Abstract
The purpose of this study was to compare the operative outcome between mini and standard incisions in total hip arthroplasty (THA). We identified 12 randomised or quasi-randomised control trials (RCT or qRCT) published between 1996 and 2008. Subgroup and sensitivity analyses were performed to evaluate the differences in results for surgical approach, trial quality, and follow-up duration. Operative time and blood loss were significantly reduced in the mini-incision group for studies with the posterior or posterolateral approach. Concerning postoperative complications, there were no significant differences between the two groups with no significant heterogeneity. No differences were observed between the two groups for Harris hip score and radiographic results except for cup anterversion. Although mini-incision appeared to have similar outcomes compared to standard incision, the follow-up is short-term according to current standards in THA. High-quality studies are required to compare the outcomes of these two procedures.
Resumé
Le but de cette étude est de comparer le devenir opératoire des patients ayant bénéficié d'une prothèse totale de hanche par voie mini-invasive ou par incision standard. Nous avons identifié 12 publications d'essais randomisés ou quasi randomisés (RCT ou qRCT) publiées entre 1996 et 2008. Des sous-groupes ont été réalisés de façon à évaluer la différence des résultats selon l'approche chirurgicale, la qualité des essais et la durée du suivi. Le temps opératoire et les pertes sanguines étaient significativement moins importants dans le groupe mini-incision réalisé par voie postérieure ou postéro-latérale. Il n'y a pas de différence significative dans les complications postopératoires entre les deux groupes de même en ce qui concerne le score de Harris, les résultats radiologiques exceptés pour l'antéversion de la cupule. Cependant, la mini incision semble avoir un devenir comparable à l'incision standard, mais avec des suites plus rapides. Des études ultérieures de grande qualité seront nécessaires pour comparer le devenir de ces deux procédés.
Introduction
Total hip arthroplasty (THA) has been one of the most successful orthopaedic procedures over the past 30 years [30, 45]. Recently, the techniques of exposure for THA have undergone great change, allowing surgeons to perform THA through mini-incisions (MI) [17, 28]. There has been much controversy over MI versus standard incisions (SI). Mini-incisions have been claimed by opponents to be deleterious and potentially more prone to complications, mainly due to component malpositioning or compromised fixation [5, 6, 46]. Internet advertising has increased patient awareness and demands for MI THA. However, information on the Internet regarding minimally invasive THA is misleading and of poor quality [25, 26]. It is understandable that some surgeons do not want to change to a small incision because of the superb results with THA using long incisions [22, 29]. Proponents of MI claim that mini-incision results perioperatively in less soft-tissue trauma (smaller skin incision and less muscle damage), reduced blood loss and fewer blood transfusion requirements. Postoperative benefits include less pain, quicker recovery (e.g. earlier return to normal gait) and better cosmetic appearance [8, 11, 33]. Overall, there is conflicting data as to the efficacy of these approaches regarding blood transfusions, pain control, length of hospital stay, and duration of recovery [3, 41, 42, 48].
The lack of objective data to demonstrate the benefit of the new procedure has been noted by some authors, who have stressed the importance of the minimally invasive technique to the orthopaedic community and the need for research to determine its effectiveness [12]. With this background, it is important to determine if there is any scientific evidence to support the use of small incision operations.
Recently, there have been several randomised or quasi-randomised control trials (RCTs or qRCTs) comparing MI THA versus SI THA [12, 13, 23, 43, 52]. RCTs are widely accepted as the most reliable method of determining the effectiveness of specific therapies [37]. However, currently these data have not been pooled for evaluation of overall outcomes. The aim of our study was to use meta-analytical techniques to compare intraoperative and postoperative outcomes from randomised or quasi-randomised studies of MI versus SI in patients undergoing THA.
Materials and methods
In order to assemble all the relevant literature, a comprehensive search of Medline, Embase, CBMdisc, the Cochrane database and Google Scholar was performed on all peer-reviewed studies between 1994 and 2008 for randomised or quasi-randomised trials comparing MI versus SI in patients undergoing THA. The following search terms were used: hip, arthroplasty, replacement, THR, THA, prosthesis/prostheses/implant, minimally invasive/less invasive, MIS, mini-incision/minimal incision/small incision. The “related articles” feature was used in Pubmed to broaden the search, and all titles, abstracts, studies, and citations scanned were reviewed. References of the articles acquired in full were also reviewed. We made no language restrictions. If relevant information was specified, we contacted the authors for unpublished data. The latest date for this search was September 9, 2008.
Two of the authors (Tao Cheng and Jiu Geng Feng) independently extracted the following data from each study: first author, year of publication, country of origin, follow-up duration, population, sample size, study design, inclusion and exclusion criteria, treatment characteristics, and outcomes parameters. In order to be included in the analysis, included studies had to compare MI and SI techniques in patients undergoing THA. There was no limit to type of prosthesis, duration of follow-up and preoperative diagnosis. The studies included clearly documented the technique as “minimally invasive or MI”. Studies were excluded from the analysis if: (1) the outcomes of interest were not reported for the two techniques, (2) it was impossible to extrapolate or calculate the necessary data from the published results, and (3) studies containing previously published data. The following outcome parameters were used to compare the MI with the SI group: (1) operative outcome including blood loss and operative time, (2) length of hospital stay, (3) functional outcome including Harris hip score (HHS), (4) adverse events including postoperative complications, and (5) radiographic outcomes including cup inclination, cup anterversion, angulation of the stem, acetabular outlier, femoral outlier, grade of cement mantle.
