Abstract
The measurement of joint motion is common practice in many aspects of orthopaedic surgery. A number of techniques and instruments have been developed for this purpose. We describe a method of recording and measuring knee joint motion using digital imaging which demonstrated high inter-observer reliability (r > 0.948) and intra-observer repeatability (r > 0.906). This technique may offer some practical advantages over other methods of measuring joint motion.
Résumé
La mesure de la mobilité articulaire est une pratique habituelle en chirurgie orthopédique. De nombreux instruments peuvent être développés. Nous décrivons une méthode de la mesure de la mobilité en utilisant une imagerie digitalisée. Ces techniques montrent une importante sensibilité inter-observateur (r > 0,948) et intra observateur avec une bonne répétabilité (r > 0,906). En conclusion, cette technique est fiable, répétitive et suffisamment sure offrant un certain nombre d'avantages pratiques.
Introduction
Goniometry is defined as the use of instruments to measure joint motion. A variety of instruments and techniques have been developed for measuring joint motion, each with their advantages and limitations [8]. Range of knee joint motion is generally assessed either visually or with a hand-held goniometer. Plain radiographs have been used to measure preoperative and postoperative knee flexion in research studies [8], whilst computer-assisted navigation has been recently used to analyse range of knee motion during surgery [1]. Employing the same technique to measure range of motion between different time-points rather than a variety of techniques has been advised [8].
Digital imaging has rapidly evolved from the first in-depth trials [4] to provide an efficient means of data documentation [14]. Surgical specialties such as urology [13], vascular surgery [22], plastic and reconstructive surgery [10], orthodontics [12], and neurosurgery [17] have all reported the use of digital imaging in patient care. The practice of digital imaging to record and document patient conditions has become more common in orthopaedic practice [19]. However, the use of digital image analysis to quantify range of joint motion has not previously been reported. We describe a reliable and repeatable method of measuring range of knee motion using digital imaging. The advantages and disadvantages of this method to measure knee joint motion in relation to other techniques are discussed.
Joint movement is generally reduced to a description of relative motion between two rigid members attached at a joint. Various models have been used to describe knee joint motion including one, two, three, and six degrees of freedom models [5]. Knee joint motion measured using goniometery is dependent on accurate alignment of the arms of the device between bony landmarks such as the lateral epicondyle, greater trochanter, and lateral malleolus. The goniometer is centred on the lateral epicondyle and pointed towards the greater trochanter and lateral epicondyle, with the knee considered as a hinge joint with one degree of freedom. This study presents a three degrees of freedom model to measure knee motion in the sagittal plane using two-dimensional digital images.
Patients and methods
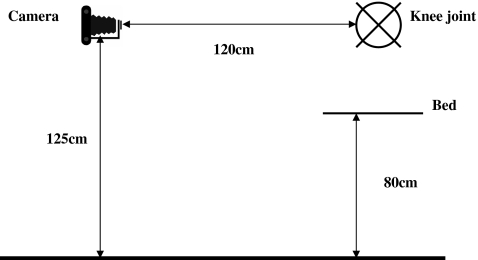
Reliability and repeatability testing
Following local ethical committee approval, ten patients (seven females, three males) presenting to the senior author for knee replacement surgery were recruited for this part of the study. The subject was placed on a bed 80 cm above floor level with their lower limb positioned parallel to the edge of the bed. A digital camera (Finepix 2400, Fuji, Tokyo, Japan) mounted on a tripod 125 cm above floor level was positioned 120 cm from the subject’s limb (Fig. 1). The camera and tripod were positioned and maintained at 90 degrees to the long axis of the bed. The set-up protocol was standardised for all images taken using the ten subjects.
Fig. 1.
Schematic of digital camera and patient positioning
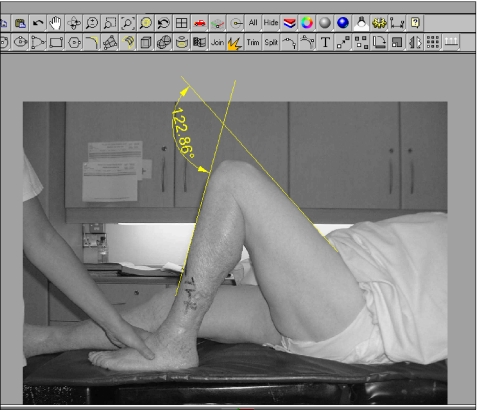
Digital images were recorded for each subject with the limb in four positions—active extension, passive maximum extension, active flexion, and passive maximum flexion (Fig. 2). Angular measurements were made to the nearest degree using image analysis software (Rhinoceros, Seattle, WA, USA) based on superimposed lines parallel to the anterior thigh and anterior tibia (Fig. 3).
