Abstract
The objective of this paper is to evaluate the long-term functional results achieved after open reduction and internal fixation of 24 distal humerus non-unions. Non-unions were extra-articular-extracapsular (11 cases), extra-articular-intracapsular (8 cases) and intra-articular (5 cases). Preoperative elbow range of motion averaged 45°. Time between original trauma and revision surgery averaged 14 months. Stabilisation methods varied according to type and location of the non-union. Follow-up averaged 46 months (range: 18–108). Elbow range of motion at last examination averaged 98°. Flexion averaged 110° and extension loss averaged 17°. The disabilities of the arm, shoulder and hand (DASH) score averaged 16 points. Secondary transposition of the ulnar nerve was necessary in three cases. Sixteen patients reported no pain at last examination, seven had mild pain and one had moderate pain. Distal humerus non-unions present different characteristics; consequently, surgical treatment must be individualised for each patient. Even though they are demanding procedures, bony union and good long-term functional results were achieved.
Résumé
L’objectif de cette étude est d’évaluer à long terme les résultats fonctionnels obtenus après réduction sanglante et fixation interne de 24 pseudarthroses de l’extrémité distale de l’humérus. Matériel et méthode: la pseudarthrose était extra articulaire et extra capsulaire dans 11 cas, extra articulaire et intra capsulaire dans 8 cas et intra articulaire dans 5 cas. La mobilité pre opératoire du coude était en moyenne de 45° et le temps entre le trauma initial et la réintervention de 14 mois. Les méthodes de fixation ont été différentes selon la localisation de la pseudarthrose. Résultats: après 46 mois de suivi en moyenne (de 18 à 108), la mobilité du coude au dernier examen était de 98° en moyenne, la flexion autour de 110° et le défaut d’extension de 17°. Le score DASH a été de 16 points en moyenne. La transposition secondaire du nerf cubital a été nécessaire dans trois cas. 16 patients se plaignaient de douleur au dernier examen, 7 avec une très légère douleur et 1 avec douleur modérée. En conclusion, les pseudarthroses de l’extrémité distale de l’humérus présentent différentes caractéristiques, notamment sur le plan chirurgical, celles-ci devant être individualisées pour chaque patient. Cependant, il s’agit d’une technique très demandeuse qui permet de bons résultats à long terme.
Introduction
Distal humerus non-union is one of the most feared complications in elbow trauma; although it can be painless and may not require treatment, in general it is characterised by marked instability, pain, strength loss and significant functional limitation [7, 17, 20]. Complex fractures, poor bone quality, soft tissue lesions and bad patient selection, particularly if associated with incorrect or inadequate internal fixation, favour complications. The reported incidence of non-union after the treatment of distal humerus fractures ranges between 2 and 10% [7, 21]. The complexity of the treatment of these lesions is usually increased by its association with poor bone quality, small bony fragments difficult to stabilise and to previous operations and approaches compromising soft tissues and the olecranon. Treatment options in distal humerus non-unions include open reduction and internal fixation with plates and screws, intramedullary nails, external fixator, total elbow replacement, interposition arthroplasty, resection arthroplasty, replacement using allograft and elbow arthrodesis. Internal fixation with plates and screws is the treatment of choice in active patients [1, 5, 7, 8, 11, 12, 17, 19, 22]. If surgery is indicated, it must restore function in a long-lasting way; for this it is necessary to achieve bony union, with no pain, and to restore an acceptable range of motion (ROM).
The objective of this paper is to evaluate the long-term functional results achieved after open reduction and internal fixation (ORIF) of 24 distal humerus non-unions, treated in an 11-year period with an average follow-up of 46 months.
