. In the second step, the spine was stabilised using a transpedicular screw and rod system. Exposing the vertebral laminae of involved segments, the posterior pedicle screw system was installed to complete kyphosis correction. Finally, another drainage tube was placed through the erector spinae. The average operative time was 263 minutes (range 231–421 minutes). The average blood loss was 650 ml (range 330–1080 ml) which increased with the operative time. The average postoperative stay was ten days (range 7–14 days).
Postoperative
The drain was usually removed after 72 hours. After operation, bracing for three months was recommended. All patients were treated with an antituberculous chemotherapy regimen for 12–18 months. The usual regimen followed was four-drug chemotherapy (rifampicin, isoniazid, ethambutol, and pyrazinamide) for eight weeks followed by three drugs (rifampicin, isoniazid, and ethambutol) for six weeks and two drugs (rifampicin and isoniazid) for the remainder of the period. Liver functions and sedimentation rates were monitored carefully at regular intervals. Follow-up examination was performed during the first year at six weeks, three months, nine months and one year. Subsequent follow-ups were at six-month intervals. All cases were followed-up for an average of 30.3 months (range 12–48 months). The parameters used in the follow-up were local deformity angle, ESR, spinal bony fusion, and neurological status.
Results
The wounds were healed without chronic infection or sinus formation. All patients achieved fusion. There was no recurrence of the disease in any of the patients at the last follow-up (Figs. 2 and 3).
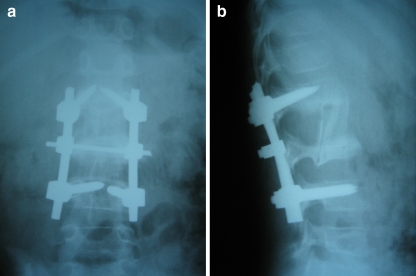
Fig. 2.
Postoperative radiographs showing placement of autogenous bone graft, supplemented with dorsal fusion with instrumentation. Postoperative segmental kyphosis measures 15°
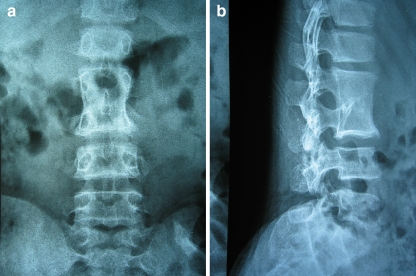
Fig. 3.
Four-year follow-up radiographs showing good incorporation of the autogenous bone graft and maintenance of the correction
Neurological status
Three patients improved two grades and eight patients improved one grade (Table 1). The average neurological recovery in the patients was 0.93 grades on the scale of Frankel et al. [4].
Table 1.
Neurologic grading
| Preoperative | Number of cases | Postoperative | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | ||
| A | 0 | 0 | 0 | 0 | 0 | 0 |
| B | 2 | 0 | 0 | 0 | 2 | 0 |
| C | 3 | 0 | 0 | 0 | 2 | 1 |
| D | 6 | 0 | 0 | 0 | 0 | 6 |
| E | 4 | 0 | 0 | 0 | 0 | 4 |
Deformity
The average postoperative kyphosis was 23° (range 15–38°). At final follow-up, minimal progression of kyphosis was seen, with an average kyphosis of 27° (range 16–40°). An average loss of correction of 4° was seen at final follow-up.
Complications
Complications occurred in three patients. One had a prolonged intercostal drainage tube in situ for five days due to persistent air leak, which resolved without any further intervention. Pneumonitis occurred in one patient, which responded well to antibiotics. We found that the anterior graft displaced in one patient. No complications related to instrumentation occurred. There was no mortality.
Discussion
The spine constitutes almost 50% of the osteoarticular tuberculosis [13], usually presenting with a spine deformity such as kyphosis, neurological deficit and even paraplegia [8, 25]. Antituberculosis chemotherapy is very important to cure the disease and prevent recurrence [18]. It should be emphasised that surgery cannot replace chemotherapy in managing spinal tuberculosis [15]. Chemotherapy with radical surgery is the basic treatment of spine tuberculosis. It must be regular and long-lasting. Although chemotherapy is the mainstay in the management of spinal tuberculosis, surgical procedures are still important.
