Abstract
Computer navigation assistance in total knee arthroplasty (TKA) results in consistently accurate alignment of prostheses. We aimed to compare the outcome of computer-navigated and conventional TKA and to analyse the radiologically malaligned knees. We analysed 637 primary TKA, carried out by a single surgeon, over five consecutive years and divided them into two cohorts: group 1 = STA (standard instrumentation) and group 2 = CAS (computer-assisted surgery). There was no significant difference between the average Oxford Knee Scores (OKS) of the two groups at any time from one to five years. However, the malaligned TKA at three years had a worse OKS. At medium term there is no difference in clinical outcome measures that can be attributed to the surgeon having used computer-assisted navigation for TKA. But group 1, having a higher proportion of malaligned TKA, might show worsening of OKS at long term.
Résumé
La navigation dans la prothèse totale du genou permet d’avoir une amélioration de l’alignement articulaire. Nous avons comparé le devenir d’une prothèse totale du genou naviguée, ou traitée par voie conventionnelle, avec une analyse radiologique des genoux présentant une déviation externe en valgus. Nous avons analysé 637 prothèses totales du genou, réalisées par le même chirurgien sur 5 ans et divisées en deux groupes: le groupe 1 STA avec une instrumentation standard et le groupe 2 CAS avec navigation. Il n’y a pas de différence significative au niveau des scores d’Oxford (OKS) dans les deux groupes sur une période de 1 à 5 ans. Cependant, les genoux présentant un défaut d’axe post-opératoire ont un résultat OKS dégradé au bout de la troisième année. A moyen terme, il n’y a pas de différence sur le devenir clinique mais le groupe 1 a néanmoins une proportion beaucoup plus importante de genoux présentant une déviation axiale ce qui peut influer, de façon négative sur le score OKS à long terme.
Introduction
Total knee arthroplasty (TKA) undertaken with the assistance of computer navigation provides greater consistency in accurate component alignment than TKA undertaken with conventional instruments [3, 4, 8, 10]. Prosthetic component malalignment in TKA has been shown to result in poorer outcome in the long term [17]. Thus, it may be anticipated that computer-navigated knees will have a lower long-term failure rate than non-navigated knees. The relative novelty of navigation means that it will be some years before such predictions can be tested.
To date, short-term studies have not demonstrated any functional difference between computer-navigated and non-navigated TKA. Furthermore, these studies were conducted on small cohorts [18] and have been weak in terms of statistical power. Our aim was to undertake a conclusive comparative outcome of the two techniques of TKA, with adequate statistical power, at short term, and to investigate whether any difference is generated at midterm. We also aimed to investigate whether patients with malaligned TKA are aware of any difference in their functional outcomes at time points before failure might be anticipated. We hypothesised that (a) computer navigation-assisted TKA and (b) well-aligned TKA would have better functional outcomes as opposed to standard TKA at midterm follow-up.
Materials and methods
Our arthroplasty outcome programme gathers data on all patients who have had their joints replaced at our hospital. A pre-operative Oxford Knee Score (OKS) is obtained at the time of the patients’ pre-admission assessment. After surgery, postal questionnaires are sent at each anniversary of the index operation. In addition, the patients are invited to attend outcome clinic appointments at designated intervals. The first clinic review is currently undertaken at three years post-operatively. The review programme is run by the Orthopaedic Research and Education unit. Members of staff are available to answer telephone queries regarding the questionnaire. The outcomes coordinator also identifies patients who fail to return their questionnaires and telephones them to request that they complete and return the forms to us. This process ensures a return rate of over 90%.
Patients are asked to complete the forms at home so that the effect of interviewer bias is minimised. The operating surgeons are not involved in the collection of the pre-operative baseline OKS or in the review process. If any problem is identified, an appointment is arranged with the operating consultant. All the information collected from the questionnaires is transcribed onto an electronic database (Microsoft Access, Microsoft® Corp.). Queries can then be made to get the desired information.
We have undertaken a retrospective analysis of all primary TKA performed by a single surgeon (AA) for a period of five years from October 2002 to October 2007. This comprised 637 TKA in 540 patients. Only the patients with primary osteoarthritis who underwent TKA with the TC Plus SB™ type of knee prostheses (Smith & Nephew Orthopaedics, London, UK) were included for further analysis. Patients who underwent TKA for other aetiologies, e.g. rheumatoid arthritis, and those in which other implant types were used, were excluded. This left us with 565 TKA. These were then divided into two groups: in group 1, TKA was performed with standard instruments (STA) in 302 knees. In group 2, TKA was undertaken with the assistance of computer navigation (CAS) on 263 knees. The navigation used was PiGalileo™ (Plus Orthopedics, Swindon, UK). This is an imageless system which incorporates a mini-robot that positions the femoral cutting jig. Additionally, the surgeon has the option of making fine adjustments to the cuts suggested by the robot.