Material and methods
Twenty-four patients with non-union at the distal end of the humerus, who underwent ORIF between 1995 and 2006, were retrospectively evaluated. Sixteen patients were male and eight female; their age averaged 45 years (range: 19–73). All fractures were secondary to trauma: 13 patients had high-energy trauma and 11 had low-energy trauma. Reconstruction was indicated only in patients whose distal humerus articular surface was preserved or reconstructible. Non-unions treated with joint replacement, interposition arthroplasty and arthrodesis were excluded. Seven fractures had originally been open; classification of initial fracture type and of the severity of soft tissue lesions was not possible since 21 patients were referred from another institution after failure in the treatment of the original fracture. Of the 24 patients, 23 had had previous operations (range: 1–5); 11 fractures were approached through an olecranon osteotomy. Two patients had had two previous olecranon osteotomies and two presented with an olecranon non-union. Initial stabilisation was performed using: two plates in four cases, one plate in five cases, only screws in six cases, Rush nails in two cases, an intramedullary nail in two cases, an external fixator in two cases and multiple Kirschner wires and screws in two cases. Five patients presented preoperative ulnar nerve neuropraxia and two had radial nerve neuropraxia. The time between original trauma or surgery and revision surgery averaged 14 months (range: 4–46). Non-union was defined as failure in radiographic progression of callus formation six months after initial trauma or surgery and/or implant loosening or breakage at least four months after the original surgery.
Anteroposterior, lateral, oblique and functional X-rays were evaluated to assess bone quality, size and location of fragments, extent of bone loss, type and placement of previous implants, characteristics of the joint surface as well as joint motion and motion at the non-union site. According to their location, non-unions were classified as extra-articular-extracapsular (11 cases), extra-articular-intracapsular (8 cases) and intra-articular (5 cases). The non-unions were classified as described by Weber: 12 atrophic non-unions, six oligotrophic and six hypertrophic. Preoperative elbow ROM averaged 45° (range: 0–95°); two patients presented fibrous ankylosis in extension, one at −15° and the other at −30°. Six patients had active infection. In two infected non-unions a two-stage reconstruction was performed: a cement spacer with antibiotics (gentamicin and vancomycin) was placed in the fracture gap in the first procedure to aid infection control locally, to reconstruct an adequate soft-tissue bed [15], and as the preliminary step to definite osteosynthesis and bone grafting.
The approaches used were: (a) posterior in 21 cases [a transolecranon approach was used in 11 cases, posterior triceps elevating approach (Bryan-Morrey) in four cases and posterior triceps-on approach (Alonso-Llames) in six cases], (b) a lateral humerus approach was used in two cases and (c) a Kocher lateral approach was used in one case. Definitive stabilisation was done using two 3.5-mm reconstruction plates in ten cases (Figs. 1 and 2), a 4.5-mm DCP plate in three cases, a reconstruction plate in two cases, two tension bands in one case, two 4.5-mm DCP plates in one case, two 1/3 tubular plates with 4.5-mm cancellous screws in the columns in one case, a 4.5-mm LC-DCP plate in one case, an extra-articular external fixator in one case, intramedullary nail in one case, tension band with one Rush nail in one case, combination of a 3.5-mm LC-DCP plate and a reconstruction plate in one case, and in one case initially stabilised with an intramedullary nail, autogenous bone graft and two screws were added preserving the nail. Autologous bone graft was used in 15 patients, associated with 1 g of vancomycin in four cases of infected non-union. In three cases with segmental bone loss at the metaphyseal level tricortical bone graft was required to reconstruct the columns; in one of them the stabilisation was protected with a dynamic external fixator for eight weeks to control and neutralise forces at the elbow joint.
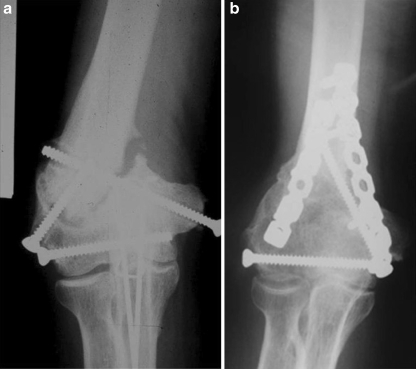
Fig. 1.
