Abstract
The results of operative treatment of two groups of patients with articular fractures of the calcaneus were evaluated. Twenty-three cases were treated surgically using a standard reconstruction procedure. In the second group of 19 patients a large bone distractor was used; it held the soft tissue flap retracted, while aiding in articular and tuberosity fragment reduction and increasing visualisation by distraction of the posterior talocalcaneal joint. After a year, the anatomical and functional results, together with the operative time, were evaluated. All fractures healed with good or very good anatomical results. All cases, except those with complications (n = 3), achieved good (n = 28) or very good (n = 11) functional scoring. The distractor group had significantly shorter operative times, and less manpower was needed during surgery. We conclude that the large bone distractor is a useful tool in open reconstruction of articular calcaneal fractures.
Introduction
Current descriptions of the operative technique used for the treatment of articular calcaneal fractures suggest the use of Kirschner wires (K-wires) for the retraction of the lateral soft tissue flap [1, 4, 8, 13, 16, 17, 23]. This method, while effective, relatively atraumatic and comfortable for the assistants, leaves poor visualisation of the posterior talocalcaneal joint. With this standard method, additional problems with manipulation and reduction of the calcaneal body and tuberosity may be difficult. We report on important features of the large bone distractor (LBD) used intraoperatively to overcome the above-mentioned drawbacks of the standard operative protocol. This aim is fulfilled by prospective evaluation and comparison of the results of treatment in a group of consecutive patients operated upon using the LBD with a similar group of patients treated by the standard technique.
Materials and methods
Patients involved in this study sustained comminuted fractures of the calcaneus (types II and III according to Sanders classification system) [21]. The average age was 46 years (range 18–60), with no preexisting musculoskeletal or mental disorders, and all signed an informed consent declaration. Exclusion criteria included: open fractures, diabetes, smoking, arterial insufficiency of the involved limb and local skin conditions, severe injury to the central nervous system (GCS<9, spinal cord injury, paraplegia) and bilateral fractures. Although we did operate on selected patients matching the exclusion criteria (bilateral fractures, injuries to the central nervous system), we were not able to use the same evaluation protocol as in the groups involved in the study.
Between 2002 and 2005, 23 consecutive patients matching the criteria listed above (four females and 19 males) were treated by the standard technique and formed the first group (see Table 1). In the Department of Trauma, Burns and Plastic Surgery of Poznan University of Medical Sciences, patients qualified for open reconstruction of comminuted articular calcaneal fractures were operated upon through the extended lateral approach after exsanguination of the affected limb and a single dose, wide spectrum antibiotic prophylaxis. Reduction and fixation of the posterior articular surface (PAS) was performed first with a lag screw, then the extrarticular anatomy was restored and fragments fixed using a low profile reconstruction plate and screws (Synthes/Stratec Medical, Switzerland). No bone grafts or postoperative suction drainage were used.
Table 1.
Results of treatment in the standard protocol group
| Sex, age (y) | Fracture type (Sanders classification) | Anatomic result | Functional result | Time to PAS fixation (minutes) | Complications |
|---|---|---|---|---|---|
| M, 46 | II | Good | Good | 40 | |
| M, 26 | II | Good | Satisfactory | 32 | C |
| M, 57 | II | Very good | Good | 30 | C |
| F, 59 | II | Good | Good | 40 | |
| F, 19 | III | Good | Good | 33 | C |
| M, 33 | II | Very good | Very good | 14 | |
| M, 48 | III | Very good | Dobry | 29 | |
| F, 32 | II | Very good | Dobry | 25 | |