We performed our meta-analysis in line with Cochrane Collaboration and the Quality of Reporting of Meta-analyses guidelines [16]. For continuous outcome data such as operative time or blood loss, means and standard deviations were used to calculate a weighted mean difference (WMD) and 95% confidence interval (CI) in the meta-analysis. For dichotomous outcomes such as postoperative complications the odds ratio (OR) and 95% CI were calculated as the summary statistics. For ordinal outcome data including grade of cement mantle were meta-analysed as dichotomous data. The Mantel-Haenszel method was used to combine the OR for the outcomes of interest using a “random effect” meta-analytical technique. In a random effect model it is assumed that there is variation between studies and the calculated OR thus has a more conservative value. In surgical research, meta-analysis using the random effect model is preferable particularly because patients that are operated upon in different centres have varying risk profiles and selection criteria for each surgical technique [39]. For those studies that contained a zero in one cell for the number of events of interest in one of the two groups, we used Yates’ correction. These cells create problems with the computation of ratio measures and standard errors of treatment effects. We resolved this by adding the value 0.5 in each cell of the 2 × 2 table for the study in question. We excluded studies with no events in either group. The quality of the studies was assessed by using the Jadad score (Table 1) [19, 20]. Studies achieving three or more points (from a maximum of five) were considered to be of high quality. Subgroup analysis was performed by considering studies with posterior or posterolateral approach, high quality studies only, and follow-up of at least 12 months. The test for heterogeneity was considered significant when p < 0.1, which cast doubt on the statistical validity of the pooling [36]. The possible value of I2 ranges from 0% to 100% ,and values ≥75% imply very high heterogeneity. The source of heterogeneity was investigated by performing subgroup and sensitivity analysis and considering clinical reasons for potential clinical heterogeneity. Analysis was conducted by using Review Manager version 5.0 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
Table 1.
Methodological criteria
| Checklist | Aspect | Description | Item |
|---|---|---|---|
| Jadad et al. [21] | Randomisation | Was the study described as randomised? | J1 |
| Was the method of randomisation described and appropriate? | J2 | ||
| Blinding | Was the study described as double blind? | J3 | |
| Was the method of blinding described and appropriate? | J4 | ||
| Lost patients | Was there a description of withdrawals and dropouts? | J5 |
Results
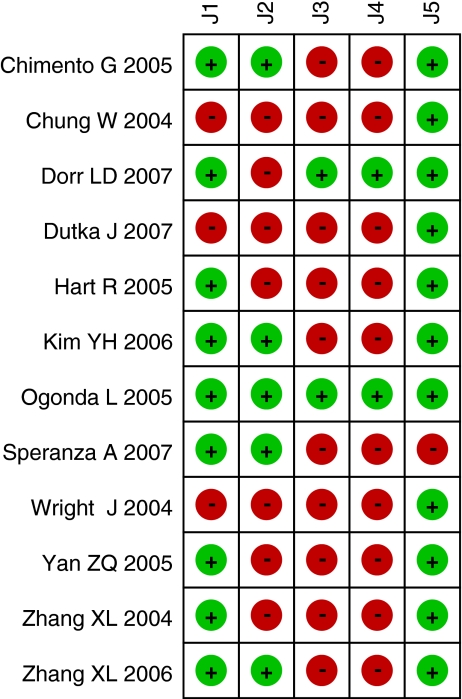
Twelve randomised or quasi-randomised control trials were included in the meta-analysis [8, 9, 12, 13, 15, 23, 35, 43, 49–52]. A total of 1,205 hips were included in the 12 studies, 597 hips in the MI group and 608 in the SI group. The study characteristics of these 12 studies are shown in Tables 2 and 3. Each study fulfilled the inclusion and exclusion criteria and only randomised or quasi-randomised elective surgical case data was used. Although all the studies explicitly stated that the comparison was between MIS and SIS, the incision type for the former were variable. Overall, the methodological quality of the partial trials was found to be low, and may have been more a consequence of incomplete reporting. Some of the included randomised trials did not adequately describe quality items (e.g., mode of randomisation, blinding, allocation concealment) that are often used for the assessment of overall trial quality. The randomisation technique was only mentioned in five of the 12 trials, which included table-generated randomisation and drawing a card. Allocation concealment was documented in only one trial. Blinding is rarely used in orthopaedic surgery trials. None of the studies used blinding of the surgeon. Two studies used patient blinding and seven studies used observer blinding. There were descriptions of withdrawals and dropouts in 11 studies. Among the 12 studies, there were different preoperative diagnoses including osteoarthritis, rheumatoid arthritis, post-traumatic arthritis, hip dysplasia, and osteonecrosis. A variety of hip prostheses were used in the 12 trials. The methodological scores of the trials are given in Fig. 1, and a Forest plot for postoperative complications is given in Fig. 2.
Table 2.