a Anteroposterior preoperative X-ray showing a distal humerus non-union with insufficient osteosynthesis using three screws. b Union after stabilisation with two posterior reconstruction plates. The distal screw of the medial plate goes through the medial column
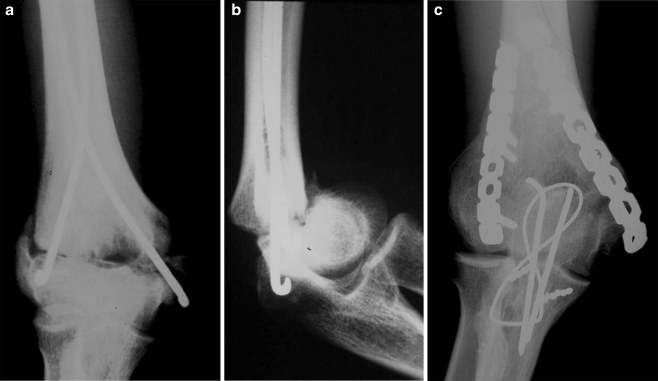
Fig. 2.
a, b Anteroposterior and lateral X-rays: distal humerus extra-articular-intracapsular non-union, previous stabilisation with two Rush nails. c Anteroposterior X-ray showing union 9 years after surgery, olecranon V-type osteotomy approach and stabilisation with two dorsal plates
In extra-articular-extracapsular non-unions the transolecranon approach was avoided; instead, the approach was lateral or posterior (Bryan-Morrey or Alonso-Llames) because the olecranon should be preserved intact when possible, in view of the possible need for arthroplasty in the future. In intra-articular non-unions an intra-articular V-shaped transolecranon osteotomy or a Kocher lateral approach was used providing a better view of the joint surface. In extra-articular-intracapsular non-unions the approaches varied according to previous approaches and operations, and the precise location of the non-union. The ulnar nerve was identified and protected in all cases and was transposed anteriorly in nine cases.
The triceps muscle is usually adherent to the non-union site and was carefully released; when the dissection was extended proximally care was taken not to damage the radial nerve. Once the distal humerus was exposed, implant removal, resection of fibrous, inflammatory, necrosed and synovial tissue and opening of sclerotic surfaces of bone ends was performed. In six patients capsulolysis, arthrolysis, cleaning of olecranon and coronoid fossa and restoration of joint surface were performed, trying to avoid excessive release the soft tissues attached to bone fragments so as to preserve their blood supply. This was followed by reduction of the joint surface, restoration of trochlear length and width and reconstruction of the length and continuity of the columns. In patients approached through an olecranon osteotomy, the osteotomy was stabilised using a tension band; when the approach was performed through triceps reflection, it was reinserted using non-absorbable sutures placed transosseously.
Fluoroscopy was performed to confirm correct placement of the implants and anatomical reduction; once the reconstruction was finished elbow ROM was checked to assess construction stability. After surgery the affected limb was immobilised in extension with a plaster splint for 48 hours and elevated, favouring active shoulder and hand movements. Prompt passive controlled motion (48 hours postoperatively) was started in all cases. The surgeon knows the level of stability achieved by the osteosynthesis so he/she should control and lead postoperative mobilisation.
Results
Follow-up averaged 46 months (range: 18–108). All non-unions healed within five months after surgery. Elbow ROM at last examination averaged 98° (range: 65–125°). Flexion averaged 110° (range: 95–125°) and loss of extension averaged 17° (range: 10–35°). In all cases ROM improved; the improvement was more significant in the two patients with preoperative fibrous ankylosis. Only in one case was there limitation in pronation (−30°). The disabilities of the arm, shoulder and hand (DASH) score averaged 16 points (range: 0–36). No patient presented signs or symptoms of instability. Sixteen patients had no pain at last examination, seven had mild pain and one had moderate pain.