| M, 44 | II | Very good | Very good | 17 | |
| M, 25 | III | Good | Good | 38 | C |
| M, 22 | II | Very good | Good | 19 | |
| M, 52 | III | Very good | Very good | 32 | |
| M, 34 | III | Good | Very good | 33 | |
| M, 29 | III | Good | Good | 30 | |
| M, 57 | III | Good | Satisfactory | 36 | C, I |
| M, 48 | II | Very good | Good | 20 | |
| M, 39 | II | Very good | Very good | 22 | |
| M, 33 | II | Good | Good | 19 | |
| F, 37 | III | Very good | Good | 29 | C |
| M, 50 | II | Very good | Good | 20 | C |
| M, 31 | III | Good | Good | 30 | |
| M, 50 | III | Good | Good | 32 | |
| M, 26 | III | Good | Good | 28 |
M male, F female, PAS posterior articular surface, C toe contracture, I infection
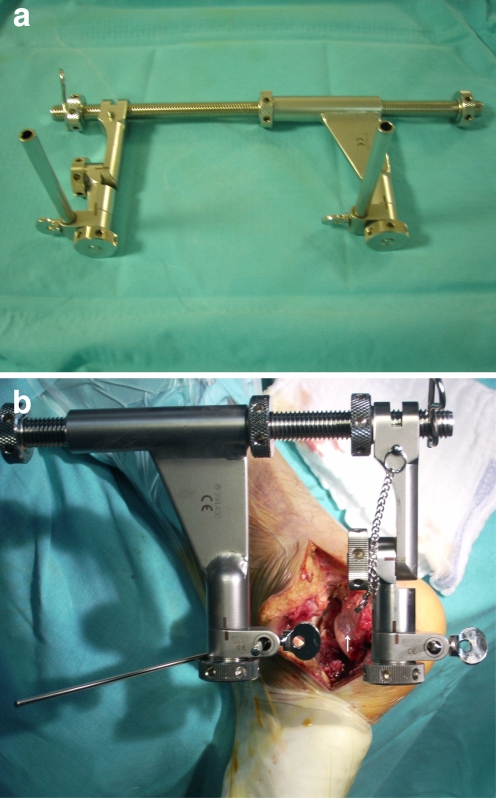
The second group was formed of 19 consecutive patients (four females and 15 males) treated during the 13 month period between August 2005 and June 2006 (see Table 2). For operative calcaneal reconstruction, the LBD was used (Fig. 1a).
Table 2.
Results of treatment in the large bone distractor (LBD) group
| Sex, age (y) | Fracture type (Sanders classification) | Anatomic result | Functional result | Time to PAS fixation (minutes) | Complications |
|---|---|---|---|---|---|
| M, 26 | II | Good | Good | 39 | C |
| M, 57 | II | Very good | Good | 35 | C |
| F, 59 | II | Good | Very good | 30 | |
| F, 19 | III | Good | Good | 42 | C |
| M, 33 | II | Very good | Very good | 11 | |
| M, 48 | III | Good | Good | 31 | |
| F, 32 | II | Very good | Good | 19 | |
| M, 44 | II | Very good | Very good | 21 | |
| M, 22 | II | Very good | Very good | 14 | |
| M, 52 | III | Very good | Good | 19 | |
| M, 34 | III | Good | Good | 20 | |
| M, 29 | III | Good | Good | 34 | |
| M, 57 | III | Good | Satisfactory | 20 | C, I |
| M, 48 | II | Very good | Good | 16 | |
| M, 39 | II | Very good | Very good | 15 | |
| M, 33 | II | Good | Good | 12 | |
| F, 37 | III | Very good | Very good | 22 | |
| M, 50 | II | Very good | Good | 12 | C |
| M, 31 | III | Good | Good | 18 |
M male, F female, PAS posterior articular surface, C toe contracture, I infection
Fig. 1.
a Large bone distractor. b The large bone distractor (LBD) in articular calcaneal fracture. Depressed and rotated anteriorly (white arrow), the lateral part of the posterior articular surface is visible
The preoperative evaluation was based on lateral radiograph. When articular fracture was suspected, computed tomography was performed and PAS injury was described using the Sanders classification system. The operative intervention was performed after skin wrinkling and healing of epidermal blisters was noted (6–18 days after injury, mean 11 days). After the operation, no additional immobilisation was used and patients were encouraged to perform full range, pain free exercises of the ankle joint. The results were evaluated by the senior author in a prospective, non blinded fashion. None of the patients included in the study groups were lost to follow-up.
Lateral and Broden views were obtained immediately after the operation and again after six weeks (when a decision on partial weight bearing was made), 12 weeks and finally after a year. The quality of reduction was evaluated on the following grounds: (1) restoration of PST anatomy (Broden radiographic view) such that very good results include a smooth articular surface, a good result is step-off 1–2 mm, and a bad result is step-off exceeding 2 mm and (2) Böhlers angle (lateral radiographic view) in which a very good result occurs when the angle is comparable to the unaffected side in the range ±10 degrees, a good result is if the difference does not exceed ±20 degrees, and the rest are graded as bad.
The functional results were evaluated with the Creighton-Nebraska Health Foundation Assessment Score for Fractures of the Calcaneus, a year after the operation [6]. Special attention was paid to the presence of complications, mainly toe contractures and infection.
Time from exposure of the lateral wall of the calcaneus to definitive fixation of the articular fragments with a lag screw was compared in both groups.
