Abstract
While short-term outcome studies of patients following total hip arthroplasty (THA) have shown compromised walking ability, it is often assumed that temporospatial parameters will return to normal levels at long-term follow-up, especially for younger patients. Temporospatial parameters were determined for 149 THA patients selected arbitrarily from routine ten-year post-operative review clinics. Patients were divided into five age groups: 54–64, 65–69, 70–74, 75–79 and over 80 years. The parameters of speed, step length, stride length and cadence were measured. All age groups displayed significantly reduced velocity, step length and stride length compared to an age-matched normal group. There was no difference in most of the temporospatial parameters between the age groups. This study shows that even younger THA patients at long-term follow-up do not regain normal age-matched walking characteristics.
Résumé
Alors que les études présentant les patients ayant bénéficié d’une prothèse totale de hanche montrent une altération immédiate des possibilités de marche, il semble assuré que les paramètres temporospatiaux se normalisent après un long suivi, spécialement chez les patients jeunes. Ces paramètres temporospatiaux ont été déterminés chez 149 patients sélectionnés, de façon arbitraire et routinière après avoir été revus 10 ans après l’intervention chirurgicale. 10 ans après l’intervention, les patients ont été divisés en 5 groupes d’âge: 54–64, 65–69, 70–74, 75–79 et après 80 ans. Les différents paramètres de marche, vitesse, escalier, cadence, etc. ont été mesurés. Quel que soit l’âge, il y a une diminution significative de la rapidité, de la longueur du pas et de longueur de foulée comparés à un groupe témoin normal. Il n’y a pas la plupart du temps de différence, des paramètres temporospatiaux entre les différents groupes d’âge. Cette étude montre que, même chez les patients jeunes, la mise en place d’une prothèse totale de hanche, ne permet pas, à long terme, de récupérer tous les paramètres normaux de la marche.
Introduction
Total hip arthroplasty (THA) secondary to arthritic pain is one of the most common orthopaedic procedures undertaken, with over 300,000 THAs being carried out annually in the USA alone [8]. While THA outcomes have been reported in terms of implant survival time and outcome scores such as the Harris and Oxford hip scores, one of the most objective outcome measures is that of patient walking ability as measured by temporospatial parameters.
The primary objective of the hip replacement operation is the relief of pain. Consequently, while the procedure may allow the patient to execute normal daily tasks pain free, the restoration of normal range of motion at the joint may not occur [10]. It is unknown whether the temporospatial parameters of THA patients return to normal levels in long-term follow-up after the operation. Most studies have considered THA patients in the immediate post-operative period [1, 2] or at short-term follow-up of between one and four years [4–7, 9, 12]. While some of these studies report a return to normal walking speed for patients post-THA between one and three years follow-up [5, 6, 12] others report contrary findings with THA patients failing to achieve normal walking speeds at two to four years follow-up [4, 7, 9]. In those studies which found reduced walking speed post-operatively for THA patients, it is often assumed that THA patients will eventually achieve normal temporospatial levels at longer periods post-operatively [9].
This study seeks to determine whether the temporospatial parameters of a large cohort of THA patients across a wide age range at long-term follow-up (ten years) return to normal levels. This study also sought to examine differences in temporospatial parameters across age strata to investigate whether younger patients display improved temporospatial parameters compared to their older counterparts.
Materials and methods
Patient details and surgical procedure
Patients were arbitrarily selected from ten-year hip replacement review clinics at a regional orthopaedic centre, with 149 patients recruited. Patients were excluded if they reported lower limb pain or if they had experienced other orthopaedic procedures (e.g. knee or ankle replacement) due to possible compromise of that patient’s walking pattern. The average time for which the implant had been inserted was 9.90 years, ranging from 8.91 to 11.44 years. Eight patients had bilateral THA while the remaining 141 had unilateral THA. All replacements were primary arthroplasties (i.e. none were revision arthroplasties).
