Abstract
To investigate the long-term clinical results of proximal row carpectomy for treating chronic wrist injuries, we collected the postoperative results of ten patients who underwent this procedure between 1978 and 1996. The evaluation was based on Gartland and Werley and modified Green and O’Brien scoring systems. The follow-up ranged from ten to 29 years. Nine patients could perform daily activities properly, two experienced occasional pain and one moderate pain. Eight patients were rated as excellent, two were good, while none was fair or poor by the former scoring system. Seven patients were rated as good, three were fair and none was excellent or poor by the latter scoring system. No apparent degenerative change was found in the radiocapitate joints apart from a slight change in one patient. The operation is a dependable and durable procedure that results in satisfactory pain relief, improved functional wrist motion and grip strength, allowing most patients to resume their previous work.
Introduction
Since the first report of Stamm on treating chronic wrist injuries and ischaemic necrosis of the lunate with proximal row carpectomy, the procedure has become an approach in treating chronic injuries and functional restoration of the wrist thanks to its capacity to relieve pain and enhance range of motion and grip strength. Nevertheless, this procedure has long been somewhat controversial, being considered as a “salvage procedure”. Criticism includes postoperative loss of grip strength, unsatisfactory range of motion, prolonged rehabilitation time and the potential for progressive painful arthritis.
So far, there have been many different surgical procedures which are used in treating wrist injuries; however, proximal row carpectomy still has not been replaced. Many studies have evaluated outcomes of the procedure with differing results.
Methods
We performed a retrospective review of 12 patients who had undergone proximal row carpectomy for the treatment of some chronic wrist injuries in our hospital between 1978 and 1996. Ten of them were followed up for a duration of ten to 29 years (16.5 years on average).
The operations took place three to 25 months following the injuries (average: 13.5 months). The scaphoid, lunate and triquetrum were excised with the pisiform retained in all cases. A horizontal incision was made along the dorsal line between the ulnar and radial styloids. The skin and the subcutaneous layers were incised to the dorsal extensor retinaculum of the wrist. The proximal scaphoid was exposed by division of the dorsal radiocarpal ligament. After the ligaments of the triquetrum adherent to the ulnar carpal capsule and the palmar radiocarpal ligament were excised, the triquetrum was removed, followed by the lunate and scaphoid. After excision of the proximal carpal row, the capitate was located in the centre of the lunate fossa. Passive wrist flexion and extension were done in neutral and slight radial deviation to detect impingement of the trapezium against the radial styloid [1]. No patients required radial styloidectomy. The carpal capsule was then repaired, the wound closed and pressure dressing applied. Postoperative immobilisation with plaster in a neutral wrist position varied from four to six weeks.
Clinical assessment was performed with two scoring systems. The Gartland and Werley scoring system [2] is ranked according to points given on the basis of four indicators: residual deformity (0–3 points), subjective evaluation of pain and disability (0–6 points), range of motion (0–5 points) and complications (0–5 points), including arthritic change, median nerve complications and finger stiffness. The modified Green and O’Brien [3] system was also employed in our study. This 100-point scale has four categories, with 25 points allocated equally to pain, functional status, range of motion and grip strength (Tables 1 and 2).
Table 1.