Characteristics of studies
| Study | Methods | Participants | Interventions | Outcome |
|---|---|---|---|---|
| Zhang et al. [51] (China) | RCT; FU = 11 weeks | FNF = 60 MI vs 60 SI; similar DC; unilateral THA | MI anterolateral 8.2 cm vs SI posterior 14 cm; similar DC; unilateral THA Versys cementless prosthesis | Operative time; blood loss; HHS; complications |
| Wright et al. [49] (USA) | qRCT; presence of assistant; FU = 5 years | OA, ON, RA = 42 MI vs 42 SI; similar DC; unilateral THA | MI posterolateral 8.8 ± 1.5 cm vs SI posterolateral 23.0 ± 2.1 cm press-fit cup and cemented stem; a senior surgeon | Operative time; blood loss; HHS ; complications radiographic evaluation |
| Chung et al. [9] (Australia) | qRCT; observer blinded; alternation; FU = 14 months | OA = 60 MI vs 60 SI; similar DC; unilateral THA | MI posterolateral 9.2 cm vs SI posterolateral 20.0 cm; porous-coated cup and uncemented stem | Operative time; blood loss; length of hospital stay; HHS; complications |
| Hart et al. [15] (Czech Republic) | RCT; observer blinded; FU = 39 months | OA = 60 MI vs 60 SI; similar DC; unilateral THA | MI posterolateral 9–10 cm vs SI posterolateral 20 cm; cemented prosthesis; two experienced surgeons | Operative time; blood loss; complications radiographic evaluation |
| Chimento et al. [8] (USA) | RCT draw card observer blinded; FU = 2 years | OA = 28 MIS vs 32 SIS; similar DC; unilateral THA | MI posterolateral 8 cml vs SI posterolateral 15 cm; press-fit cup cemented or press-fit stem; a senior surgeon | Operative time; blood loss; complications radiographic evaluation |
| Yan et al. [50] (China) | RCT; FU = 6 months | OA , ON, FNF = 15 MI vs 15 SI; similar DC; unilateral THA | MI anterior two incisions 3.6 cm, 5.7 cm vs SI posterolateral 12 cm; Versys cementless prosthesis; a senior surgeon | Operative time; blood loss; complications radiographic evaluation |
| Ogonda et al. [35] (UK) | RCT sealed envelope patient and observer blinded; FU = 6 weeks | OA , ON ,RA = 109 MI vs 110 SI; similar DC; unilateral THA | MI posterolateral 9.5 ± 0.95 cm vs SI posterolateral 15.81 ± 0.93 cm cementless cup cemented stem; a experienced surgeon | Operative time; blood loss; HHS; complications radiographic evaluation |
| Zhang et al. [52] (China) | RCT sealed envelope; FU = 20 months | OA, RA = 60 MIS vs 60 SIS; similar DC; unilateral THA | MI anterior 6.9 cm vs SI posterolateral 16.3 cm Versys hip prosthesis | Operative time; blood loss; HHS; complications radiographic evaluation |
| Kim et al. [23] (Korea) | RCT randomized number table observer blinded; FU = 26.4 months | ON, OA, AS = 70 MIS vs 70 SIS; similar DC; bilateral THA | MI posterolateral 8.8 ± 1.5 cm vs SI posterolateral 23.0 ± 2.1 cm cementless cup and cementless stem; a senior surgeon | Operative time; blood loss; HHS; length of hospital stay; Complications; radiographic evaluation |
| Dorr et al. [12] (USA) | RCT patient and observer blinded; FU = 3 months | OA, PA, HD, ON = 30 MIS vs 30 SIS; similar DC; unilateral THA | MI posterior 10 ± 2 cm vs SI posterior 20 ± 2 cm; cementless cup noncemented stem; two experienced surgeons | Operative time; blood loss; HHS; complications radiographic evaluation |
| Dutka et al. [13] (Poland) | qRCT odd or even day observer blinded; FU = 9.5 months | OA, HD, ON = 60 MIS vs 60 SIS; similar DC; unilateral THA | MI lateral 6–8 cm vs SI direct lateral 20–25 cm | Operative time; blood loss; HHS; length of hospital stay; complications |
| Speranza et al. [43] (Italy) | RCT draw; FU = 6 months | OA, ON, FNF = 50 MIS vs 50 SIS; similar DC; unilateral THA | MI direct lateral 7.1 ± 1.1 cm vs SI posterior 12.8 ± 2.3 cm; cementless cup cementless stem; a senior surgeon | Operative time; blood loss; HHS; length of hospital stay; complications |
MI mini incision, SI standard incision, OA osteoarthritis, RA rheumatoid arthritis, PA posttraumatic arthritis, HD hip dysplasia, ON osteonecrosis, FU follow-up, DC demographic characteristic, FNF femoral neck fracture, HHS Harris hip score
Table 3.
Results of overall meta-analysis
| Outcome | No. of studies | No. of patients | OR/WMD (95%CI) | p-value | HG p-value |
|---|---|---|---|---|---|
| Perioperative outcome | |||||
| Operative time | 9 | 875 | −1.07 (−6.88, 4.74) | 0.72 | <0.00001 |
| Intraoperative blood loss | 9 | 875 | −79.75 (−125.45, −34.04) | 0.0006 | <0.00001 |
| Postoperative complications | 12 | 1205 | 1.08 (−0.59, 1.97) | 0.81 | 0.85 |
| Length of stay | 4 | 330 | −3.59 (−5.69, −1.50) | 0.0008 | <0.00001 |
| HHS | 5 | 513 | 3.99 (−0.18, 8.16) | 0.06 | <0.00001 |
| Radiographic outcome | |||||
| Cup inclination | 5 | 569 | 0.57 (−0.85, 1.98) | 0.43 | 0.11 |
| Cup anterversion | 4 | 350 | 2.90 (1.05, 4.74) | 0.002 | 0.04 |
| Stem angle | 3 | 419 | 0.01 (−0.49, 0.51) | 0.98 | 0.05 |
| Acetabular outlier | 4 | 504 | 1.02 (0.64, 1.62) | 0.94 | 0.92 |
| Femoral outlier | 4 | 599 | 0.75 (0.50, 1.12) | 0.16 | 0.75 |
| Grade of cement mantle | 2 | 279 | 0.83 (0.48, 1.43) | 0.49 | 0.66 |
NO number, OR odds ratio, WMD weighed mean difference, HG heterogeneity, HHS Harris hip score
Fig. 1.
