Abstract
Anterior cervical decompression and fusion (ACDF) is the standard for cervical discectomies. With the full-endoscopic anterior cervical discectomy (FACD) a minimally invasive procedure is available. The objective of this prospective, randomised, controlled study was to compare the results of FACD with those of ACDF in mediolateral soft disc herniations. A total of 103 patients with ACDF or FACD were followed up for two years. In addition to general parameters specific measuring instruments were used. Postoperatively 85.9% of the patients no longer had arm pain, and 10.1% had occasional pain. There were no significant clinical differences between the decompression with or without fusion. The full-endoscopic technique afforded advantages in operation technique, rehabilitation and soft tissue injury. The recorded results show that FACD is a sufficient and safe alternative to conventional procedures when the indication criteria are fulfilled. At the same time, it offers the advantages of a minimally invasive intervention.
Résumé
La décompression cervicale antérieure avec greffe (ACDF) est un standard de la chirurgie cervicale avec discectomies. La discectomie endoscopique FACD par voie mini-invasive est également possible. L’objectif de cette étude prospective randomisée est de comparer les résultats de cette technique endoscopique mini-invasive FACD avec la technique classique ACDF. 103 patients ayant bénéficié soit d’une ACDF soit d’une FACD ont été suivis pendant une moyenne de deux ans. après l’intervention, 85,9% des patients ne présentent aucune douleur au niveau brachial et 10,1% des douleurs occasionnelles. Il n’y a pas de différence significative que l’on ait réalisé ou non une greffe. La technique par endoscopie présente des avantages pratiques notamment en ce qui concerne la rééducation et les lésions des tissus en post-opératoires. le résultat montre que la technique FACD est une technique suffisamment sûre et es-t une alternative valable à la technique conventionnelle lorsque les critères d’indication ont été respectés. Cette technique a par ailleurs les avantages de la voie mini-invasive.
Introduction
In cervical disc herniations anterior cervical decompression and fusion (ACDF) has now developed as a standard surgical procedure. It is usually described as a safe and sufficient operation with good fusion rates [1–3]. Nonetheless, specific problems may occur, such as loss in height of the intervertebral space, pseudarthroses or access complications [4–7]. Degeneration of adjacent segments is discussed as a particular disadvantage of fusion [8].
Modifications to reduce the disadvantages of ACDF have been described, such as anterior cervical decompression without fusion [9–11], anterior foraminotomy using various techniques [12, 13], endoscopic anterior transdiscal decompression [14], posterior microscope-assisted or endoscope-assisted “keyhole foraminotomy” [15] or endoscopic posterior decompression [16]. The cervical disc prosthesis is intended to combine decompression and reconstruction of the intervertebral space while preserving segment mobility [17].
Endoscopic operations have become standard in various areas, such as arthroscopy or laparoscopy. These days, all disc herniations in the lumbar spine can be operated upon with the full-endoscopic technique [18, 19]. In lateral disc herniations of the cervical spine, a full-endoscopic posterior procedure is possible [16]. Otherwise anterior, transdiscal decompressions are described in the literature [14].
The objective of this prospective, randomised, controlled study was to compare the results of cervical discectomy in mediolateral soft disc herniations using the full-endoscopic technique via an anterior approach with those of conventional microsurgical ACDF.
Materials and methods
Patient characteristics
In the prospective, randomised, controlled study we enrolled 120 patients with clinically symptomatic cervical mediolateral soft disc herniations who underwent discectomies in 2005/2006 (77 women and 43 men; age: 30–61 years; duration of pain: 4–128 days)
Study groups
Sixty patients each underwent conventional microsurgical (ACDF) or full-endoscopic anterior cervical decompression (FACD). Randomisation was not blinded, since the patients could identify the operation procedure. After determination of the general indication for surgical decompression by experienced physicians who were not involved in the operation, randomised assignment was made by non-physician study stuff. This was balanced block randomisation to the end of the study. All operations were performed by two surgeons, who have many years of experience in both techniques. The results of the study group (FACD) were compared with those of the control intervention group (ACDF). The patients were informed prior to surgery about the procedure which was to be used for them. The later examiners were not informed about which operation procedure was used. Three interventions were performed at the level C3–4 (1 × ACDF, 2 × FACD), 16 at C4–5 (9 × ACDF, 9 × FACD), 55 at C5–6 (26 × ACDF, 29 × FACD), 41 at C6–7 (21 × ACDF, 20 × FACD) and five at C7–Th1 (3 × ACDF, 2 × FACD).