Gartland and Werley scoring system and the clinical assessment results of the ten patients
| Item | Score | Patients’ score by number | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| Residual deformity | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Ulnar styloid prominence | 1 | ||||||||||
| Palmar deviation deformity | 2 | ||||||||||
| Radial deviation deformity | 3 | ||||||||||
| Subjective evaluation of pain and disability | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||
| Absent | 0 | ||||||||||
| Occasional pain and slightly limited motion | 2 | 2 | 2 | ||||||||
| Occasional pain and moderate limited motion | 4 | 4 | |||||||||
| Pain, limited motion, disabled | 6 | ||||||||||
| Objective evaluation | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Dorsal extension defect (<45°) | 5 | ||||||||||
| Ulnar deviation defect (<15°) | 3 | ||||||||||
| Supination defect (<50°) | 2 | ||||||||||
| Palmar flexion defect (<30°) | 1 | ||||||||||
| Radial deviation defect (<15°) | 1 | ||||||||||
| Circular motion defect | 1 | ||||||||||
| Lower radioulnar pain | 1 | 1 | |||||||||
| Grip: 60% of opposite side or less | 1 | ||||||||||
| Rotation defect | 2 | ||||||||||
| Complications | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Inflammatory change in joint | 1–5 | 1 | |||||||||
| Median nerve complications | 1 | ||||||||||
| Poor digital function due to plaster use | 2 | ||||||||||
| Total score | 0 | 0 | 2 | 0 | 0 | 3 | 0 | 0 | 0 | 5 | |
Excellent: 0–2; good:3–8; fair: 9–20; poor: >21
Table 2.
Modified Green and O’Brien scoring system and the clinical assessment results of the ten patients
| Item | Score | Patients’ score by number | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| Pain | |||||||||||
| Absent | 25 | 25 | 25 | 25 | 25 | 25 | 25 | 25 | |||
| Occasional | 20 | 20 | 20 | ||||||||
| Moderate, tolerable | 15 | 15 | |||||||||
| Severe, intolerable | 0 | ||||||||||
| Functional status | |||||||||||
| Resumed work | 25 | 25 | 25 | 25 | 25 | 25 | 25 | 25 | 25 | 25 | |
| Constrained work | 20 | 20 | |||||||||
| Able to work but failed to be employed | 15 | ||||||||||
| Unable to work due to pain | 0 | ||||||||||
| Range of motion (percentage of normal status) | |||||||||||
| 100% | 25 | ||||||||||
| 75–99% | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 |
| 50–74% | 10 | ||||||||||
| 25–49% | 5 | ||||||||||
| 0–24% | 0 | ||||||||||
| Grip strength (compared to healthy side) | |||||||||||
| 100% | 25 | ||||||||||
| 75–99% | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 | 15 |
| 50–74% | 10 | ||||||||||
| 25–49% | 5 | ||||||||||
| 0–24% | 0 | ||||||||||
| Total score | 100 | 80 | 80 | 75 | 80 | 80 | 75 | 80 | 80 | 80 | 65 |
Excellent: 90–100; good:80–89; fair: 65–79; poor: <65
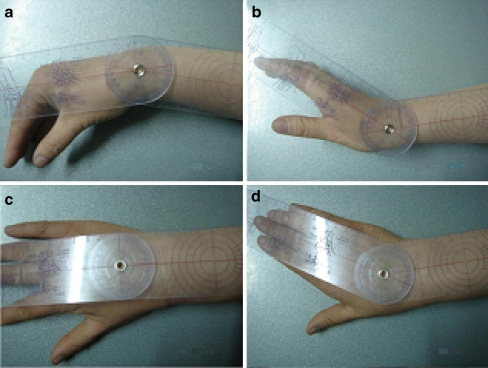
The subjective evaluation including pain and functional status was carried out by the first two authors through questionnaire about pain and disability according to the index description of the two scoring systems on all of the patients who returned to the outpatient department of our hospital for review. The objective evaluation was made possible by careful observation of the affected wrist such as residual deformity and complications. The first two authors used the same goniometer to measure range of motion of the affected wrist, including palmar flexion, dorsal extension, ulnar deviation and radial deviation (Fig. 1), to obtain the percentage of normal status (normal range of motion of wrist joint) in every patient. The Jamar grip meter was used three times in each hand of the ten patients and the average grip score was calculated individually to reveal the percentage of grip strength of the affected side compared to the healthy side. Postoperative anteroposterior (AP) and lateral X-ray films were taken in all patients and evaluated by the first two authors and the corresponding author to assess the extent of inflammatory change of the wrist according to the evaluation standard given in the Gartland and Werley scoring system [2].
Fig. 1.