Patients were assigned to navigation or standard methods by the scheduling team depending on the availability of instruments for computer navigation. No other factors were involved in assigning patients to either technique and the surgical team had no prior knowledge of the allocation. We obtained the OKS in both the groups pre-operatively and at yearly intervals after the operation. At each time point, we have undertaken a comparative analysis between the two groups.
Clinical and radiological examinations were performed at the three-year clinical follow-up. The X-rays are all obtained as per a standard protocol. A long-leg anteroposterior (AP) standing film with both feet placed together and pointing forwards is taken followed by a lateral X-ray with knee flexed and a patellar axis view. The radiographic alignment of the tibial prostheses on the three-year AP films was measured by two observers who were blinded to the surgical technique employed. Furthermore, each observer took two independent readings of all films. The tibial components were studied and those greater than 3° malaligned with respect to the mechanical axis identified. The average OKS of these less well-aligned TKA was compared with that of all the others at the same time point.
Statistical methods
For the power analysis and sample size calculations, the minimum effective difference in average OKS was taken as five. To arrive at this, random comparisons between data of OKS from large numbers of TKA performed by various different surgeons on our outcome programme database were performed. This outcome programme was begun in 1998 and has generated more than 4,000 OKS assessments. The average OKS values pre- and post-operatively and the standard deviations thereof, from this study, are consistent with corresponding figures from the large data set. Statistical power of greater than 80% has been achieved for our comparative analyses up to three years post-operative results. Student’s t-test was employed for the comparison at each time point, with a p level < 0.05 being considered as significant.
Results
Both surgical and non-surgery-related complications were found to be similar in both groups. The CAS group had one superficial infection, one re-exploration for a haematoma with a subsequent delayed wound healing and one nerve palsy. The STA group had one deep infection, one superficial infection with delayed wound healing and one nerve palsy. There were two revision operations performed, one in each group, and both these involved only resurfacing of a previously unresurfaced patella.
The numbers and demographic details of the patients in both groups are shown in Table 1. The age at operation was similar in both groups. They had comparable American Society of Anesthesiologists (ASA) grades at operation. There was no statistically significant difference (p = 0.87) between mean pre-operative OKS in both groups.
Table 1.
Pre-operative status of groups 1 (CAS) and 2 (STA)
| CAS | STA | |
|---|---|---|
| No. of TKA | 263 (148 women, 115 men) | 302 (170 women, 132 men) |
| Average age at op. (years) | 72.6 | 71.7 |
| Average OKS | 40.4 (range: 18–57, SD: 7.84) | 39.9 (range: 16–55, SD: 7.54) |
At the post-operative one, two, three, four and five-year points we had 434, 289, 179, 84 and 28 complete returned questionnaires, respectively. Table 2 shows the number of OKS obtained from patients in each group, average OKS, range, standard deviation and p values obtained from the t-test at each of the post-operative time points.
Table 2.
Comparison of average OKS between the CAS and STA groups
| No. of OKS assessments | Mean & range | SD | p value (t-test) | ||
|---|---|---|---|---|---|
| 1 year | STA | 246 | 25.84 (12–59) | 9.82 | 0.72 |
| CAS | 188 | 24.43 (12–54) | 9.05 | ||
| 2 years | STA | 166 | 24.89 (12–58) | 9.88 | 0.62 |
| CAS | 123 | 24.48 (12–53) | 9.25 | ||
| 3 years | STA | 102 | 24.51 (12–49) | 9.69 | 0.33 |
| CAS | 77 | 25.66 (12–52) | 10.37 | ||
| 4 years | STA | 51 | 24.26 (12–57) | 10.67 | 0.97 |
| CAS | 33 | 24.18 (12–45) | 9.07 | ||
| 5 years | STA | 15 | 25.21 (12–48) | 10.85 | 0.66 |
| CAS | 13 | 26.9 (12–45) | 9.26 | ||
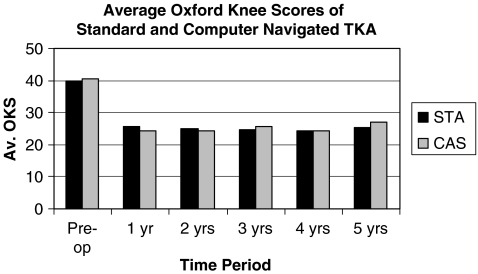
Figure 1 shows the average OKS of both groups 1 and 2 over time. The improvement in the OKS at the one-year post-operative time point was maintained in the subsequent period.