Fig. 2.
Passive maximum flexion
Fig. 3.
Angular measurement using image analysis software
For the purpose of determining inter-observer reliability, two observers from different disciplines (a physiotherapist and an orthopaedic registrar) independently measured each of the 40 images. Both observers were given the same sheet of instructions outlining in detail the method for measuring the digital images. Inter-observer reliability was evaluated using Pearson product–moment correlation coefficients.
In order to assess repeatability, the four sets of digital images for the ten subjects were measured by a single observer on three different occasions with the observer being blinded to the results obtained from the previous measurements. Repeatability was evaluated using analysis of variance (ANOVA) and intra-class correlation coefficients (ICC).
Accuracy testing
In this part of the study, the effect of camera or limb mal-positioning was investigated. A prosthetic limb (Fig. 4) was positioned first in almost full extension and then in flexion. A digital image was taken in each position using the set-up as described above and the knee angle measured to provide a baseline measurement. The reference measurements for each position were 16 and 95 degrees of flexion, respectively.
Fig. 4.
Prosthetic limb used in accuracy testing
Using the same set-up as above, digital images were recorded with the prosthetic limb in positions of 15 and 30 degrees of abduction and adduction. The camera position remained constant for each image. Digital images were then recorded with the camera rotated 15, 30, and 45 degrees in a clockwise and an anti-clockwise direction. The position of the prosthetic limb remained constant for each image. Errors were recorded as the difference between the reference measurements of the prosthetic limb and the measurements observed under the simulated conditions.
Results
Reliability and repeatability testing
Testing revealed a mean difference between measurements of the two independent observers of 1.8 degrees (range 0–5 degrees). These mean differences ranged from 1.1 degrees for active extension to 2.4 degrees for passive extension (Table 1). The Pearson product–moment correlation coefficient for each of the knee positions examined was at least 0.948, implying a high degree of agreement between the measurements of the two observers (Table 1). Intra-observer repeatability testing revealed intra-class correlation coefficients (ICC) of at least 0.906 for all knee positions (Table 2). The standard deviation of error of the measurements was between 0.9 and 1.9 degrees (Table 2). The mean difference in measurements by the single observer over three assessments was 1.3 degrees, ranging from 1.0 degrees for active flexion to 2.0 degrees for active extension (Table 2). For all the parameters measured, the measurement error variation was very small compared to the variation in the absolute measures of these parameters.
Table 1.
Inter-observer reliability testing for various knee positions
| Knee position | Pearson’s correlation coefficient | Mean difference between observers (degrees) |
|---|---|---|
| Active extension | 0.995 | 1.1 |
| Passive extension | 0.948 | 2.4 |
| Active flexion | 0.993 | 1.9 |
| Passive flexion | 0.993 | 1.8 |
Table 2.
Intra-observer repeatability
| Knee position | Interclass correlation coefficient | Standard deviation of error (degrees) | Mean difference in measurements (degrees) |
|---|---|---|---|
| Active extension | 0.906 | 1.9 | 2.0 |
| Passive extension | 0.955 | 1.3 | 1.4 |
| Active flexion | 0.995 | 1.1 | 1.0 |
| Passive flexion | 0.996 | 0.9 | 0.9 |
Accuracy testing
The results of the accuracy tests are summarised in Table 3. With the knee in extension, an error of 2 degrees or less was recorded in all the simulated positions of abduction and adduction. With the knee in flexion an error of 5 degrees or less was recorded for positions of 15 degrees abduction and adduction, while an error of 10 degrees was recorded for positions of 30 degrees abduction and adduction.
Table 3.