In six patients it was necessary to remove osteosynthesis material because of discomfort at the elbow once union was achieved (after an average of 15 months). Both patients with preoperative radial nerve neuropraxias and the four patients with preoperative ulnar nerve neuropraxias recovered sensitivity and motor function completely; in the ulnar nerve cases anterior subcutaneous transposition was performed at the time of treatment of the non-union. Secondary transposition of the ulnar nerve was necessary in three cases. One of the patients with postoperative ulnar nerve neuropraxia, in whom secondary transposition of the ulnar nerve had been performed (at the time of transposition a neuroma presented caused by irritation produced by the movement of the nerve over the head of one of the screws), had only partially recovered nerve function (this is the patient who reports moderate pain). Four weeks after surgery a patient developed a fracture of the olecranon proximal tip; in the first operation this patient had a V-shaped intra-articular osteotomy, and at reconstruction of the non-union an olecranon reflecting approach was used; the fracture was treated by immobilisation in a splint for three weeks, and union and good function were achieved.
Discussion
Distal humerus non-unions are not frequent and are usually associated with instability, abnormal motion, strength loss, reduction of articular motion, pain and functional loss. Although they are demanding procedures, requiring secondary operations in a high percentage of cases, the treatment of these lesions by detailed preoperative planning, an adequate approach, rigid open reduction and internal fixation together with correct implant selection and placement, and prompt postoperative mobilisation, associated with capsular release and bone graft when necessary, allowed a high rate of bony union and good functional results (Fig. 2). The main limitations of this study are that it is retrospective, it has no control group and that different stabilisation methods were used.
Total elbow replacement has proven effective for the treatment of these lesions, but it is not indicated in young active patients or in patients with a history of infection [4, 13, 16]. The risk of complications such as infection, triceps insufficiency and ulnar neuropraxia is increased when total elbow replacement is performed as a salvage procedure, even more if the patient has a history of infection [17]. Elbow arthrodesis, resection or distraction arthroplasty and the use of joint allografts have yielded disappointing results [3, 25].
An important factor in the development of non-unions at the distal humerus is the initial treatment of the lesion [2]. In our series, X-ray review showed that the initial treatment could be considered inadequate or insufficient in 16 cases according to standard osteosynthesis principles, another six non-unions developed after infection and in the other two cases no technical problems could be identified as the cause of non-union. ROM at last examination in this series is similar to those previously reported in the literature [1, 7, 11, 17]; improvement in elbow articular ROM was 53° (an average of 45° before surgery and an average of 98° at last examination); this significant increase is justified since both elbows with ankylosis improved ROM from 0° before surgery to 110 and 115°, respectively, at the last examination and because of long-term follow-up in our series.
Infected non-unions are associated with marked osteopaenia due to disuse, significant articular contracture, focal bone defects from previous osteosynthesis and avascular or necrotic bone which makes reconstruction even more difficult. Results reported in infected non-unions are significantly worse than those obtained in aseptic non-unions [6]. Careful débridement has to be performed to remove implants and avascular tissues. Later an assessment is made to determine whether the reconstruction will be performed in one or two stages and the type of stabilisation to be used. Vascularised osseous flaps might be a good treatment option for these complex cases [14].
Surgical treatment of distal humerus non-unions is demanding, particularly because it is generally associated with small bone fragments and poor bone quality which hinder the achievement of rigid internal fixation. The advent of new osteosynthesis techniques and materials such as the use of triple plating and locked plates may increase the stability achieved in these lesions [8, 9]. Implants need to be precontoured to allow their adaptation to distal humeral anatomy; and they need to allow for the possibility of being placed to avoid remains of osteosynthesis materials from previous operations. The articular cartilage can regenerate itself once anatomical reduction, stable fixation and early movement are achieved [10, 18, 23], but methods to improve its remodelling are necessary to improve results in intra-articular lesions [24]. Currently, we consider anterior transposition of the ulnar nerve a routine procedure when treating distal humerus non-unions.