Motion measurement of the affected wrist in one of the cases. a Palmar flexion. b Dorsal extension. c Radial deviation. d Ulnar deviation
Results
The study group included five male patients (42%) and seven female patients (58%) with an average age of 39 years at the time of undergoing the surgery (range: 21–54 years). Three cases (25%) had operations on the left wrist and nine (75%) on the right, with nine involving the dominant side and three involving the non-dominant side. Underlying conditions included: six chronic fractures of the scaphoid accompanied by trans-scaphoid perilunate fracture dislocation, three trans-scaphoid perilunate fracture dislocations accompanied by ischaemic necrosis of the scaphoid, two perilunate dislocations and one case was advanced-stage Kienböck’s disease (Lichtman IIIA).
Ten patients completed the whole follow-up procedure and two (16.7%) were lost to follow-up. They were one 40-year-old male patient and one 54-year-old female patient. Both of them had operations on the right dominant side wrist after chronic fractures of the scaphoid accompanied by trans-scaphoid perilunate fracture dislocation.
The average age of the ten cases was 52 years at the time of review (range: 45–61 years). They had chronic wrist pain preoperatively, and their range of motion was reduced to different extents compared with the healthy side. After undergoing carpectomy, none needed secondary surgery to treat failure of the procedure.
Gartland and Werley scoring system
According to this system, none of the ten cases showed postoperative residual deformity or loss of motion upon objective evaluation. One case complained of lower radioulnar pain (1 point). Median nerve complications or reduced digital function were not found in any cases, apart from a slight inflammatory change of the wrist joint (1 point) in one patient (10%). As revealed by the subjective evaluation, one patient experienced occasional postoperative pain and moderate limited wrist motion (4 points), and two had occasional pains and slightly limited wrist motion (2 points). Generally, eight patients (80%) were rated as excellent (0–2 points), two (20%) were good (3–8 points), while none were rated as fair or poor (Table 1).
Modified Green and O’Brien scoring system
According to this system, two of the ten patients (20%) had occasional pain (20 points), one (10%) had moderate but tolerable pain (25 points) and none experienced severe pain. The postoperative function allowed nine patients (90%) to resume their previous occupations or retire normally afterwards, with only one (10%) exception, whose work was constrained by the “moderate pain”. By measuring range of motion and calculating the percentage we found a 75–99% wrist motion compared to the normal range in all patients (15 points). Evaluation of grip strength showed that 75–99% of the grip strength on the healthy side was restored on the affected side in all patients (15 points). Eventually, seven of the patients (70%) scored 80 points, rated as good, three (30%) scored 65–79 points, rated as fair, and no one was rated as excellent or poor (Table 2).
Discussion
The two scoring systems are both easy to use and scientific for assessing different wrist problems after operation and thus increasingly cited recently [4]. No statistical analysis was attempted because of our small sample size, yet a few meaningful recommendations are made possible through long-term follow-up and strict evaluation with the two systems.
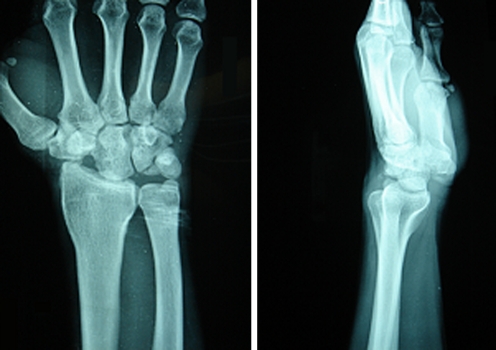
In addition to removal of the diseased carpus and the non-fitting joint, proximal row carpectomy helps to create a “ball-and-socket joint” between the lunate fossa of the distal radius and the capitate (radiocapitate joint). The motion of the capitate on the radius is rolling with a moving centre of rotation due to the different curvature of the lunate fossa and the capitate, viz. hinge-plus-rotation motion [5, 6], which may reduce the distal loading upon the radius and thereby relieve pain to some extent. Salomon and Eaton [7] and DiDonna et al. [8] reported that symptomatic degeneration did not necessarily occurr in the radiocarpal joint after proximal row carpectomy. Inglis and Jones [9] followed up eight cases and observed absence of apparent radiocarpal degeneration as long as 37 years after the procedure. Similar outcomes (only one patient showed a slight inflammatory change in the radiocapitate joint) are also evident in our study (Fig. 2). Our study showed that despite flattening of the capitate or narrowing of the radiocapitate space, patients can achieve good satisfaction with reduced wrist pain.