Methodological quality summary by using the Jadad Score
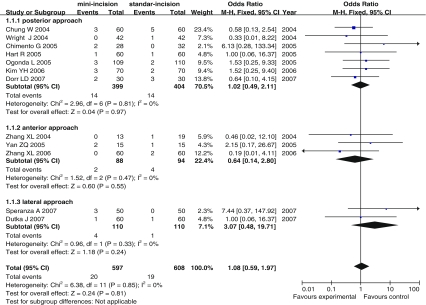
Fig. 2.
Forest plot for postoperative complication overall. CI confidence interval, WMD weighted mean difference
Using a random effects model, the overall results demonstrated that there was no significant difference in operating time between the MI and SI groups (WMD = −1.07, 95%CI −6.88, 4.74; p = 0.72) with very high heterogeneity (I2 = 91%) (Table 3). Subgroup analysis for studies with a Jadad score of 3 or more demonstrate that there was no significant differences between the two groups with respect to operative time (WMD = −1.06, 95% CI −8.11,5.99; p = 0.77) with high heterogeneity (I2 = 88%). When studies with the posterior or posterolateral approach were analysed separately, operative time was reduced in the MI group (WMD −4.73 min, 95% CI −7.37,−2.09; p = 0.0004) with moderate heterogeneity (I2 = 26 %) (Table 4).
Table 4.
Result of subgroup analysis with respect to operative time, intraoperative blood loss, and postoperative complications
| Outcome | No. of studies | No. of patients | OR/WMD (95%CI) | p-value | HG p-value |
|---|---|---|---|---|---|
| Studies with a Jadad score 3 or more | |||||
| Operative time | 4 | 459 | −1.06 (−8.11, 5.99) | 0.77 | <0.00001 |
| Intraoperative blood loss | 4 | 459 | −86.85 (−59.89, −13.81) | 0.02 | <0.00001 |
| Postoperative complications | 5 | 599 | 1.13 (0.47, 2.69) | 0.79 | 0.56 |
| Studies with posterior approach | |||||
| Operative time | 5 | 543 | −4.73 (−7.37, −2.09) | 0.0004 | 0.24 |
| Intraoperative blood loss | 5 | 543 | −45.75 (−65.07, −26.43) | <0.00001 | 0.10 |
| Postoperative complications | 7 | 803 | 1.02 (0.49, 2.11) | 0.97 | 0.81 |
| Studies with a follow-up of at least 12 months | |||||
| Postoperative complications | 6 | 644 | 0.85 (0.37, 1.96) | 0.70 | 0.63 |
NO number, OR odds ratio, WMD weighed mean difference, HG heterogeneity
Using a random effects model, intraoperative blood loss was reduced in the MI group (WMD −79.75 ml, 95% CI −125.45, −34.04; p = 0.0006) with significant heterogeneity (I2 = 92%) overall. Subgroup analysis for studies with a Jadad score of 3 or more demonstrate that intraoperative blood loss was also reduced in the MI group (WMD = −86.85, 95% CI −159.89, −13.81; p = 0.02) with significant heterogeneity (I2 = 91%). When studies with the posterior or posterolateral approach were analysed separately, intraoperative blood loss was reduced significantly in the MI group (WMD −45.75 ml, 95% CI −65.07,−26.43; p < 0.0001) with moderate heterogeneity (I2 = 48 %).
The weighted mean difference with the random effect model was −3.59 days for the length of hospital stay (95% CI −5.69,−1.50; p = 0.0008) with significant heterogeneity (I2 = 97%). For all postoperative complications (see Table 5), there was no significant difference (OR 1.08, 95% CI 0.59, 1.97; p = 0.81) between the two groups without heterogeneity (I2 = 0%). To demonstrate complications, subgroup analysis for studies with a Jadad score of 3 or more and posterior or posterolateral approach showed no significant difference between the two groups without heterogeneity (I2 = 0%). When studies with follow-up of at least 12 months were analysed separately, there was also no significant difference without heterogeneity (I2 = 0%).
Table 5.
Results of postoperative complications
| Outcome | No. of studies | No. of patients | MI | SI |
|---|---|---|---|---|
| Dislocation | 5 | 623 | 5 | 4 |
| Deep venous thrombosis | 5 | 551 | 3 | 10 |
| Infection | 3 | 419 | 4 | 0 |
| Nerve palsy | 3 | 270 | 4 | 1 |
| Periprosthetic fracture | 3 | 190 | 3 | 3 |
| Subcutaneous haematous | 1 | 120 | 0 | 1 |
| Wound healing | 1 | 120 | 1 | 0 |
| Total | 12 | - | 20 | 19 |
NO number, MI mini-incision, SI standard incision
The Harris hip score (HHS), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the Oxford hip score were used for the clinical assessment of patients (in nine trials, two trials and one trial, respectively). However, summary score data necessary for quantitative analyses were incompletely reported. The mean changes and the standard deviations in postoperative HHS were calculated for only five trials. The available data were very highly heterogeneous (I2 = 90%) and, overall, they showed no significant difference between the compared arms (WMD = 3.99, 95% CI −0.18, 8.16; p = 0.06).