Inclusion criteria
The inclusion criteria for discectomy were: unilateral radiculopathy with arm pain; on magnetic resonance imaging (MRI)/computed tomography (CT) mediolateral localised monosegmental disc herniation; segments C2–3 to C7–Th1; ventrally at least 4 mm height of the intervertebral space.
Exclusion criteria were: foraminal localisation of the disc herniation; craniocaudal sequestering more than half of the vertebral body; clear instabilities or deformities; isolated neck pain; foraminal stenosis without disc herniation; previous operation at the same segment.
Full-endoscopic instruments
The oval operation sheath surrounding the endoscope has an outer diameter of 3.8 × 6.2 mm and is inserted diagonally into the intervertebral space by means of a dilator system. The telescope can be moved within the operation sheath, sliding through toward ventral in the direction of the cord is prevented. The angle of vision of the system is 25°. The telescope contains the light conductor system, a canal for continuous irrigation and the rod lens system. Various instruments including drills up to 2.5 mm in diameter can be used (Fig. 1). All of the operating instruments and optics were products supplied by Richard Wolf GmbH (Knittlingen, Germany).
Fig. 1.

Optic in oval sheath with inserted rongeur
Operative technique
The conventional microsurgical ACDF was performed with the known standardised technique using a microscope. A polyetheretherketone (PEEK) cage was used as the intervertebral implant; there was no additional ventral plating.
For the FACD, the ventral spine was palpated contralaterally between the oesophagus/trachea and vascular nerve sheath. After a 5-mm skin incision, a thin dilator (OD 1.8 mm) was inserted into the intervertebral space. Over this, a combined dilator-sheath system was bluntly inserted, until the final oval operation sheath (oval OD 3.8 mm × 6.2 mm) lay diagonally in the intervertebral space. After insertion of the telescope, further operation was performed under visual control and continuous irrigation with 0.9% saline solution. On the side with the pathological condition, the dorsal anulus, the dorsal segments of the vertebral body or the end plates and the uncinate process were prepared. The sequestered disk material was prepared and resected, and the anulus and posterior longitudinal ligament were opened.
The operations were performed under general anaesthesia and radiographic control with the patient supine. The head was fixed in place with Mayfield clamps. The arms were positioned on either side of the body with gentle traction. Drainage was applied only in the ACDF group. All patients were given a soft brace for seven days.
Follow-up
Follow-up examinations were conducted at day one (120 patients) and at three (115 patients), six (111 patients), 12 (110 patients) and 24 (103 patients) months after surgery. All patients received the appropriate questionnaire by mail four working days in advance. They came personally to the clinic for follow-up examination. The examinations were performed by two doctors, who were not involved in the operations. In addition to general parameters, other information was obtained using the following instruments: a visual analogue scale (VAS) for neck and arm pain, the German version of the North American Spine Society Instrument (NASS) [20] and Hilibrand criteria [21] based on Smith and Robinson [22]. All patients underwent MRI/CT and X-rays at the end of the follow-up period.
Statistical analysis
The Wilcoxon rank sum test and the Mann-Whitney U test were applied for the comparison of pre- and postoperative global results and comparison of results in the group at various times. The McNemar test was used to compare the characteristics of the groups. The descriptive assessments and analytical statistics were performed depending on the group characteristics with the program package SPSS. A positive significance level was assumed at a probability of less than 0.05.
Results
Baseline characteristics
A total of 103 patients (86%) were included in follow-up after two years (49 × ACDF, 54 × FACD). The remaining cases were lost for the following reasons: one operation-unrelated death (17 months postoperative), three patients moved away and left no forwarding address and 13 patients did not respond to letters or telephone calls. The patient population was equal in the ACDF and FACD groups. There were no differences in results in relation to the individual surgeons.
Operative technique
The mean operating time in the ACDF group was 62 min (41–102) and thus significantly longer (p < 0.001) than in the FACD group at 32 min (18–51). The intra- and postoperative blood loss in the ACDF group, measured by intraoperative suctioning and postoperative drainage, was less than 10 ml. In the FACD group, there was no measurable blood loss.
In the FACD group, bone resection on the posterior vertebral body or the uncinate process was required to reach the epidural space or the foramen in 33 cases (55%) Measurement of the lavage fluid inflow and outflow showed a maximum of 10 ml remaining intracorporeally.
In the ACDF group, the bone harvested intraoperatively sufficed to fill the cage in 47 cases. Cancellous bone was obtained from the pelvis using a percutaneous technique in 13 cases.
Perioperative complications
Transient difficulty swallowing occurred in seven cases (5 × ACDF, 2 × FACD) and there were two surface haematomas in the ACDF group. No further serious complications of the types described in the literature or other problems occurred.