All operations were performed using a posterior approach by a single orthopaedic surgeon. The implant consisted of a cemented titanium femoral stem with a 28-mm diameter cobalt chrome alloy head (Orthogenesis custom X-press stem, DePuy International, Leeds, UK) articulating against a cemented UHMWPE acetabular cup (Elite cup, DePuy International, Leeds, UK). All components were sterilised using 25 kGy gamma irradiation in an air environment.
Ethical approval was obtained from the local Research Ethics Committee and informed, written consent was provided by all participants. A group of ten fit and active age-matched normal subjects were also tested. An entrance questionnaire [13] was used to exclude normal subjects with walking or lower limb problems. Summary details of the age-matched normal subjects are given in Table 1.
Table 1.
Patient details for the age-stratified groups and the normal elderly group
| Group | Number of subjects | Gender (M:F) | Age, years (range) | Period post-op., years (range) |
|---|---|---|---|---|
| Total THR | 147 | 83:64 | 71.10 (54.44–92.83) | 9.90 (8.91–11.44) |
| 54–64 | 33 | 12:21 | 61.12 (54.44–64.96) | 9.75 (8.91–10.60) |
| 65–69 | 25 | 14:11 | 67.68 (65.02–69.92) | 9.89 (9.19–10.78) |
| 70–74 | 45 | 32:13 | 72.39 (70.16–74.98) | 9.94 (8.99–11.44) |
| 75–79 | 29 | 19:10 | 76.80 (75.03–79.81) | 9.98 (9.43–10.74) |
| > 80 | 15 | 6:9 | 83.90 (80.67–92.83) | 10.01 (9.89–10.28) |
| Normal | 10 | 6:4 | 64.0 (59.2–68.5) | n.a. |
Retro-reflective markers were placed on both feet at the toe (at the second metatarsal head) and heel (over the os calcis at the same vertical height as the toe marker) positions. Together with ground reaction force data from two instrumented force plates (AMTI, Watertown, MA, USA) the beginning and end of the stance phase for each foot were determined. Accurate identification of heel contact and toe-off gait events were determined using thresholding of ground reaction force data (heel contact when F > 20 N, toe-off when F < 20 N). Data were captured with a 6-camera Vicon 612 system at 120 Hz with both THA patients and normal subjects being tested. Each trial consisted of the subject walking a distance of 8 m at self-selected speed. Data from the central section of the walkway, in which the force plates are situated, were used for analysis to ensure the acceleration and deceleration phases of walking were not used. A minimum of three trials were captured for each subject, with a single representative trial used for analysis.
Statistical analysis
The variables analysed were velocity, cadence, step length of the operated and non-operated limbs, stride length and stance phase duration for the operated and non-operated limbs. To test for differences between temporospatial parameters of the operated and non-operated limbs paired t-tests were used. Differences in variables between the age-stratified groups and the normal group and between each of the age-stratified groups were tested using a one-way analysis of variance (ANOVA) with pair-wise comparisons using Tamhane’s T2 test. The significance level for all tests was set at 0.05. Statistical analysis was performed using SPSS version 13.0 (SPSS Inc., Chicago, IL, USA).
Results
Of the 149 patients recruited, one was excluded due to pain during walking and another was excluded due to comprehension problems. Patient details are given in Table 1. Based on the age profiles of the subjects tested, five age strata were used to group the patients tested. These were 54–64 years, 65–69 years, 70–74 years, 75–79 years and 80 years and over. Patient details of each group are given in Table 1.
A summary of temporospatial parameters for each of the five groups and for the elderly normal groups is shown in Table 2. All groups showed significantly reduced velocity, step length and stride length compared to the normal control group. Cadence (step frequency) was not significantly reduced and stance duration was not significantly increased for any age group compared to normal (Table 2). There were no significant differences between any of the age groups for any of the temporospatial parameters measured, apart from reduced step and stride length of the oldest (> 80 years) age group compared to the youngest (54–65 years) age group.