Accuracy of digital image measurements under simulated limb and camera mal-positioning
| Knee flexion/extension | Simulated limb (L) or camera (C) position | Difference between true knee flexion/extension and measured flexion/extension |
|---|---|---|
| 16° knee extension | 15° abduction (L) | 2 |
| 16° knee extension | 30° abduction (L) | 1 |
| 96° knee flexion | 15° abduction (L) | 1 |
| 96° knee flexion | 30° abduction (L) | 10 |
| 16° knee extension | 15° adduction (L) | 1 |
| 16° knee extension | 30° adduction (L) | 0 |
| 96° knee flexion | 15° adduction (L) | 5 |
| 96° knee flexion | 30° adduction (L) | 10 |
| 16° knee extension | 15° clockwise (C) | 1 |
| 16° knee extension | 30° clockwise (C) | 1 |
| 16° knee extension | 45° clockwise (C) | 6 |
| 96° knee flexion | 15° clockwise (C) | 3 |
| 96° knee flexion | 30° clockwise (C) | 5 |
| 96° knee flexion | 45° clockwise (C) | 14 |
| 16° knee extension | 15° anti-clockwise (C) | 0 |
| 16° knee extension | 30° anti- clockwise (C) | 2 |
| 16° knee extension | 45° anti- clockwise(C) | 8 |
| 96° knee flexion | 15° anti- clockwise (C) | 3 |
| 96° knee flexion | 30° anti- clockwise (C) | 14 |
| 96° knee flexion | 45° anti- clockwise (C) | 28 |
For both flexion and extension, camera mal-positioning of 15 degrees rotation produced 3 degrees or less of error. Camera mal-positioning of 30 degrees rotation produced an error of 2 degrees or less with the knee in extension and an error of 14 degrees or less with the knee in flexion. Camera mal-positioning of 45 degrees rotation produced an error of 8 degrees or less with the knee in extension and an error of 28 degrees or less in flexion (Table 3).
Discussion
The measurement of joint motion is an important parameter in clinical practice and is a useful measure of outcome following either surgical intervention or a period of physical therapy. A variety of instruments have been developed for measuring joint motion, but that which is most commonly used is the hand-held goniometer, which has been employed since the early 1900s [15, 18]. The hand-held goniometer relies on the identification of bony anatomical landmarks to act as reference points, for example, the greater trochanter, the lateral femoral epicondyle, and the lateral malleolus. Goniometric measurements are usually made by placing the axis of the goniometer at the epicondylar mark with the arms pointing towards the greater trochanter and the lateral malleolus. The arc of motion is then measured directly from the protractor of the goniometer. In some studies, bony landmarks are not used and the mid-line or long axis of the thigh and tibia are simply visualised for alignment [2].
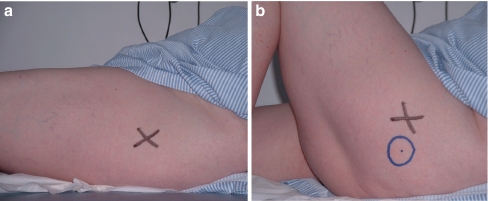
Despite the simplicity and minimal cost, the accuracy of knee measurements obtained using a hand-held goniometer is dependent on the accurate alignment of the arms of the device between bony landmarks, which are often visualised rather than marked [8]. Palpation of bony landmarks around the hip and knee regions can prove difficult in obese patients. Furthermore, movement of the overlying skin may alter the position of the bony landmark. For example, when moving from extension to flexion there is significant movement of the skin over the greater trochcanter as is shown in Fig. 5. Thus, re-palpation of the bony landmarks and re-positioning of the goniometer between the extended and flexed positions are important in order to minimise measurement error. Both goniometer alignment and landmark identification have been shown to contribute to measurement error in previous studies [9].
Fig. 5.