Fig. 2.
Male patient, undergoing proximal row carpectomy in the left wrist (non-dominant side) for chronic scaphoid fracture accompanied by trans-scaphoid perilunate fracture dislocation, 36 years old at the time of surgery. AP and lateral X-ray films taken at postoperative year 15 showing slight narrowing of the radiocapitate joint without apparent inflammatory changes
Another approach for treating chronic wrist injury is limited wrist arthrodesis, which may reduce wrist pain and deformity; however, it leads to significant decrease in the range of wrist motion. Tomaino et al. [10] found no significant difference in the pain scoring between 15 cases that had undergone proximal row carpectomy and nine cases that had undergone scaphoid excision and limited midcarpal arthrodesis according to the Bach Pain Score Standard [11]. In a similar comparison, Wyrick et al. [12] reported that nine of 11 patients undergoing proximal row carpectomy and wrist arthroplasty experienced no postoperative pain and two had minimal pain, while ten of the 18 receiving scaphoid excision and limited carpal arthrodesis were free of pain, two had minimal pain, one moderate pain and five severe pain. In our study, seven cases were painless on activities of daily living postoperatively, two experienced occasional pain and one complained of moderate pain when performing heavy labour, but none of them required analgesic medication.
The patients had good recovery of their wrist muscle strength, although it was weaker compared with the unaffected side, which could be a result of the relative lengthening of the wrist tendons after proximal row carpectomy. Grip strength was enhanced to 75–99% of the healthy side post-operatively, and there was no complaint of objective weakness in the wrist. Early and medium postoperative muscle strength increases may be attributed to relief of wrist pain [13]. The grip strength of our patients improved over a long time, most of them (90%) were able to continue their previous work.
Range of wrist motion at the time of the last follow-up had considerably increased compared to that prior to surgery. Although unable to restore 100% of the normal status, all of the cases achieved a 75–99% restoration. The lost range of radial deviation and palmar flexion was relatively greater, while the other movements recovered well; accordingly all of the cases could basically perform activities of daily living.
Therefore, the procedure of proximal row carpectomy is not significantly different from limited midcarpal arthrodesis in terms of pain relief. However, the former can maintain the motion of the wrist joint which is preferable, and radiocapitate joint arthrodesis can still be applied in cases when proximal row carpectomy fails or wrist pain continues postoperatively [14, 15]. Severe pain was absent in our study, where the patients were basically able to perform their daily activities, without needing further carpal arthrodesis. Furthermore, a recent study found that the rate of complications such as carpal tunnel syndrome was higher and the duration of hospital stay was longer in the arthrodesis group [16]. We thus believe that proximal row carpectomy should be preferred if both procedures are indicated. Only in specified situations, such as for patients carrying out heavy manual work, do some researchers recommend midcarpal arthrodesis due to the better grip strength postoperatively [17].