Only a minority of trials reported the mean and the standard deviations with respect to radiographic measurements. The weighted mean difference for cup inclination was 0.57 (95% CI −0.85, 1.98), with no significant difference between the two groups (p = 0.34) with moderate heterogeneity (I2 = 47%). Using random effects modelling, the result of cup anterversion demonstrated that there was a significant increase in the MI group (MWD = 2.90, 95% CI 1.05, 4.74; p = 0.002) with significant heterogeneity (I2 = 63%). Sensitivity analysis revealed that omission from the pooled analysis of the study from Zhang et al. [52] resulted in no significant differences (p = 0.07) between two groups with respect to cup anterversion. The weighted mean difference for stem angle on the anteroposterior radiograph was 0.01 (95% CI −0.49, 0.51) for varus; there was no significant difference between the two groups (p = 0.97), with significant heterogeneity (I2 = 67%). Meta-analysis showed there was no significant difference between the two groups with respect to acetabular (OR = 1.02, 95% CI 0.64, 1.62, p = 0.94) or femoral outlier (OR = 0.75, 95% CI 0.50, 1.12, p = 0.16), with no heterogeneity (I2 = 0%). The data concerning grade of cement mantle could be dichotomised, that is, grades A, B constitute a success, while grades C, D constitute a failure. The odds ratio (−0.83, 95% CI −0.48, 1.43) for cement mantle showed no significant difference between the two groups (p = 0.26) with no heterogeneity (I2 = 0%).
Discussion
The goals of THR should be to relieve pain and restore function with a minimum of complications and adverse events. Cosmesis and the ultra-short-term results are minor priorities. It is clear that the minimal incision technique is not a minimally invasive operation [1, 2].
The major ambiguity of this study lies in the varying definition of MI used by the different studies. Reported lengths of incision varied from 6–10 cm. Currently, multiple mini-incision approaches have been described to include anterior, anterolateral, direct lateral, posterior, posterolateral, and a direct two-incision approach [2–28, 34, 38, 44]. Minimally invasive THA involves a modified surgical dissection that uses internervous planes while minimising any tendon or muscle trauma during the exposure [10, 19, 28, 29]. High-technology computer navigation can be used for correct positioning of the components given the decreased visualisation of minimally invasive surgery [32, 40]. Choice of implants and cementing techniques was highly variable across studies when reported.
In some studies the size of the comparative groups was small, because it would have been extremely difficult to recruit patients if the differences in incision lengths were so marked. Total patients enrolled ranged from 30 to 219 patients, with 50% of the studies having less than 120 patients. In the meta-analysis, these available data had been pooled to clarify the controversy over MI versus standard SI.
Most studies did not assess the long-term results for these patients. Only one study was conducted to evaluate five-year clinical outcome [49]. The follow-up period was short but covered the critical time when the benefits of the minimally invasive approach to THA are supposed to be maximal. Flören et al. found that the MI THA technique did not compromise the long-term clinical and radiographic findings when compared with conventional techniques [14]. However, it was not a rigorously prospective controlled study. Future reports of longer-term follow-up in the next few years will give us a more accurate reflection of adverse effects and revision rates.
From individual randomised control trials it is unclear whether the MI technique does improve the intraoperative and postoperative outcomes. In a meta-analysis, a marginal difference was found between MI and IS THA [47]. The study designs were accepted in the meta-analysis including RCTs, as well as prospective and retrospective nonrandomised controlled trials (nRCTs) between 2003 and 2005. When there was significant heterogeneity of outcome across studies, absence of subgroup and sensitivity analyses precluded reliable inference in the meta-analysis. The strengths of our review include the clear definition of the research question to eliminate bias in study selection, adherence to an explicit research protocol developed before the analysis, the comprehensive nature of the literature search regardless of language, and data extraction through cross-checking of all quantitative information by two of the authors. Inclusion of only RCTs or qRCTs enables one to assemble a large volume of clinical data (on 1,205 patients) from the most rigorous evidence. The appropriate pooling of data is highlighted by the fact that heterogeneity between studies was considered on overall or subgroup analysis. Our study also reviewed peer-review articles being published in the last two to three years from different countries and institutions, indicating growing interest and development in this field.
Operative times showed no significant differences between MI and SI groups overall, but there was strong statistical heterogeneity. This makes it difficult to draw conclusions about differences in operative time between the two groups, and subgroup analysis demonstrated that operative time was reduced in the MI group through a posterior or posterolateral approach with moderate heterogeneity, but it is unclear if 4.73 minutes is a clinically significant effect size. There is bound to be variation between the various MI THA techniques involving surgical approach and specialised instrumentation. The two-incision was described as the most time consuming, and the main advantage of the posterolateral approach compared with other mini-incisions is its simplicity, with shortened operating time as a result [4]. The various hip scores were incompletely reported or were not reported at all, precluding their inclusion in the calculations. Hence, the corresponding syntheses should be interpreted with caution. These functional outcomes published at different stages in follow-up may affect the comparability and the reliability of the different results.