a, b Digital images demonstrating the effect of skin marker movement during typical range of flexion and extension movements. The greater trochcanter skin marker (marker X) with the knee in extension (a). The new greater trochcanter skin marker (marker O) with the knee in flexion and the original marker (marker X) with the knee in extension (b)
Traditionally, knee range of motion measured using a goniometer uses the landmarks of knee joint centre, greater trochanter, and lateral malleolus and employs a simple hinge joint model with one degree of freedom. This study considered the knee as a plantar joint with motion taking place between parallel sagittal planes and comprising three degrees of freedom (rotation and translation) [5]. Although knee joint motion involves interaction between the tibia, femur, patella and fibula, this study considered only motion at the tibio-femoral joint. We considered only two dimensional images and motion in the sagittal plane in this study and thus a plantar joint model with three degrees of freedom was used. Only knee motion in the sagittal plane was measured with tibial and femoral rotation, with medial and lateral translational and knee abduction/adduction assumed to be negligible. More accurate measurement of knee joint motion would be possible using six degrees of freedom models which can fully describe the relative motion between two bodies and consider movements in the sagittal, coronal, and transverse planes; they may also account for medial–lateral shift and anterior–posterior draw [5]. However, sophisticated equipment, such as video-based systems, electromagnetic devices or fluoroscopy, would be required for such analysis and these may not be suitable for assessment of patient’s knee motion at routine postoperative follow-up.
This study evaluated the use of digital imaging as a method of measuring knee joint motion. The main advantage of this technique is that it does not rely on skin marks placed over bony landmarks, which is particularly useful when taking intra-operative measurements, as wound contamination is a potential risk factor with repeated palpation and indeed the close proximity of an unsterile goniometer device.
This technique also facilitates measurement by the same investigator at a future date, even if the investigator was absent when the image was taken. Measurements can also be made and rechecked. Serial digital images of a patient’s range of motion may facilitate patient education by describing patients’ postoperative improvements relative to their preoperative status. Indeed, such images may prove a useful motivational tool for further patient improvement [7]. Digital images may also be used for professional education and presentation purposes.
Inter-observer and intra-observer analysis revealed a high level of reliability and repeatability which is comparable with goniometric studies [3, 8, 11, 16, 21]. Avoiding camera and/or limb malpositioning is, however, important in order to minimise measurement error.
The issue of patient confidentiality and informed consent with respect to the taking and storage of digital images must be considered [14, 20]. In a study by Cheung et al. [6], 84% of patients surveyed in an emergency department were amenable to a photograph of themselves being used for medical education and 71% to publication in a medical journal [6]. Thus, most patients are agreeable to the use of digital photographs for medical use providing these images are treated in the same manner as medical notes, i.e. strictly private and confidential. In our study, all of the subjects gave informed consent and all of the images were archived in a password protected electronic file system.
The main disadvantage of this technique is that it is relatively time consuming. Access to a digital camera, a computer, and the angle measurement software are also potential drawbacks when compared to the low cost and simplicity of the hand-held goniometer.
In conclusion, we describe a reliable and repeatable method of measuring knee joint motion using digital imaging. This technique has several advantages over the hand-held goniometer and, in particular, is a useful tool for measuring knee motion in the intra-operative setting.
References