The management of spinal tuberculosis is a combination of clinical and surgical treatment.
Indications for surgery are neurological deficits, spinal instability, severe and/or progressive kyphosis, no response to chemotherapy treatment, non-diagnostic and large paraspinal abscess [8, 25]. The spinal cord can be compressed by the inflammatory focus, debris and caseation from the anterior aspect; therefore, to be decompressed, an anterior approach is necessary. This radical anterior procedure led to complete neurological recovery in most cases [15]. Surgical treatment of tuberculosis of the spine remains controversial. Indications for surgery vary from one centre to another [1, 8, 15, 25]. There is a wide spectrum of treatment options available for children with tuberculosis. A judicious use of conservative therapy and operative decompression when indicated is the usual management [18].
For the spinal lesion, adequate debridement, decompression and anterior graft placement is used, although this procedure has been indicated mainly in adults [2, 28] with few reports in children in the literature. One-stage surgical management for children with anterior decompression, bone grafting, posterior instrumentation and fusion can be safely performed in children in our experience.
Spinal tuberculosis is a common cause of severe kyphotic deformity. Severe kyphosis is more often a complication of childhood spinal tuberculosis than of adult disease [9, 19, 20]. In spite of effective treatment for spinal tuberculosis, it is common to find residual kyphosis and instability at the end of treatment [21]. Moon [14] reported that combining chemotherapy with anterior autogenous bone grafting following radical debridement is an efficient method to cure spinal tuberculosis and prevent progression of kyphotic deformity. There was a reduction of the angles of kyphosis and deformity following surgery, which was maintained throughout subsequent years of follow-up. In our 15 patients this has resulted in an improvement in the correction of the deformity as well as encouraging neurological recovery and allowing early mobilisation. Reconstruction of spinal stability is beneficial to heal spinal tuberculosis and avoid recurrence. Tuberculosis of the spine is an unstable lesion that tends to progress at least until there is sound bony fusion. Bone fusion of the vertebrae is thought to be the most reliable evidence of healing of spinal tuberculosis [1]. Without instrumentation, the grafted bone may displace or may be absorbed and a long period of external fixation may be required, marring the therapeutic effect of this surgery. Thus, many authors had explored the feasibility of internal fixation after debridement and bone grafting [5]. In order to reduce deformity, posterior fixation is followed by anterior debridement and fusion. In our series, all cases were performed with autogenous bone graft and internal fixation. Posterior instrumental stabilisation and anterior interbody fusion were found helpful in arresting the disease early, providing early fusion, preventing progression of kyphosis, and correcting the kyphosis [11].
We performed one-stage surgical management for children with spinal tuberculosis by anterior decompression, bone grafting, posterior instrumentation, and fusion. This method has been proven as a useful technique [3, 10, 23, 27]. The anterior approach leads the surgeon directly to the lesion and allows good visualisation. Decompression of the spinal cord anteriorly can be obtained directly and completely [17]. Posterior instrumentation can effectively prevent the excessive growth of the posterior column in children. Rigid stabilisation of the spine allows early mobilisation of these patients when compared to the prolonged periods of immobilisation which were originally recommended [10]. Posterior instrumentation surgery was not a hazard in spinal tuberculosis infection. The adherence properties of Mycobactarium tuberculosis to stainless steel was evaluated experimentally [16]. It has been proven that tubercle bacillus has no adhesiveness to autogenous bone and instruments, and it is safe to graft bone and use instrumentation in an infection focus [26]. There were no cases of persistence or recurrence of infection after surgery, and instrumentation provided immediate stability and protected against development of kyphotic deformity. We therefore suggest that posterior instrumentation should be undertaken to prevent kyphosis in children.