Since complications rates were low, we pooled all types of postoperative complications. Total and subgroup analyses indicated that there was no significant difference between the two groups with no significant heterogeneity. In most included studies, there were no intraoperative complications or technical difficulties. None of the incisions required intraoperative conversion to a longer incision. Dislocation, transient nerve palsy, and infection were slightly more common with the MI techniques. On the other hand, postoperative deep venous thrombosis (DVT) was slightly more prevalent in the SI group. We would argue that the much higher infection and nerve palsy rates in the MIS group should not be ignored. DVT may be asymptomatic and cause no distress to the patient but infection and nerve palsy are major tragedies.
Although we cannot conclude that component positioning and cement mantle directly translate into improved implant longevity or outcome, the literature and clinical experience tell us that there is a strong relationship between them. For the outcome of radiographical evaluation, similar inferences based on several trials with longer or shorter follow-up may be precarious because of the limited amount of accumulated information. Incomplete reporting or non-reporting of outcomes may be related to their level of significance in the pertinent trials [7]. This phenomenon has been termed “outcome reporting bias” and may influence the results of the quantitative synthesis.
Most studies have reported improved cosmesis and patient satisfaction with these smaller incision approaches [3, 36, 49]. Howell et al. gave significant importance to the psychological impact of improved cosmesis on patient attitude, satisfaction, and motivation for recovery, and cautioned that this appeal should not be underestimated [18]. However, the cosmetics of mini-incision total hip replacement scars may be inferior to standard-incision scars because of skin and soft tissue damage produced by high retractor pressures needed for exposure using a limited skin incision [30, 31]. The decreased skin blood flow in mini-incision THA due to excessive forces applied to the tissue by retractors may cause early postoperative wound complications [24]. A cosmetically better result of the hip arthroplasty is through step-by-step reduction of the incision and the benefits of suitable instruments under less blood loss [47]. Complication rates and learning curve may be altered by changes in training and surgical techniques [1]. THA through minimally invasive techniques is safe and reproducible in the hands of a highly experienced surgeon who has selected the appropriate patients.
In conclusion, this meta-analysis has illustrated that MI appeared to have similar short-term operative outcomes compared to SI. Although meta-analysis cannot improve the quality of included studies, our study may help the orthopaedic community to clearly define what variables need to be evaluated and included in future RCTs and thereby establish some standards by which future studies provide information regarding MI THA. Because the overall quality of published articles and length of follow-up is low, intermediate and long-term follow-up of high-quality RCTs are needed to demonstrate any anticipated improvement in implant survivorship as well as any associated improvement in clinical outcomes.
Acknowledgments
We thank for Dr. L.D. Dorr, P. Vavken and Y.S. Chen, MD for providing additional information regarding their studies.
Conflict of interest statement Each author certifies that he or she has no commercial associations that might pose a conflict of interest in connection with the submitted article.
Footnotes
Tao Cheng, Jiu Geng Feng and Tao Liu all contributed equally to this work.
References
- 1.Archibeck MJ, White RE., Jr Learning curve for the two-incision total hip replacement. Clin Orthop Relat Res. 2004;429:232–238. doi: 10.1097/01.blo.0000150272.75831.2f. [DOI] [PubMed] [Google Scholar]
- 2.Aziz O, Rao C, Panesar SS, Jones C, Morris S, Darzi A. Meta-analysis of minimally invasive internal thoracic artery bypass versus percutaneous revascularisation for isolated lesions of the left anterior descending artery. BMJ. 2007;334:617. doi: 10.1136/bmj.39106.476215.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berger RA, Jacobs JJ, Meneghini RM, Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429:239–247. doi: 10.1097/01.blo.0000150127.80647.80. [DOI] [PubMed] [Google Scholar]
- 4.Bottner F, Delgado S, Sculco TP. Minimally invasive total hip replacement: the posterolateral approach. Am J Orthop. 2006;35:218–224. [PubMed] [Google Scholar]
- 5.Callaghan J. Skeptical perspectives on minimally invasive total hip arthroplasty. J Bone Joint Surg Am. 2006;85:2242–2243. [Google Scholar]
- 6.Cameron HU. Mini-incisions: visualization is key. Orthopedics. 2002;25:473. doi: 10.3928/0147-7447-20020501-12. [DOI] [PubMed] [Google Scholar]
- 7.Chan AW, Hróbjartsson A, Haahr MT, Gøtzsche PC, Altman DG. Empirical evidence for selective reporting of outcomes in randomized trials: comparison of protocols to published articles. JAMA. 2004;291:2457–2465. doi: 10.1001/jama.291.20.2457. [DOI] [PubMed] [Google Scholar]