Table 2.
Temporospatial parameters for the age-stratified and elderly normal groups. 1,2,3,4,5,N denote significant difference with the relevant groups (e.g. 5, N denotes significant difference with group 5 and the normal elderly group)
| Group | Age strata | Velocity, m/s (SD) | Cadence, steps/min (SD) | Step length, m (SD) | Stride length, m (SD) | Stance duration, % of gait cycle (SD) |
|---|---|---|---|---|---|---|
| 1 | 54–64 | 1.06 (0.26)N | 111.6 (13.14) | 0.57 (0.10)5,N | 1.13 (0.19)5,N | 62.1 (2.4) |
| 2 | 65–69 | 0.98 (0.24)N | 108.2 (13.9) | 0.54 (0.08)N | 1.08 (0.17)N | 62.5 (2.5) |
| 3 | 70–74 | 1.00 (0.22)N | 109.6 (12.4) | 0.54 (0.10)N | 1.09 (0.19)N | 62.3 (2.3) |
| 4 | 75–79 | 0.99 (0.18)N | 110.22 (10.3) | 0.54 (0.08)N | 1.07 (0.16)N | 62.7 (2.8) |
| 5 | > 80 | 0.82 (0.25)N | 110.9 (15.1) | 0.44 (0.10)1,N | 0.88 (0.25)1,N | 64.1 (2.7) |
| N | Elderly normal | 1.34 (0.13) | 117.2 (9.8) | 0.69 (0.04) | 1.37 (0.07) | 60.9 (1.92) |
Considering patients with unilateral hip replacements (n = 139) from the entire patient cohort, no significant differences were found between the operated limb compared to the non-operated limb for any of the temporospatial parameters measured (Table 3). Similarly, for each of the five age groups no significant differences in temporospatial parameters were found between the operated limb compared to the non-operated limb.
Table 3.
Temporospatial parameters of the operated and non-operated limbs for unilateral patients
| Velocity, m/s (SD) | Cadence, steps/min (SD) | Step length, m (SD) | Stride length, m (SD) | Stance duration, % of gait cycle (SD) | |
|---|---|---|---|---|---|
| Operated | 0.98 (0.24) | 110.1 (13.0) | 0.53 (0.10) | 1.07 (0.20) | 62.0 (6.1) |
| Non-operated | 0.99 (0.24) | 111.0 (12.9) | 0.54 (0.10) | 1.07 (0.20) | 62.2 (6.1) |
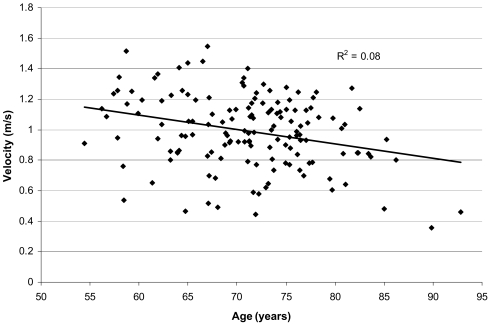
A plot of velocity against age for the entire group showed a trend for walking speed to reduce with increasing age. However, the correlation was relatively poor (r2 = 0.08) with a large degree of scatter (Fig. 1).
Fig. 1.
Velocity against age for THA patients 10 years post-operation
Discussion
While other studies have reported temporospatial parameters of hip replacement patients post-operatively, these have tended to focus on small groups of patients who do not represent typical patients presenting for THA. Furthermore, most studies consider patients at short-term follow-up and the results to date have often been contradictory.