Neurological complications are the most feared in spinal tuberculosis [7]. Prompt treatment can reverse paralysis and minimise the potential disability. Some patients' significant neurological improvement was seen immediately postoperatively followed by a return of the paraplegia due to subsequent cord compression. Many factors determined such a partial recovery of neurological function; long-term compression of the spinal cord resulting from the delay of diagnosis and surgery, was, no doubt, the major reason. It is important for children to have early diagnosis and early therapy to prevent spinal tuberculosis.
In conclusion, for children with tuberculosis, systemic antituberculosis chemotherapy was the cornerstone of treatment, with tuberculous focus clearance second, spinal fusion by bone grafting third, and kyphosis correction fourth. Through these surgical procedures, problems such as radical debridement, anterior spinal decompression, reconstruction of spinal stability by bone grafting, and kyphosis correction may be achieved. One-stage surgical management for children with spinal tuberculosis by anterior decompression, bone grafting, posterior instrumentation, and fusion was feasible and effective.
References
- 1.Boachie-Adjei O, Squillante RG. Tuberculosis of the spine. Orthop Clin North Am. 1996;27:95–103. [PubMed] [Google Scholar]
- 2.Chacko AG, Moorthy RK, Chandy MJ. The transpedicular approach in the management of thoracic spine tuberculosis: a short-term follow up study. Spine. 2004;29:363–367. doi: 10.1097/01.brs.0000137063.64650.e1. [DOI] [PubMed] [Google Scholar]
- 3.Dai LY, Jiang LS, Wang W, et al. Single-stage anterior autogenous bone grafting and instrumentation in the surgical management of spinal tuberculosis. Spine. 2005;30:2342–2349. doi: 10.1097/01.brs.0000182109.36973.93. [DOI] [PubMed] [Google Scholar]
- 4.Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia. 1969;7:179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 5.Guven O, Kumano K, Yalcin S, et al. A single stage posterior and rigid fixation for preventing kyphosis in the treatment of spinal tuberculosis. Spine. 1994;19:1039–1043. doi: 10.1097/00007632-199405000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Hodgson AR, Stock FE. Anterior spinal fusion a preliminary communication on the radical treatment of Pott’s disease and Pott’s paraplegia. Br J Surg. 1956;44:266–275. doi: 10.1002/bjs.18004418508. [DOI] [PubMed] [Google Scholar]
- 7.Jain AK. Treatment of tuberculosis of the spine with neurologic complications. Clin Orthop Relat Res. 2002;398:75–84. doi: 10.1097/00003086-200205000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Jain AK. Tuberculosis of the spine. Clin Orthop Relat Res. 2007;460:39–49. doi: 10.1097/BLO.0b013e318073bd29. [DOI] [PubMed] [Google Scholar]
- 9.Jain AK, Aggarwal PK, Arora A, et al. Behaviour of the kyphotic angle in spinal tuberculosis. Int Orthop. 2004;28:110–114. doi: 10.1007/s00264-003-0516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim DJ, Yun YH, Moon SH, et al. Posterior instrumentation using compressive laminar hooks and anterior interbody arthrodesis for the treatment of tuberculosis of the lower lumbar spine. Spine. 2004;29:275–279. doi: 10.1097/01.BRS.0000129027.68574.06. [DOI] [PubMed] [Google Scholar]
- 11.Laheri VJ, Badhe NP, Dewnany GT. Single stage decompression, anterior interbody fusion and posterior instrumentation for tuberculous kyphosis of the dorso-lumbar spine. Spinal Cord. 2001;39:429–436. doi: 10.1038/sj.sc.3101185. [DOI] [PubMed] [Google Scholar]
- 12.Lönnroth K, Raviglione M. Global epidemiology of tuberculosis: prospects for control. Semin Respir Crit Care Med. 2008;29:481–491. doi: 10.1055/s-0028-1085700. [DOI] [PubMed] [Google Scholar]