The only difference between the two groups was the intraoperative use of LBD. Both 4.5-mm Steinmann pins (S-pin) were introduced obliquely, about 30 degrees off the horizontal plane, one into the talus and the other into the tuberosity of the calcaneus. The distractor’s upper S-pin acts as a retractor for the lateral soft tissue flap (instead of K-wires in the standard technique). The lower not only disimpacts the tuberosity fragment and corrects the typical calcaneal shortening, but also may reduce the common varus deformity if introduced obliquely in the frontal plane at an appropriate angle. It additionally retracts soft tissues of the posterior calcaneus. In the standard protocol group, one 4.5-mm S-pin introduced into the tuberosity was used as a “joystick” for bony manipulation.
After the LBD is in place, distraction is carried out until the calcaneal fragments become disimpacted and the width of articular space of the posterior talocalcaneal joint (PTC) reaches 7–10 mm. The range of distraction is dependent on the subjective feeling of distraction screw resistance. At this moment the two S-pins become parallel, leading to slight external rotation of the talus, giving more space at the lateral aspect of the PTC (Fig. 1b).
Results
The anatomical and functional results in the standard protocol group a year after operative intervention are presented in Table 1. The anatomical and functional results in the LBD group a year after operative intervention are presented in Table 2. Anatomical result was rated good and very good in all patients from both groups. Function was rated good or very good in 39 of 42 cases. The only three satisfactory functional outcomes were detected in patients with complications. The mean fixation time for the standard protocol group was 28 minutes (range 14–42), while for the distractor group it averaged 22 minutes (range 11–42).
Statistical analysis
No correlation was found between the fracture type and sex, though articular calcaneal fractures were more common in males (34:8). A significant relation exists between the fracture type and anatomical result obtained (p = 0.00527, Pearson’s chi2 test). In both groups, fractures classified as type II ended up with very good anatomical results in 16 cases, while in type III fractures only in five. No correlation of functional result and the fracture type was found, though the function at one year was significantly related to the anatomical result (p = 0.0113, Fisher–Freeman–Halton test). Only nine cases with very good anatomical result ended up with very good function, while in patients with just good restoration of anatomy only two had their function rated very good.
The number of toe contractures was not related to fracture type (n = 6 in type II fractures and n = 6 in type III). No difference in mean patient’s age between type II and III fractures was observed. The mean fixation time was significantly (p = 0.0143, Student t-test) reduced in the type II fractures (22.7 minutes) compared to type III (29.3 minutes).
No influence of the use of LBD on anatomical or functional results and the number of toe contractures was detected. However, the distractor significantly (p = 0.0411, Student t-test) reduced mean PAS fixation time, such that for the control group it was 28.2 minutes and for the LBD group 22.6 minutes.
Discussion
We used standard inclusion criteria for the patients, operative approach and anatomical goal of the procedure [1, 4, 5, 10, 18, 20, 25]. Our results also meet the international standards [4, 6, 16, 18, 25]. Among authors using the Creighton-Nebraska system, Crosby and Fitzgibbons report of 50% very good and 30% good outcomes, while Monsey et al. had 30% very good and 26% good results in an homogenous group of patients with Sanders type II fractures [6, 18]. In cases with type III fractures Monsey et al. reports of 22% very good and 22% good results [18].
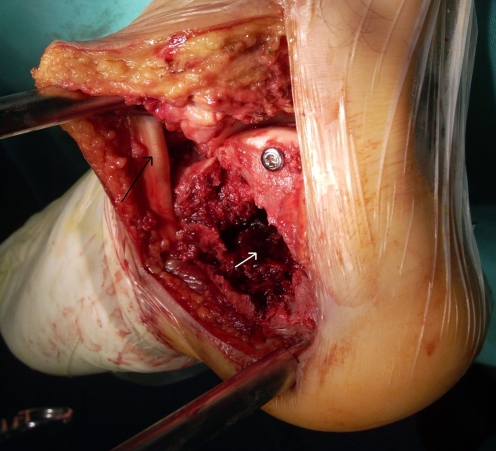
Abandoning bone grafting of the defect of the calcaneal body did not lead to deterioration of the anatomical result (Fig. 2). Tufescu and Buckley compared patient groups treated with and without bone grafting. They were unable to prove any radiological or functional differences between them [24]. This fact might be associated with minimal physiological loading of the neutral triangle, the location most severely affected with post injury bone loss [1, 12] (Fig. 2). In a study from the Netherlands, Schepers et al. report bone grafting being used by 20% of surgeons in that country, 42% used them occasionally and 38% admitted to not using them [22]. Some use resorbable bone cement in cases of significant defects [11].