Mitsunaga et al. [12] treated 25 elbow non-unions giving priority to achieving union and leaving mobility as a second objective; this led to bony union in only 20 cases (80%) and only 9° improvement in ROM. Elbow stiffness results in abnormal forces as regards intensity and direction at the level of the non-union. Capsular release and arthrolysis in patients with distal humerus non-union and motion limitation due to articular causes improve elbow mobility and reduce implant stress during postoperative mobilisation, thus protecting the stability achieved with the osteosynthesis. In distal humerus non-unions anterior arthrolysis can be performed using a posterior approach, releasing the anterior capsule and retracting soft tissues through the non-union site before reduction and fixation of the lesion.
Screw type, quantity, direction and diameter varied according to the characteristics and location of the non-unions and to the quality of the affected bone; the most distal screw of the plate placed on the medial aspect of the distal humerus is generally placed in the medial column to achieve a tension band effect (Fig. 1b and c). Superficial placement of 4.5-mm plates produces discomfort at the distal end of the humerus; this usually forces their removal after union is achieved. The use of tension bands is particularly useful in patients with osteoporotic bone and small bone fragments, since they allow the reduction of the bone fragment preserving muscle, tendons and ligament origins.
Not all distal humerus non-unions have to be surgically treated either because the disability they produce does not justify surgery, because the patient’s general condition is not good enough or because the patient is not ready to take the risks and compromise offered by the proposed treatment. Surgical treatment of distal humerus non-unions is complex and yields positive results in cases that are well selected, planned and technically executed. The surgeon must be ready to change the preoperative plan according to his findings during surgery in order to provide better stability. It is important to suspect and diagnose all alterations in a fracture consolidation process to avoid complications or to treat them promptly. Distal humerus non-unions present different characteristics; consequently, surgical treatment must be individualised for each patient.
References
- 1.Ackerman G, Jupiter JB. Non-union of fractures of the distal end of the humerus. J Bone Joint Surg Am. 1988;70:75–83. [PubMed] [Google Scholar]
- 2.Ali A, Douglas H, Stanley D. Revision surgery for nonunion after early failure of fixation of fractures of the distal humerus. J Bone Joint Surg Br. 2005;87:1107–1110. doi: 10.1302/0301-620X.87B8.15610. [DOI] [PubMed] [Google Scholar]
- 3.Breen T, Gelberman RH, Leffert R, Botte M. Massive allograft replacement of hemiarticular traumatic defects of the elbow. J Hand Surg [Am] 1988;13:900–907. doi: 10.1016/0363-5023(88)90268-7. [DOI] [PubMed] [Google Scholar]
- 4.Figgie MP, Inglis AE, Mow CS, Figgie HE., 3rd Salvage of non-union of supracondylar fracture of the humerus by total elbow arthroplasty. J Bone Joint Surg Am. 1989;71:1058–1065. [PubMed] [Google Scholar]
- 5.Gallay SH, McKee MD. Operative treatment of nonunions about the elbow. Clin Orthop. 2000;370:87–101. doi: 10.1097/00003086-200001000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Haidukewych GJ, Sperling JW. Results of treatment of infected humeral nonunions: the Mayo Clinic experience. Clin Orthop Relat Res. 2003;414:25–30. doi: 10.1097/01.blo.0000084399.53464.4e. [DOI] [PubMed] [Google Scholar]
- 7.Helfet DL, Kloen P, Anand N, Rosen HS. Open reduction and internal fixation of delayed unions and nonunions of fractures of the distal part of the humerus. J Bone Joint Surg Am. 2003;85-A:33–40. doi: 10.2106/00004623-200301000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Jupiter JB, Goodman IJ. The management of complex distal humerus nonunion in the elderly by elbow capsulectomy, triple plating, and ulnar nerve neurolysis. J Shoulder Elbow Surg. 1992;1:37–46. doi: 10.1016/S1058-2746(09)80015-3. [DOI] [PubMed] [Google Scholar]