- 13.Mehta JB, Emery MW, Girish M, et al. Atypical Potts disease: localized infection of the thoracic spine due to Mycobacterium avium-intracellulare in a patient without human immunodeficiency virus infection. South Med J. 2003;96:685–688. doi: 10.1097/01.SMJ.0000054604.75361.57. [DOI] [PubMed] [Google Scholar]
- 14.Moon MS. Tuberculosis of the spine. Controversies and a new challenge. Spine. 1997;22:1791–1797. doi: 10.1097/00007632-199708010-00022. [DOI] [PubMed] [Google Scholar]
- 15.Moon MS, Moon YW, Moon JL, et al. Conservative treatment of tuberculosis of the lumbar and lumbosacral spine. Clin Orthop Relat Res. 2002;398:40–49. doi: 10.1097/00003086-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Oga M, Arizono T, Takasita M, et al. Evaluation of the risk of instrumentation as a foreign body in spinal tuberculosis. Clinical and biologic study. Spine. 1993;18:1890–1894. doi: 10.1097/00007632-199310000-00028. [DOI] [PubMed] [Google Scholar]
- 17.Ozdemir HM, Us AK, Ogun T. The role of anterior spinal instrumentation and allograft fibula for the treatment of Pott disease. Spine. 2003;28:474–479. doi: 10.1097/00007632-200303010-00012. [DOI] [PubMed] [Google Scholar]
- 18.Parthasarathy R, Sriram K, Santha T, et al. Short-course chemotherapy for tuberculosis of the spine. J Bone Joint Surg Br. 1999;81:464–471. doi: 10.1302/0301-620X.81B3.9043. [DOI] [PubMed] [Google Scholar]
- 19.Rajasekaran S. The natural history of post-tubercular kyphosis in children. J Bone Joint Surg Br. 2001;83:954–962. doi: 10.1302/0301-620X.83B7.12170. [DOI] [PubMed] [Google Scholar]
- 20.Rajasekaran S. The problem of deformity in spinal tuberculosis. Clin Orthop Relat Res. 2002;398:85–92. doi: 10.1097/00003086-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Rajasekaran S, Prasad SA, Dheenadhayalan J, et al. Morphological changes during growth in healed childhood spinal tuberculosis. J Pediatr Orthop. 2006;26:716–724. doi: 10.1097/01.bpo.0000230326.21707.71. [DOI] [PubMed] [Google Scholar]
- 22.Salazar GE, Schmitz TL, Cama R, et al. Pulmonary tuberculosis in children in a developing country. Pediatrics. 2001;108:448–453. doi: 10.1542/peds.108.2.448. [DOI] [PubMed] [Google Scholar]
- 23.Talu U, Gogus A, Ozturk C, et al. The role of posterior instrumentation and fusion after anterior radical debridement and fusion in the surgical treatment of spinal tuberculosis: experience of 127 cases. J Spinal Disord Tech. 2006;19:554–559. doi: 10.1097/01.bsd.0000211202.93125.c7. [DOI] [PubMed] [Google Scholar]
- 24.Teo HE, Peh WC. Skeletal tuberculosis in children. Pediatr Radiol. 2004;34:853–860. doi: 10.1007/s00247-004-1223-7. [DOI] [PubMed] [Google Scholar]
- 25.Tuli SM. Tuberculosis of the spine: a historical review. Clin Orthop Relat Res. 2007;460:29–38. doi: 10.1097/BLO.0b013e318065b75e. [DOI] [PubMed] [Google Scholar]
- 26.Yilmaz C, Selek HY, Gurkan I, et al. Anterior instrumentation for the treatment of spinal tuberculosis. J Bone Joint Surg Am. 1999;81:1261–1267. doi: 10.2106/00004623-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Zhang HQ, Guo CF, Xiao XG, et al. One-stage surgical management for multilevel tuberculous spondylitis of the upper thoracic region by anterior decompression, strut autografting, posterior instrumentation, and fusion. J Spinal Disord Tech. 2007;20:263–267. doi: 10.1097/01.bsd.0000211281.68400.1b. [DOI] [PubMed] [Google Scholar]
- 28.Zhao J, Lian XF, Hou TS, et al. Anterior debridement and bone grafting of spinal tuberculosis with one-stage instrumentation anteriorly or posteriorly. Int Orthop. 2007;31:859–863. doi: 10.1007/s00264-006-0253-1. [DOI] [PMC free article] [PubMed] [Google Scholar]