The walking speed of a cohort of 17 THA patients (mean age: 52.6 years) was reported to be approximately 1.05 m/s at one-year follow-up, which was not found to be significantly less than that expected of normal Japanese people [6]. However, a total of six implant types were considered in this small study group, while the normal data referenced were derived from a separate unrelated study. Long et al. tested 18 patients up to two years post-operatively and found that walking speed had indeed returned to normal levels [5]. In contrast, Perron et al. reported an average walking speed of 1.07 m/s for a group of 18 THA female patients six–18 months post-operatively, which was significantly less than for a group of age-matched normal female subjects [9]. Loizeau et al. reported an average speed of 0.78 m/s for a group of four THA patients (mean age: 67.3 years) at mean follow-up of 3.8 years, which was significantly less than a group of four age-matched controls [4]. Sliwinski et al. found reduced velocity (mean: 1.09 m/s) compared to a normal age-matched group in a cohort of 16 THA patients (mean age: 70.9 years) [11]. Patients were tested between two months and two years post-operatively and two different surgical procedures (cemented and uncemented) were considered.
The only other study of the walking ability of THA patients at long-term follow-up considers the temporospatial parameters of a group of 20 female patients (average age: 60) eight to ten years post-operatively [3]. Of these patients, it was noted that they were not representative of a typical THA cohort due to being exclusively female, having a young age profile and the fact that the majority presented for surgery due to hip dysplasia. However, the average velocity of this group eight to ten years post-operatively was 1.12 m/s, which compares well to the average velocity of 1.07 m/s for the 54- to 64-year-old group in this study.
For those patients with unilateral hip replacements there were no significant differences found in any of the measured temporospatial parameters (velocity, step and stride length, stance phase duration and cadence) of the operated limb compared to the non-operated limb for the entire cohort (Table 3). In the immediate post-operative period the step length of the non-operated side has been shown previously to be reduced compared to the operated side due to the inability of the operated limb to extend during walking post-surgery [1]. As the non-operated limb swings through during gait the operated limb is pushed into extension, which is painful for patients in the immediate post-operative period [2]. However, this study shows that differences in step length between the operated and non-operated limbs have been elimated at long-term follow-up (Table 3).
Furthermore, there were no significant differences between any of these temporospatial parameters for any of the five age groups when tested separately. This suggests that symmetry between the operated and non-operated limbs is achieved at long-term follow-up for all the age groups tested. However, despite the significant period of time post-operatively, all groups, including the youngest patients (54–64 years old), showed significantly reduced temporospatial parameters compared to the elderly normal group. This confirms that key gait parameters of velocity and step length do not return to normal levels, even for the youngest patients.
This study reports that while the velocity of the older groups is reduced compared to the younger ones, this difference did not prove to be significantly different (Table 2). Although velocity is approximately inversely associated with age for the cohort as a whole, the correlation is relatively weak (Fig. 1). Consequently while the trend is certainly for reduced velocity and step length with advancing age, a specific correlation between age and walking speed for THA patients cannot be assumed (Fig. 1).
No significant differences in any of the temporospatial parameters were reported between the age strata of 54–79 years old. The most elderly group (> 80 years old) displayed a significantly reduced step and stride length compared to the youngest group (54–64 years old) (Table 2). However, this may be simply due to the reduced walking velocity of this group rather than factors attributable to their hip replacement.
By considering patients who received the same implant from the same surgeon via the same surgical technique at the same hospital this study sought to greatly reduce possible confounding factors and variability associated with previous post-operative studies of patients following joint replacement [6, 9]. This study also sought to ensure that the level of post-operative rehabilitation was reasonably uniform by considering patients at a single time point (i.e. 10 years) post-operatively.
This study shows that THA patients up to 80 years old have remarkably similar temporospatial characteristics, especially those of walking speed and step length. Above this age patients displayed significant reductions in step and stride length and marked but non-significant reductions in velocity. However, these reductions in walking speed and step length are more likely due to advancing age rather than limitations caused by the hip replacement itself. Symmetry of temporospatial parameters between the operated and non-operated limbs was achieved by all patient age groups. This study reveals that at a period of ten years post-operation, crucial temporospatial parameters of velocity and step length do not differ significantly across patient age groups up to 80 years of age. However, all THA age groups displayed significantly reduced velocity and step and stride length compared to normal age-matched controls, suggesting that walking function has not returned to normal levels even for the youngest group of patients ten years post-operatively.