Fig. 2.
The calcaneus distracted with the large bone distractor (LBD), the posterior talocalcaneal joint (PAS) reduced and fixed with a lag screw. Visible defect in the body of the calcaneus (white arrow) with the neutral triangle most severely affected. The black arrow shows the upper S-pin and retracted peroneal tendons
It is widely believed that restoration of normal anatomy is a good prognostic factor for the future function of the extremity. Our results suggest that a good anatomical reduction will not necessarily provide a good restoration of function. Similar conclusions of other studies relate this problem to injuries of soft tissues adjacent to the calcaneus, thus emphasising the role of high energy transfers and also to the socioeconomic status of the patient [3, 4, 9].
A poor result is usually manifested by pain in the subtalar region and often necessitates corrective osteotomies or arthrodesis [7, 22]. In the Netherlands, this concerns 21% of patients, while in the United States 16% of patients treated initially nonoperatively and 3% after failed reconstruction are subjected to arthrodesis [4, 7, 22].
Early, significant foot oedema, often with concomitant skin problems (blisters, ecchymoses) inclines the surgeon to consider fasciotomy. In all patients from this group, direct measurement of pressure in three hind foot compartments was performed. Despite marked elevation of pressures, we did not detect other early clinical symptoms of compartment syndrome; thus, fasciotomies were not performed [14]. Other authors report of varying frequency of such procedures—from 0% to 20%. It is believed that, in about 10% of patients, fractures of the calcaneus lead to increased pressure in the facial compartments and to later fibrosis resulting in toe contractures [4, 19]. In our group, such problems occurred in 12 cases and in none of these late function was very good. Due to these soft tissue complications of our protocol we should use fasciotomies in the future more aggressively.
Another important finding is that there were few wound complications, though we did not use postoperative suction drainage. We use such protocol to reduce the typical problems with wound closure [4]. Avoidance of suction drainage did not increase the complication rate.
Infection is the most catastrophic sequel of open calcaneal reconstruction [2, 3, 17]. In our material, the number of infectious complications (n = 2) compares favourably with numbers reported by others. Zwipp found 6.7% with superficial wound problems and osteomyelitis in 2.2% [25]. Similarly, in the Netherlands, 16% had superficial problems and 2% had deep infections [22]. Buckley et al. report of 5% infection rate in a group of 400 patients [4].
The rate of infection is kept low due to strict inclusion criteria (contraindication in smokers, diabetics and patients with peripheral vascular disease), antibiotic prophylaxis, delayed intervention (skin wrinkling) and delicate manipulation of the lateral soft tissue flap.
In cases of deep infections with typical soft tissue defect, there are few options for wound coverage [4, 17]. One of our two cases healed a month after removal of implants, debridement, local wound care and systemic antibiotic therapy. The other required additional bone resection with initial local use of the Gentamycin sponge (Garamycin Schwamme) and later use of the vacuum technique (VAC).
Modification of the standard operative technique by the use of LBD eliminates K-wires for retraction of the soft tissue flap from the lateral calcaneal surface, allows wide distraction of the posterior talocalcaneal joint, and leads to disimpaction and reduction of the calcaneal tuberosity, simultaneously reducing the need for additional assistants. Calcaneal reconstruction can be performed with the assistance of a scrub nurse only, although this technique is less laborious and more effective. Such an intraoperative impression is supported by significantly shorter operative time in the LBD group of patients. The learning curve might be another factor that caused shortening of the procedure, since the LBD group was treated after the standard group.
Reports of the use of such a device for the treatment of articular fractures of the calcaneus are not available in the Medline database. We have found studies presenting the use of LBD in subtalar arthrodesis for complications of calcaneal fractures and in arthroscopy of the ankle joint [5, 15].