Fig. 1.
Average Oxford Knee Scores of standard and computer-navigated TKA
We had three-year post-operative clinical and radiological data for 84 TKA from group 1 (STA) and 67 TKA from group 2 (CAS). The average Knee Society Scores were as follows: group 1 (STA): mean combined score 162, mean knee score 85.8, mean function score 76.2 and group 2 (CAS): mean combined score 164.9, mean knee score 86.5, mean function score 78.4. There was no significant difference between the groups.
The radiographic analysis revealed that 13 of 84 TKA (15.5%) in the STA group (1) were aligned beyond 3° of the mechanical axis. In the CAS group (2), 2 of 67 (2.9%) were beyond ± 3° from the mechanical axis. The mean OKS of the total 15 ‘malaligned’ TKA was 29.5 (range: 13–52, SD: 23.3). Mean OKS of all the remaining TKA that were well-aligned was 23.32 (range: 12– 40, SD: 8.35). In view of the large standard deviation in the malaligned group, a t-test for statistical comparison was not deemed appropriate.
Discussion
The use of computer navigation for TKA in recent years has brought about critical evaluation of radiological parameters with great precision [2]. Assistance of computer navigation has been conclusively proved to provide consistent and superior alignment of prostheses in TKA, even when tested with different systems and different surgeons with no specialisation in surgical navigation [13]. However, to the knowledge of the authors, there are no published data yet on longitudinal analysis of clinical outcome measures of computer-navigated TKA.
The OKS [5, 6] provides a consistent patient-administered self-assessment [12] that patients are generally willing to complete at regular intervals and has been shown to provide a useful assessment of patient disability due to the knee being assessed. It has been ranked as the best disease-specific patient questionnaire by a large study on patients from the Swedish Knee Arthroplasty Registry [7]. Use of this simple measure has provided us with the largest sample size among published comparative studies between computer-navigated and conventional TKA.
Our outcome programme has enabled measurement of the OKS at the pre-operative stage and at regular time intervals thereafter. Pre-operative analysis of the OKS confirms equality of the two groups for further comparison. Behaviour of Oxford hip scores over time has been reported [9]. Scores were seen to level of from a year after operation. Our study shows that OKS follow a similar pattern for both computer-navigated and standard knees.
In order to achieve a statistical power of 80%, one needs a minimum sample size of 57 in each group. Our analysis of the OKS shows no statistical difference between the navigated and non-navigated knees up to five years. Again, while our data have achieved statistical power up to three years, the numbers that we have at four and five years are only comparable to those of previous studies [14, 15]. The midterm data do however, provide an indication that longer term studies will be required to eventually prove or disprove our hypothesis. We have employed a rigid protocol for all X-rays undertaken at the three-year follow-up and have had measurements from two observers in order to reduce error, as financial and time constraints did not permit use of advanced imaging techniques.
With the use of computer navigation, we are now in a position to evaluate less precisely aligned TKA in greater detail. The incidence of malaligned and well-aligned knees in both groups of our study are consistent with previously published results [1]. In their long-term evaluation of TKA, Jeffery et al. [11] identified that prosthetic loosening increased significantly with component malalignment in excess of 3°. Rand and Coventry [16] found survivorship to be improved when the mechanical axis was within 0–4°. Thus, comparison of TKA with well-aligned components against TKA with malaligned components should reveal measurable differences. At present, we do not know whether these differences will be reflected in the OKS, at what stage and whether a consistent pattern can be identified. Stulberg [19] has proved that use of computer navigation betters a single surgeon’s consistency in prosthetic alignment during the performance of conventional TKA. There is hence a fair argument for the continued use of computer navigation assistance in TKA.
Conclusion
Thus, this study demonstrates that there is no difference in functional outcome between TKA undertaken with computer navigation assistance and standard instrumentation at midterm follow-up. But TKA that are not well-aligned fare worse than those undertaken with computer navigation which have a very high proportion of accurately aligned knees. Our hypothesis (a) was refuted and hypothesis (b) was affirmed. However, longer term follow-up will be required to establish whether component malalignment will be associated with premature deterioration of the OKS.
Acknowledgements
Mrs. June Riordan, Outcomes Programme Co-Ordinator, St. Helier Hospital and Mr. Pradeep B. Moonot, Clinical Research Fellow, The South West London Elective Orthopaedic Centre.