Acknowledgements
The assistance of staff at the Outcomes Assessment Unit and the advice of Mike Parker, Medical Statistician at the Clinical Research Support Centre is very much appreciated.
This study has been supported by the Northern Ireland Research and Development Office Small Grant Scheme.
References
- 1.Bennett D, Ogonda L, Elliott D, et al. Comparison of gait kinematics in patients receiving minimally invasive and traditional hip replacement surgery: a prospective blinded study. Gait Posture. 2006;23:374–382. doi: 10.1016/j.gaitpost.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 2.Bennett D, Ogonda L, Elliott D, et al. Comparison of immediate postoperative walking ability in patients receiving minimally invasive and standard-incision hip arthroplasty: a prospective blinded study. J Arthroplasty. 2007;22:490–495. doi: 10.1016/j.arth.2006.02.173. [DOI] [PubMed] [Google Scholar]
- 3.Kyriazis V, Rigas C. Temporal gait analysis of hip osteoarthritic patients operated with cementless hip replacement. Clin Biomech (Bristol, Avon) 2002;17:318–321. doi: 10.1016/S0268-0033(02)00024-4. [DOI] [PubMed] [Google Scholar]
- 4.Loizeau J, Allard P, Duhaime M, et al. Bilateral gait patterns in subjects fitted with a total hip prosthesis. Arch Phys Med Rehabil. 1995;76:552–557. doi: 10.1016/S0003-9993(95)80510-9. [DOI] [PubMed] [Google Scholar]
- 5.Long WT, Dorr LD, Healy B, et al. Functional recovery of noncemented total hip arthroplasty. Clin Orthop Relat Res. 1993;288:73–77. [PubMed] [Google Scholar]
- 6.Miki H, Sugano N, Hagio K, et al. Recovery of walking speed and symmetrical movement of the pelvis and lower extremity joints after unilateral THA. J Biomech. 2004;37:443–455. doi: 10.1016/j.jbiomech.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Murray MP, Gore DR, Brewer BJ, et al. A comparison of the funtional performance of patients with Charnley and Müller total hip replacement. A two-year follow-up of eighty-nine cases. Acta Orthop Scand. 1979;50:563–569. doi: 10.3109/17453677908989805. [DOI] [PubMed] [Google Scholar]
- 8.Parvizi J, Tarity TD, Herz A, et al. Ninety-day mortality after bilateral hip arthroplasty. J Arthroplasty. 2006;21:931–934. doi: 10.1016/j.arth.2006.02.080. [DOI] [PubMed] [Google Scholar]
- 9.Perron M, Malouin F, Moffet H, et al. Three-dimensional gait analysis in women with a total hip arthroplasty. Clin Biomech (Bristol, Avon) 2000;15:504–515. doi: 10.1016/S0268-0033(00)00002-4. [DOI] [PubMed] [Google Scholar]
- 10.Skinner HB. Pathokinesiology and total joint arthroplasty. Clin Orthop Relat Res. 1993;288:78–86. [PubMed] [Google Scholar]
- 11.Sliwinski MM, Sisto SA, Batavia M, et al. Dynamic stability during walking following unilateral total hip arthroplasty. Gait Posture. 2004;19:141–147. doi: 10.1016/S0966-6362(03)00039-0. [DOI] [PubMed] [Google Scholar]
- 12.Tanaka Y. Gait analysis of patients with osteoarthritis of the hip and those with total hip arthroplasty (in Japanese) Nippon Seikeigeka Gakkai Zasshi. 1993;67:1001–1013. [PubMed] [Google Scholar]
- 13.Winter DA, Patla AE, Frank JS, et al. Biomechanical walking pattern changes in the fit and healthy elderly. Phys Ther. 1990;70:340–347. doi: 10.1093/ptj/70.6.340. [DOI] [PubMed] [Google Scholar]