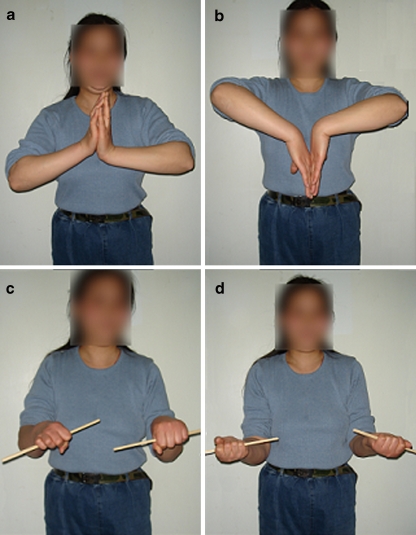
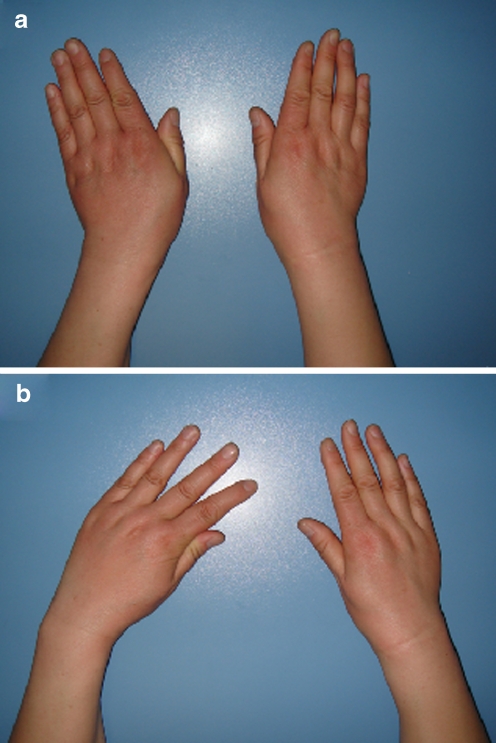
Proximal row carpectomy is currently considered as a suitable surgical solution to chronic wrist injuries, such as chronic scaphoid facture, trans-scaphoid perilunate fracture dislocation, perilunate dislocation and ischaemic necrosis of the lunate bone [18, 19]. Our findings support the view that chronic wrist pain caused by chronic wrist injuries as an indication for the procedure. Chronic wrist injuries are often complicated by serious local disuse osteoporosis and usually cause damage to the neighbouring intercarpal ligaments, leading to compromised blood supply to the carpus; these factors limit options of other procedures. As a result, proximal row carpectomy or limited carpal arthrodesis is the only choice for some younger patients. Three of our patients were aged less than 30 years at the time of surgery, including one case followed up for up to 29 years (Figs. 3 and 4). The procedure afforded all of them satisfactory functional outcomes.
Fig. 3.
Female patient, who underwent proximal row carpectomy in the right wrist (dominant side) at the age of 23 years, with utmost motions of her wrist on both healthy and affected sides 29 years after the operation. a Dorsal extension. b Palmar flexion. c Supination of forearms. d Pronation of forearms
Fig. 4.
Female patient, who underwent proximal row carpectomy in the right wrist (dominant side) at the age of 23 years, with utmost motions of her wrist on both healthy and affected sides 29 years after the operation. a Ulnar deviation. b Radial deviation
As our evaluation and analysis indicate, proximal row carpectomy is helpful for reducing wrist pain and improving grip strength and wrist function. It is a feasible solution and can lead to favourable long-term results in treating some chronic injuries of the wrist.
Acknowledgment
The study was supported by National Natural Sciences Foundation of China (30271317) and Scientific Research Foundation of Sichuan Province, People’s Republic of China.
Footnotes
Ming Liu and Haitao Zhou have contributed equally to this paper.