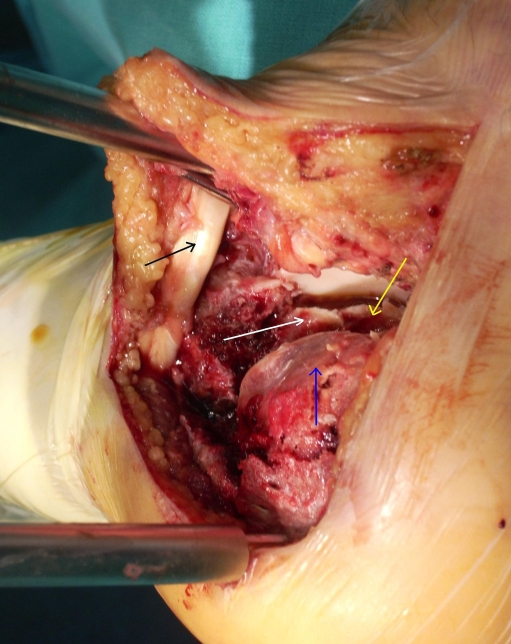
The LBD distracts the PTC to 6–8 mm in its lateral aspect, gradually decreasing medially (Fig. 3). Good visualisation of the PTC limits the need for intraoperative fluoroscopy. We have not used it in any of these cases. Instead, we expose the space between the posterior talus and Achilles tendon gaining view of the posterior aspect of PAS and the possibility of digital control of the medial wall.
Fig. 3.
Calcaneal fracture, Sanders type III. PTC distraction with the use of LBD. Black arrow points out the peroneal tendons. Deep inside the joint, a yellow arrow points to the undislocated anteromedial articular fragment. The mid portion of PAS is marked with a white arrow. The depressed and anteriorly rotated lateral fragment is shown by a blue arrow
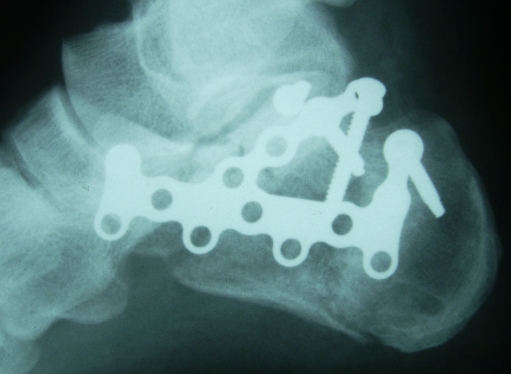
An important technical detail is the necessity of LBD dissembling (the S-pins stay) after reduction and fixation of the PAS with the tuberosity fragment. If left in place, reduction of the Gissane angle with the anterior process of the calcaneus is impossible (Fig. 4).
Fig. 4.
Calcaneal fracture, Sanders type III (patient from Fig. 3). Very good anatomic result
We have found that comparing the functional results among the two groups of patients is useless because the modified operative technique should not translate to different outcomes if the anatomical results were similar. However, we will continue to track these results to find out whether function is improving or deteriorating with longer observation time.
Having no control group, with the same fracture type but treated nonoperatively, might be considered another bias of this study. For ethical reasons, formation of such a group from patients believed to benefit from operative reconstruction is impossible. Additionally, comparing the results of operative and nonoperative management was not our goal.
Conclusions
Despite the fairly low statistical power of this consecutive cohort series study following a small number of patients, certain conclusions can be drawn.
An appropriately inserted large femoral distractor is very useful in open reconstruction of articular calcaneal fractures via the extended lateral approach.
Operative reconstruction of articular calcaneal fractures should result in a high rate of good and very good anatomical and mid term functional outcome.
Operative reconstruction of normal calcaneal anatomy is a good prognostic factor for restoration of normal function of the lower limb.
Articular calcaneal fractures are three times more frequent in males than females.
Anatomical results of operative reconstruction of articular calcaneal fractures are dependent on the amount of articular involvement in the range II/III of Sanders classification.