- 8.Chimento GF, Pavone V, Sharrock N, Kahn B, Cahill J, Sculco TP. Minimally invasive total hip arthroplasty: a prospective randomized study. J Arthroplasty. 2005;20:139–144. doi: 10.1016/j.arth.2004.09.061. [DOI] [PubMed] [Google Scholar]
- 9.Chung WK, Liu D, Foo LS. Mini-incision total hip replacement-surgical technique and early results. J Orthop Surg (Hong Kong) 2004;12:19–24. doi: 10.1177/230949900401200105. [DOI] [PubMed] [Google Scholar]
- 10.Beer J, Petruccelli D, Zalzal P, Winemaker MJ. Single-incision, minimally invasive total hip arthroplasty: length doesn't matter. J Arthroplasty. 2004;19:945–950. [PubMed] [Google Scholar]
- 11.DiGioia AM, 3rd, Plakseychuk AY, Levison TJ, Jaramaz B. Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty. 2003;18:123–128. doi: 10.1054/arth.2003.50025. [DOI] [PubMed] [Google Scholar]
- 12.Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni LE. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty. A prospective, randomized, blinded study. J Bone Joint Surg Am. 2007;89:1153–1160. doi: 10.2106/JBJS.F.00940. [DOI] [PubMed] [Google Scholar]
- 13.Dutka J, Sosin P, Libura M, Skowronek P. Total hip arthroplasty through a minimally invasive lateral approach-our experience and early results. Orthop Traumatol Rehabil. 2007;9:39–45. [PubMed] [Google Scholar]
- 14.Flören M, Lester DK. Durability of implant fixation after less-invasive total hip arthroplasty. J Arthroplasty. 2006;21:783–790. doi: 10.1016/j.arth.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Hart R, Stipcák V, Janecek M, Visna P. Component position following total hip arthroplasty through a miniinvasive posterolateral approach. Acta Orthop Belg. 2005;71:60–64. [PubMed] [Google Scholar]
- 16.Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews of interventions version 5.0. The Cochrane Collaboration
- 17.Howell JR, Garbuz DS, Duncan CP. Minimally invasive hip replacement: rationale, applied anatomy, and instrumentation. Orthop Clin North Am. 2004;35:107–118. doi: 10.1016/S0030-5898(03)00112-3. [DOI] [PubMed] [Google Scholar]
- 18.Howell JR, Masri BA, Duncan CP. Minimally invasive versus standard incision anterolateral hip replacement: a comparative study. Orthop Clin North Am. 2004;3:153–162. doi: 10.1016/S0030-5898(03)00137-8. [DOI] [PubMed] [Google Scholar]
- 19.Ilizaliturri VM, Jr, Chaidez PA, Valero FS, Aguilera JM. Small incision total hip replacement by the lateral approach using standard instruments. Orthopedics. 2004;27:377–381. doi: 10.3928/0147-7447-20040401-11. [DOI] [PubMed] [Google Scholar]
- 20.Jacobs WC, Clement DJ, Wymenga AB. Retention versus removal of the posterior cruciate ligament in total knee replacement: a systematic literature review within the Cochrane framework. Acta Orthop. 2005;76:757–768. doi: 10.1080/17453670510045345. [DOI] [PubMed] [Google Scholar]
- 21.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary. Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 22.Keener JD, Callaghan JJ, Goetz DD, Pederson D, Sullivan P, Johnston RC. Long-term function after Charnley total hip arthroplasty. Clin Orthop Relat Res. 2003;417:148–156. doi: 10.1097/01.blo.0000096807.78689.19. [DOI] [PubMed] [Google Scholar]
- 23.Kim YH. Comparison of primary total hip arthroplasties performed with a minimally invasive technique or a standard technique: a prospective and randomized study. J Arthroplasty. 2006;21:1092–1098. doi: 10.1016/j.arth.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 24.Kiyama T, Naito M, Shitama H, Shinoda T, Maeyama A. Comparison of skin blood flow between mini-and standard-incision approaches during total hip arthroplasty. J Arthroplast. 2008;23:1045–1049. doi: 10.1016/j.arth.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 25.Klein GR, Parvizi J, Sharkey PF, Rothman RH, Hozack WJ. Minimally invasive total hip arthroplasty: internet claims made by members of the Hip Society. Clin Orthop Relat Res. 2005;441:68–70. doi: 10.1097/01.blo.0000192380.54520.8f. [DOI] [PubMed] [Google Scholar]
- 26.Labovitch RS, Bozic KJ, Hansen E. An evaluation of information available on the internet regarding minimally invasive hip arthroplasty. J Arthroplasty. 2006;21:1–5. doi: 10.1016/j.arth.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 27.Laffosse JM, Chiron P, Molinier F, Bensafi H, Puget J. Prospective and comparative study of the anterolateral mini-invasive approach versus minimally invasive posterior approach for primary total hip replacement—early results. Int Orthop. 2007;31:597–603. doi: 10.1007/s00264-006-0247-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levine BR, Klein GR, Cesare PE. Surgical approaches in total hip arthroplasty: a review of the mini-incision and MIS literature. Bull NYU Hosp Jt Dis. 2007;65:5–18. [PubMed] [Google Scholar]
- 29.Malik A, Dorr LD. The science of minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2007;463:74–84. doi: 10.1097/BLO.0b013e3181468766. [DOI] [PubMed] [Google Scholar]
- 30.McAuley JP, Szuszczewicz ES, Young A, Engh CA., Sr Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004;418:119–125. doi: 10.1097/00003086-200401000-00019. [DOI] [PubMed] [Google Scholar]