- 9.Korner J, Lill H, Muller LP, Rommens PM, Schneider E, Linke B. The LCP-concept in the operative treatment of distal humerus fractures—biological, biomechanical and surgical aspects. Injury. 2003;34(Suppl 2):B20–B30. doi: 10.1016/j.injury.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 10.Llinas A, McKellop HA, Marshall GJ, Sharpe F, Kirchen M, Sarmiento A. Healing and remodeling of articular incongruities in a rabbit fracture model. J Bone Joint Surg Am. 1993;75:1508–1523. doi: 10.2106/00004623-199310000-00012. [DOI] [PubMed] [Google Scholar]
- 11.McKee M, Jupiter J, Toh CL, Wilson L, Colton C, Karras KK. Reconstruction after malunion and nonunion of intra-articular fractures of the distal humerus. Methods and results in 13 adults. J Bone Joint Surg Br. 1994;76:614–621. [PubMed] [Google Scholar]
- 12.Mitsunaga MM, Bryan RS, Linscheid RL. Condylar nonunions of the elbow. J Trauma. 1982;22:787–791. doi: 10.1097/00005373-198209000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Morrey BF, Adams RA. Semiconstrained elbow replacement for distal humerus nonunion. J Bone Joint Surg Br. 1995;77:67–72. [PubMed] [Google Scholar]
- 14.Mullett H, Hausman M, Zaidemberg C. Recalcitrant distal humeral and proximal forearm nonunion: salvage using an extended pedicled radial forearm osseous flap. J Trauma. 2008;64:E60–E64. doi: 10.1097/01.ta.0000229713.56091.5b. [DOI] [PubMed] [Google Scholar]
- 15.Pelissier P, Masquelet AC, Bareille R, Pelissier SM, Amedee J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthop Res. 2004;22:73–79. doi: 10.1016/S0736-0266(03)00165-7. [DOI] [PubMed] [Google Scholar]
- 16.Ramsey ML, Adams RA, Morrey BF. Instability of the elbow treated with semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 1999;81:38–47. doi: 10.2106/00004623-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Ring D, Gulotta L, Jupiter JB. Unstable nonunions of the distal part of the humerus. J Bone Joint Surg Am. 2003;85-A:1040–1046. doi: 10.2106/00004623-200306000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Salter RB, Simmonds DF, Malcolm BW, et al. The biological effect of continuous passive motion on the healing of full-thickness defects in articular cartilage. An experimental investigation in the rabbit. J Bone Joint Surg Am. 1980;62:1232–1251. [PubMed] [Google Scholar]
- 19.Sanders RA, Sackett JR. Open reduction and internal fixation of delayed union and nonunion of the distal humerus. J Orthop Trauma. 1990;4:254–259. doi: 10.1097/00005131-199004030-00003. [DOI] [PubMed] [Google Scholar]
- 20.Schatzker J. Intraarticular malunions and nonunions. Orthop Clin North Am. 1990;21:743–757. [PubMed] [Google Scholar]
- 21.Sim FH, Morrey BF. Non-union and delayed union of distal humeral fractures. In: Morrey BF, editor. The elbow and its disorders. 3. Philadelphia: Saunders; 2000. pp. 331–340. [Google Scholar]
- 22.Simonis RB, Nuñez VA, Khaleel A. Use of the Coventry infant hip screw in the treatment of nonunion of fractures of the distal humerus. J Bone Joint Surg Br. 2003;85:74–77. doi: 10.1302/0301-620X.85B1.12953. [DOI] [PubMed] [Google Scholar]
- 23.Trumble T, Allan CH, Miyano J, Clark JM, Ott S, Jones DE, Fernacola P, Magnusson M, Tencer A. A preliminary study of joint surface changes after an intraarticular fracture: a sheep model of a tibia fracture with weight bearing after internal fixation. J Orthop Trauma. 2001;15:326–332. doi: 10.1097/00005131-200106000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Trumble T, Verheyden J. Remodeling of articular defects in an animal model. Clin Orthop Relat Res. 2004;423:59–63. doi: 10.1097/01.blo.0000132625.05916.48. [DOI] [PubMed] [Google Scholar]
- 25.Urbaniak JR, Aitken M. Clinical use of bone allografts in the elbow. Orthop Clin North Am. 1987;18:311–321. [PubMed] [Google Scholar]