References
- 1.Stern PJ, Agabegi SS, Kiefhaber TR, et al. Proximal row carpectomy. J Bone Joint Surg Am. 2005;87:166–174. doi: 10.2106/JBJS.E.00261. [DOI] [PubMed] [Google Scholar]
- 2.Gartland JJ, Jr, Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am. 1951;33:895–907. [PubMed] [Google Scholar]
- 3.Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;214:136–147. [PubMed] [Google Scholar]
- 4.Leung F, Tu YK, Chew WY, Chow SP. Comparison of external and percutaneous pin fixation with plate fixation for intra-articular distal radial fractures. A randomized study. J Bone Joint Surg Am. 2008;90:16–22. doi: 10.2106/JBJS.F.01581. [DOI] [PubMed] [Google Scholar]
- 5.Hogan CJ, McKay PL, Degnan GG. Changes in radiocarpal loading characteristics after proximal row carpectomy. J Hand Surg [Am] 2004;29:1109–1113. doi: 10.1016/j.jhsa.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Blankenhorn BD, Pfaeffle HJ, Tang P, et al. Carpal kinematics after proximal row carpectomy. J Hand Surg [Am] 2007;32:37–46. doi: 10.1016/j.jhsa.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 7.Salomon GD, Eaton RG. Proximal row carpectomy with partial capitate resection. J Hand Surg [Am] 1996;21:2–8. doi: 10.1016/S0363-5023(96)80147-X. [DOI] [PubMed] [Google Scholar]
- 8.DiDonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: study with a minimum of ten years of follow-up. J Bone Joint Surg Am. 2004;86:2359–2365. [PubMed] [Google Scholar]
- 9.Inglis AE, Jones EC. Proximal-row carpectomy for diseases of the proximal row. J Bone Joint Surg Am. 1977;59:460–463. [PubMed] [Google Scholar]
- 10.Tomaino MM, Delsignore J, Burton RI. Long-term results following proximal row carpectomy. J Hand Surg [Am] 1994;19:694–703. doi: 10.1016/0363-5023(94)90284-4. [DOI] [PubMed] [Google Scholar]
- 11.Bach AW, Almquist EE, Newman DM. Proximal row fusion as a solution for radiocarpal arthritis. J Hand Surg [Am] 1991;16:424–431. doi: 10.1016/0363-5023(91)90008-Y. [DOI] [PubMed] [Google Scholar]
- 12.Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. J Hand Surg [Am] 1995;20:965–970. doi: 10.1016/S0363-5023(05)80144-3. [DOI] [PubMed] [Google Scholar]
- 13.Lecomte F, Wavreille G, Limousin M, et al. Proximal row carpectomy: 25 cases (in French) Rev Chir Orthop Reparatrice Appar Mot. 2007;93(5):444–454. doi: 10.1016/s0035-1040(07)90326-8. [DOI] [PubMed] [Google Scholar]
- 14.Wyrick JD. Proximal row carpectomy and intercarpal arthrodesis for the management of wrist arthritis. J Am Acad Orthop Surg. 2003;11:277–281. doi: 10.5435/00124635-200307000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Smet L, Degreef I, Robijns F, et al. Salvage procedures for degenerative osteoarthritis of the wrist due to advanced carpal collapse. Acta Orthop Belg. 2006;72:535–540. [PubMed] [Google Scholar]
- 16.Vanhove W, Vil J, Seymortier P, et al. Proximal row carpectomy versus four-corner arthrodesis as a treatment for SLAC (scapholunate advanced collapse) wrist. J Hand Surg Eur Vol. 2008;33(2):118–125. doi: 10.1177/1753193408087116. [DOI] [PubMed] [Google Scholar]
- 17.Dacho AK, Baumeister S, Germann G, et al. Comparison of proximal row carpectomy and midcarpal arthrodesis for the treatment of scaphoid nonunion advanced collapse and scapholunate advanced collapse in stage II. J Plast Reconstr Aesthet Surg. 2007;61(10):1210–1218. doi: 10.1016/j.bjps.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 18.Gündes H, Kurt H, Buluc L, et al. The mid-term results of proximal row carpectomy in the treatment of degenerative wrist joint derangements (in Turkish) Acta Orthop Traumatol Turc. 2004;38:34–41. [PubMed] [Google Scholar]
- 19.Lumsden BC, Stone A, Engber WD. Treatment of advanced-stage Kienböck’s disease with proximal row carpectomy: an average 15-year follow-up. J Hand Surg [Am] 2008;33(4):493–502. doi: 10.1016/j.jhsa.2007.12.010. [DOI] [PubMed] [Google Scholar]