- 31.Mow CS, Woolson ST, Ngarmukos SG, Park EH, Lorenz HP. Comparison of scars from total hip replacements done with a standard or a mini-incision. Clin Orthop Relat Res. 2005;441:80–85. doi: 10.1097/01.blo.0000191317.85422.c3. [DOI] [PubMed] [Google Scholar]
- 32.Murphy SB, Ecker TM, Tannast M. THA performed using conventional and navigated tissue-preserving techniques. Clin Orthop Relat Res. 2006;453:160–167. doi: 10.1097/01.blo.0000246539.57198.29. [DOI] [PubMed] [Google Scholar]
- 33.Musil D, Stehlík J, Verner M. A comparison of operative invasiveness in minimally invasive anterolateral hip replacement (MIS-AL) and standard hip procedure, using biochemical markers. Acta Chir Orthop Traumatol Cech. 2008;75:16–20. [PubMed] [Google Scholar]
- 34.Nakamura S, Matsuda K, Arai N, Wakimoto N, Matsushita T. Mini-incision posterior approach for total hip arthroplasty. Int Orthop. 2004;28:214–217. doi: 10.1007/s00264-004-0570-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O’Brien S, Beverland D. A minimal-incision technique in total hip arthroplasty does not improve postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87(4):701–710. doi: 10.2106/JBJS.D.02645. [DOI] [PubMed] [Google Scholar]
- 36.Petitti DB. Approaches to heterogeneity in meta-analysis. Stat Med. 2001;20:3625–3633. doi: 10.1002/sim.1091. [DOI] [PubMed] [Google Scholar]
- 37.Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, Colthart IR, Ross S, Shepherd SM, Russell D. Factors that limit the quality, number and progress of randomized controlled trials. Health Technol Assess. 1999;3:1–143. [PubMed] [Google Scholar]
- 38.Procyk S. Initial results with a mini-posterior approach for total hip arthroplasty. Int Orthop. 2007;31(Suppl 1):S17–S20. doi: 10.1007/s00264-007-0435-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Purkayastha S, Tilney HS, Georgiou P, Athanasiou T, Tekkis PP, Darzi AW. Laparoscopic cholecystectomy versus mini-laparotomy cholecystectomy: a meta-analysis of randomised control trials. Surg Endosc. 2007;21:1294–1300. doi: 10.1007/s00464-007-9210-3. [DOI] [PubMed] [Google Scholar]
- 40.Reininga IH, Wagenmakers R, Akker-Scheek I, Stant AD, Groothoff JW, Bulstra SK, Zijlstra W, Stevens M. Effectiveness of computer-navigated minimally invasive total hip surgery compared to conventional total hip arthroplasty: design of a randomized controlled trial. BMC Musculoskelet Disord. 2007;11:4. doi: 10.1186/1471-2474-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sculco TP, Jordan LC, Walter WL. Minimally invasive total hip arthroplasty: The Hospital for Special Surgery experience. Orthop Clin North Am. 2004;35(2):137–142. doi: 10.1016/S0030-5898(03)00116-0. [DOI] [PubMed] [Google Scholar]
- 42.Sherry E, Egan M, Henderson A, Warnke PH. Minimally invasive techniques for total hip arthroplasty. J Bone Joint Surg Am. 2002;84:1481. doi: 10.2106/00004623-200208000-00032. [DOI] [PubMed] [Google Scholar]
- 43.Speranza A, Iorio R, Ferretti M, Arrigo CD, Ferretti A. A lateral minimal-incision technique in total hip replacement: a prospective, randomizes, controlled trial. Hip Int. 2007;17:4–8. doi: 10.1177/112070000701700102. [DOI] [PubMed] [Google Scholar]
- 44.Swanson TV. Posterior single-incision approach to minimally invasive total hip arthroplasty. Int Orthop. 2007;31(Suppl 1):S1–S5. doi: 10.1007/s00264-007-0436-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Szendrõi M, Sztrinkai G, Vass R, Kiss J. The impact of minimally invasive total hip arthroplasty on the standard procedure. Int Orthop. 2006;30:167–171. doi: 10.1007/s00264-005-0049-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Teet JS, Skinner HB, Khoury L. The effect of the “mini” incision in total hip arthroplasty on component position. J Arthroplasty. 2006;21:503–507. doi: 10.1016/j.arth.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 47.Vavken P, Kotz R, Dorotka R. Minimally invasive hip replacement—a meta-analysis. Z Orthop Unfall. 2007;145:152–156. doi: 10.1055/s-2007-965170. [DOI] [PubMed] [Google Scholar]
- 48.Wenz JF, Gurkan I, Jibodh SR. Mini-incision total hip arthroplasty: a comparative assessment of perioperative outcomes. Orthopedics. 2002;25:1031–1043. doi: 10.3928/0147-7447-20021001-14. [DOI] [PubMed] [Google Scholar]
- 49.Wright JM, Crockett HC, Delgado S, Lyman S, Madsen M, Sculco TP. Mini-incision for total hip arthroplasty: a prospective, controlled investigation with 5-year follow-up evaluation. J Arthroplasty. 2004;19:538–545. doi: 10.1016/j.arth.2003.12.070. [DOI] [PubMed] [Google Scholar]
- 50.Yan ZQ, Chen YS, Yang Y, Li WJ, Chen ZR, Zhang GJ. Two-incision minimal invasive approach for total hip replacement. Fudan Univ J Med Sci. 2005;32:557–560. [Google Scholar]
- 51.Zhang XL, He YH, Wang Q, Jiang Y, Sui SP, Zeng BF. Minimally invasive incision in total hip arthroplasty for displaced femoral neck fractures in the elderly. Chin J Orthop Trauma. 2004;6:506–508. [Google Scholar]
- 52.Zhang XL, Wang Q, Jiang Y, Zeng BF. Minimally invasive total hip arthroplasty with anterior incision. Zhonghua Wai Ke Za Zhi. 2006;44:512–515. [PubMed] [Google Scholar]