References
- 1.Bäthis H, Perlick L, Tingart M, et al. Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86(5):682–687. doi: 10.1302/0301-620X.86B5.14927. [DOI] [PubMed] [Google Scholar]
- 2.Bejek Z, Sólyom L, Szendrõi M. Experiences with computer navigated total knee arthroplasty. Int Orthop. 2007;31(5):617–622. doi: 10.1007/s00264-006-0254-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bolognesi M, Hofmann A. Computer navigation versus standard instrumentation for TKA: a single-surgeon experience. Clin Orthop Relat Res. 2005;440:162–169. doi: 10.1097/01.blo.0000186561.70566.95. [DOI] [PubMed] [Google Scholar]
- 4.Chauhan S, Clark G, Lloyd S, Scott R, et al. Computer-assisted total knee replacement. A controlled cadaver study using a multi-parameter quantitative CT assessment of alignment (the Perth CT Protocol) J Bone Joint Surg Br. 2004;86(6):818–823. doi: 10.1302/0301-620X.86B6.15456. [DOI] [PubMed] [Google Scholar]
- 5.Davies AP. Rating systems for total knee replacement. Knee. 2002;9(4):261–266. doi: 10.1016/S0968-0160(02)00095-9. [DOI] [PubMed] [Google Scholar]
- 6.Dawson J, Fitzpatrick R, Murray D, et al. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80(1):63–69. doi: 10.1302/0301-620X.80B1.7859. [DOI] [PubMed] [Google Scholar]
- 7.Dunbar MJ, Robertsson O, Ryd L, Lidgren L. Appropriate questionnaires for knee arthroplasty. Results of a survey of 3600 patients from The Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br. 2001;83(3):339–344. doi: 10.1302/0301-620X.83B3.11134. [DOI] [PubMed] [Google Scholar]
- 8.Fehring TK, Mason JB, Moskal J, Pollock DC, Mann J, Williams VJ. When computer-assisted knee replacement is the best alternative. Clin Orthop Relat Res. 2006;452:132–136. doi: 10.1097/01.blo.0000229363.50361.25. [DOI] [PubMed] [Google Scholar]
- 9.Field RE, Cronin MD, Singh PJ. The Oxford hip scores for primary and revision hip replacement. J Bone Joint Surg Br. 2005;87(5):618–622. doi: 10.1302/0301-620X.87B5.15390. [DOI] [PubMed] [Google Scholar]
- 10.Haaker R, Stockheim M, Kamp M, et al. Computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res. 2005;433:152–159. doi: 10.1097/01.blo.0000150564.31880.c4. [DOI] [PubMed] [Google Scholar]
- 11.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 12.Liow RY, Walker K, Wajid MA, et al. Functional rating for knee arthroplasty: comparison of three scoring systems. Orthopedics. 2003;26(2):143–149. doi: 10.3928/0147-7447-20030201-15. [DOI] [PubMed] [Google Scholar]
- 13.Maculé-Beneyto F, Hernández-Vaquero D, Segur-Vilalta JM, et al. Navigation in total knee arthroplasty. A multicenter study. Int Orthop. 2006;30(6):536–540. doi: 10.1007/s00264-006-0126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martin A, Strempel A. Two-year outcomes of computed tomography-based and computed tomography free navigation for total knee arthroplasties. Clin Orthop Relat Res. 2006;449:275–282. doi: 10.1097/01.blo.0000218738.69247.d8. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto T, Tsumura N, Kurosaka M, et al. Clinical values in computer-assisted total knee arthroplasty. Orthopedics. 2006;29:1115–1120. doi: 10.3928/01477447-20061201-04. [DOI] [PubMed] [Google Scholar]
- 16.Rand JA, Coventry MB. Ten-year evaluation of geometric total knee arthroplasty. Clin Orthop Relat Res. 1988;232:168–173. [PubMed] [Google Scholar]
- 17.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 18.Spencer JM, Chauhan SK, Sloan K, Taylor A, Beaver RJ. Computer navigation versus conventional total knee replacement: no difference in functional results at two years. J Bone Joint Surg Br. 2007;89(4):477–480. doi: 10.1302/0301-620X.89B4.18094. [DOI] [PubMed] [Google Scholar]
- 19.Stulberg SD. How accurate is current TKR instrumentation? Clin Orthop Relat Res. 2003;416:177–184. doi: 10.1097/01.blo.0000093029.56370.0f. [DOI] [PubMed] [Google Scholar]