References
- 1.Barei DP, Bellabarba C, Sangeorzan BJ, et al. Fractures of the calcaneus. Orthop Clin North Am. 2002;33(1):263–285. doi: 10.1016/S0030-5898(03)00084-1. [DOI] [PubMed] [Google Scholar]
- 2.Bernstain SA. Late sequelae of calcaneal fractures. Clin Podiatric Med Surg. 2000;17(1):81–95. [PubMed] [Google Scholar]
- 3.Bondi R, Padua R, Bondi L, et al. Treatment of calcaneal fractures: the available evidence. J Orthopaed Traumatol. 2007;8:36–41. doi: 10.1007/s10195-007-0160-2. [DOI] [Google Scholar]
- 4.Buckley R, Tough S, McCormack R, et al. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures. J Bone Joint Surg [Am] 2002;84-A:1733–1744. doi: 10.2106/00004623-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Burton DC, Olney BW, Horton GA. Late results of subtalar distraction fusion. Foot Ankle Int. 1998;19(4):197–202. doi: 10.1177/107110079801900402. [DOI] [PubMed] [Google Scholar]
- 6.Crosby LA, Fitzgibbons TC. Open reduction and internal fixation of type II intra-articular calcaneus fractures. Foot Ankle Int. 1996;17(5):253–258. doi: 10.1177/107110079601700503. [DOI] [PubMed] [Google Scholar]
- 7.Csizy M, Buckley R, Tough S, et al. Displaced intra-articular calcaneal fractures. Variables predicting late subtalar fusion. J Orthop Trauma. 2003;17(2):106–112. doi: 10.1097/00005131-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Grala P, Mańkowski B, Machyńska-Bućko Z. Complications of dislocated calcaneal fractures. Ortop Traum Rehab. 2007;9(2):198–205. [PubMed] [Google Scholar]
- 9.Hammesfahr JF. Surgical treatment of calcaneal fractures. Orthop Clin North Am. 1989;20:679–689. [PubMed] [Google Scholar]
- 10.Howard JL, Buckley R, McCormack R, et al. Complications following management of displaced intra-articular calcaneal fractures: a prospective randomized trial comparing open reduction internal fixation with nonoperative management. J Orthop Trauma. 2003;17:241–249. doi: 10.1097/00005131-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Huber FX, Hillmeier J, McArthur N, et al. The use of nanocrystalline hydroxyapatite for the reconstruction of calcaneal fractures: preliminary results. J Foot Ankle Surg. 2006;45(5):322–328. doi: 10.1053/j.jfas.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Hutchinson F, Huebner MK. Treatment of os calcis fractures by open reduction and internal fixation. Foot Ankle Int. 1994;15:225–229. doi: 10.1177/107110079401500501. [DOI] [PubMed] [Google Scholar]
- 13.Juliano P, Ngujen H. Fractures of the calcaneus. Orthop Clin North Am. 2001;32(1):35–51. doi: 10.1016/S0030-5898(05)70192-9. [DOI] [PubMed] [Google Scholar]
- 14.Kierzynka G, Grala P. Compartment syndrome of the foot after calcaneal fractures. Ortop Traumatol Rehabil. 2008;10(4):377–383. [PubMed] [Google Scholar]
- 15.Kumar VP, Satku K. The A-O femoral distractor for ankle arthroscopy. Arthroscopy. 1994;10(1):118–119. doi: 10.1016/S0749-8063(05)80305-6. [DOI] [PubMed] [Google Scholar]
- 16.Letournel E. Open treatment of acute calcaneal fractures. Clin Orthop. 1993;290:60–67. [PubMed] [Google Scholar]
- 17.Lim EVA, Leung JPF. Complications of intraarticular calcaneal fractures. Clin Orthop. 2001;391:7–16. doi: 10.1097/00003086-200110000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Monsey RD, Levine BP, Trevino SG, et al. Operative treatment of acute displaced intraarticular calcaneus fractures. Foot Ankle Int. 1995;16(2):57–63. doi: 10.1177/107110079501600201. [DOI] [PubMed] [Google Scholar]
- 19.Myerson MS, Manoli A. Compartment syndromes of the foot after calcaneal fractures. Clin Orthop. 1993;290:142–150. [PubMed] [Google Scholar]
- 20.O’Farrel DA, O’Byrne JM, McCabe JP, et al. Fractures of the os calcis: improved results with internal fixation. Injury. 1993;24:263–265. doi: 10.1016/0020-1383(93)90183-7. [DOI] [PubMed] [Google Scholar]
- 21.Sanders R, Fortin P, DiPasquale T, et al. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop. 1993;290:87–95. [PubMed] [Google Scholar]
- 22.Schepers T, Lieshout EMM, Ginhoven TM, et al. Current concepts in the treatment of intra-articular calcaneal fractures: results of a nationwide survey. Int Orthop. 2008;32(5):711–715. doi: 10.1007/s00264-007-0385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Souza LJ, Rutledge E. Grouping of intraarticular calcaneal fractures relative to treatment options. Clin Orthop. 2004;420:261–267. doi: 10.1097/00003086-200403000-00037. [DOI] [PubMed] [Google Scholar]
- 24.Tufescu TV, Buckley R. Age, gender, work capability, and worker’s compensation in patients with displaced intraarticular calcaneal fractures. J Orthop Trauma. 2001;15:275–279. doi: 10.1097/00005131-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Zwipp H, Tscherne H, Thermann H, et al. Osteosynthesis of displaced intraarticular fractures of the calcaneus. Clin Orthop. 1993;290:76–86. [PubMed] [Google Scholar]