- 1.Austin MS, Ghanem E, Joshi A, Trappler R, Parvizi J, Hozack WJ. The assessment of intraoperative prosthetic knee range of motion using two methods. J Arthroplasty. 2008;23(4):515–521. doi: 10.1016/j.arth.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 2.Bengs BC, Scott RD. The effect of distal femoral resection on passive knee extension in posterior cruciate ligament-retaining total knee arthroplasty. J Arthroplasty. 2006;21(2):161–166. doi: 10.1016/j.arth.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 3.Brosseau L, Tousignant M, Budd J, Chartier N, Duciaume L, Plamondon S, O'Sullivan JP, O'Donoghue S, Balmer S. Intratester and intertester reliability and criterion validity of the parallelogram and universal goniometers for active knee flexion in healthy subjects. Physiother Res Int. 1997;2(3):150–166. doi: 10.1002/pri.97. [DOI] [PubMed] [Google Scholar]
- 4.Brown S. Digital imaging in clinical photography, part 1. J Audiov Media Med. 1994;17(2):53–65. doi: 10.3109/17453059409063658. [DOI] [PubMed] [Google Scholar]
- 5.Bull AM, Amis AA. Knee joint motion: description and measurement. Proc Inst Mech Eng [H] 1998;212(5):357–372. doi: 10.1243/0954411981534132. [DOI] [PubMed] [Google Scholar]
- 6.Cheung A, Al-Ausi M, Hathorn I, Hyam J, Jaye P. Patients’ attitudes toward medical photography in the emergency department. Emerg Med J. 2005;22(8):609. doi: 10.1136/emj.2004.019893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunlevy C, Cooney M, Gormely J. Procedural considerations for photographic-based joint angle measurements. Physiother Res Int. 2005;10(4):190–200. doi: 10.1002/pri.9. [DOI] [PubMed] [Google Scholar]
- 8.Edwards JZ, Greene KA, Davis RS, Kovacik MW, Noe DA, Askew MJ. Measuring flexion in knee arthroplasty patients. J Arthroplasty. 2004;19(3):369–372. doi: 10.1016/j.arth.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Fish DR, Wingate L. Sources of goniometric error at the elbow. Phys Ther. 1985;65(11):1666–1670. doi: 10.1093/ptj/65.11.1666. [DOI] [PubMed] [Google Scholar]
- 10.Galdino GM, Vogel JE, Kolk CA. Standardizing digital photography: it's not all in the eye of the beholder. Plast Reconstr Surg. 2001;108(5):1334–1344. doi: 10.1097/00006534-200110000-00037. [DOI] [PubMed] [Google Scholar]
- 11.Gogia PP, Braatz JH, Rose SJ, Norton BJ. Reliability and validity of goniometric measurements at the knee. Phys Ther. 1987;67(2):192–195. doi: 10.1093/ptj/67.2.192. [DOI] [PubMed] [Google Scholar]
- 12.Hutchinson I, Williams P. Digital cameras. Br J Orthod. 1999;26(4):326–331. doi: 10.1093/ortho/26.4.326. [DOI] [PubMed] [Google Scholar]
- 13.Kuo RL, Delvecchio FC, Preminger GM. Use of a digital camera in the urologic setting. Urology. 1999;53(3):613–616. doi: 10.1016/S0090-4295(98)00489-0. [DOI] [PubMed] [Google Scholar]
- 14.Mah ET, Thomsen NO. Digital photography and computerisation in orthopaedics. J Bone Joint Surg Br. 2004;86(1):1–4. [PubMed] [Google Scholar]
- 15.Moore ML. The measurement of joint motion; introductory review of the literature. Phys Ther Rev. 1949;29(5):195–205. [PubMed] [Google Scholar]
- 16.Rothstein JM, Miller PJ, Roettger RF. Goniometric reliability in a clinical setting. Elbow and knee measurements. Phys Ther. 1983;63(10):1611–1615. doi: 10.1093/ptj/63.10.1611. [DOI] [PubMed] [Google Scholar]
- 17.Rutka JT, Otsubo H, Kitano S, Sakamoto H, Shirasawa A, Ochi A, Snead OC., III Utility of digital camera-derived intraoperative images in the planning of epilepsy surgery for children. Neurosurgery. 1999;45(5):1186–1191. doi: 10.1097/00006123-199911000-00033. [DOI] [PubMed] [Google Scholar]
- 18.Salter N. Methods of measurement of muscle and joint function. J Bone Joint Surg Br. 1955;37-B(3):474–491. doi: 10.1302/0301-620X.37B3.474. [DOI] [PubMed] [Google Scholar]
- 19.Wade FA, Oliver CW. Living with digital imaging. Clin Orthop Relat Res. 2004;421:25–28. doi: 10.1097/01.blo.0000126870.74832.d7. [DOI] [PubMed] [Google Scholar]
- 20.Wade FA, Oliver CW, McBride K. Digital imaging in trauma and orthopaedic surgery: is it worth it? J Bone Joint Surg Br. 2000;82(6):791–794. doi: 10.1302/0301-620X.82B6.11390. [DOI] [PubMed] [Google Scholar]
- 21.Watkins MA, Riddle DL, Lamb RL, Personius WJ. Reliability of goniometric measurements and visual estimates of knee range of motion obtained in a clinical setting. Phys Ther. 1991;71(2):90–96. doi: 10.1093/ptj/71.2.90. [DOI] [PubMed] [Google Scholar]
- 22.Wirthlin DJ, Buradagunta S, Edwards RA, Brewster DC, Cambria RP, Gertler JP, LaMuraglia GM, Jordan DE, Kvedar JC, Abbott WM. Telemedicine in vascular surgery: feasibility of digital imaging for remote management of wounds. J Vasc Surg. 1998;27(6):1089–1099. doi: 10.1016/S0741-5214(98)70011-4. [DOI] [PubMed] [Google Scholar]