Ten patients (8.3%) reported pain for a maximum of two days due to the Mayfield clamp. There were no other problems with the Mayfield clamp, such as injuries or infections.
Postoperative increase in arm pain occurred four times for a maximum of ten days.
Recurrences/revisions
There were two revisions (posterior foraminotomy) in the ACDF group due to persistent arm pain. The ACDF was repeated in one patient who had clinically relevant sintering of the implant with kyphosis. The revision rate in the ACDF group was 6.1%.
In the FACD group two patients (3.7%) suffered a recurrence after a pain-free interval. One patient was revised using the same technique, the other using conventional ACDF. Two patients with persistent arm pain were revised by means of ACDF. The revision rate in the FACD group was 7.4%.
Overall, the revision rate was 6.8% (seven patients). All revision operations were performed during the follow-up observation period, the earliest after five months. The difference in the revision rate between the two groups was not significant.
Radiological findings
All patients were examined at the end of the follow-up period using MRI/CT and X-ray (99 patients without revision using ACDF). No newly occurring degeneration was found in adjacent vertebral discs. Twelve patients showed progression of pre-existing adjacent disc degeneration (9 × ACDF = 18.8%; 3 × FACD = 5.9%, not significant).
Ten patients presented with an increase in the kyphosis angle in the operated segment (ACDF: four patients = 8.3%, ∅ 5.9°; FADC: six patients = 11.8%, ∅ 5°). This was not significant within or between the groups. The height of the intervertebral space decreased in both groups (ACDF: 6.1 to 5.0 mm; FACD: 5.3 to 4.1 mm). This was significant within both groups (p < 0.05). The absolute height of the intervertebral space was significantly higher in the ACDF group (∅ 0.9 mm, p < 0.05). There was no significant relation between kyphosis, high intervertebral space and the clinical outcome.
There was no spontaneous fusion in any patient in the FACD group; 21 patients (24%) showed signs of advancing degeneration in the disc. In the ACDF group there were no clear radiological signs of bony intrusion in the cage without correlation to the clinical result in nine (18.8%) patients.
Clinical outcome
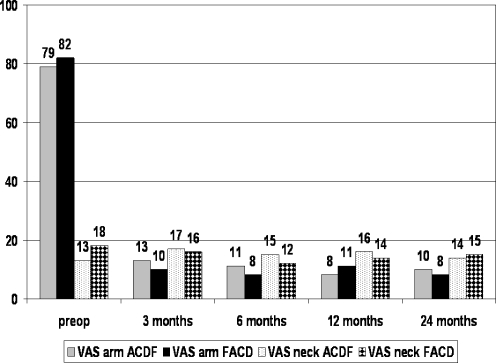
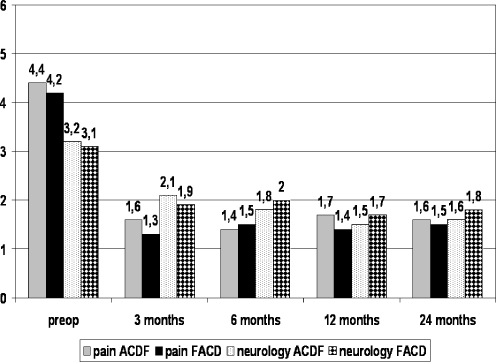
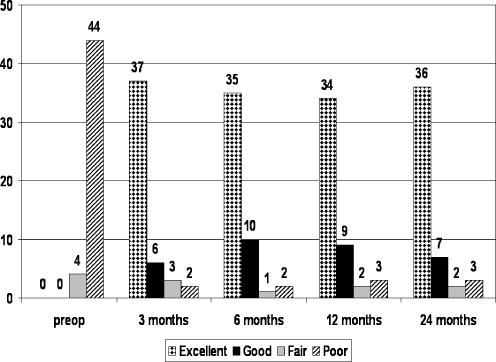
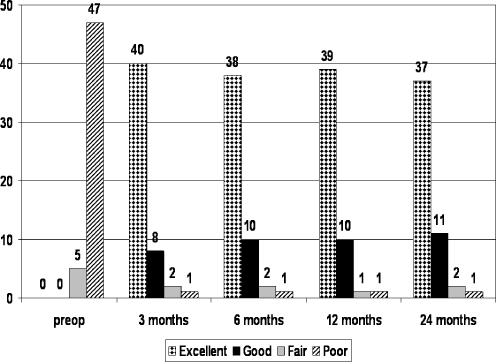
Excluding the patients revised by means of ACDF, 99 patients remained after two years. Figure 2 shows the course of arm and neck pain in both groups, rated using the VAS. Figure 3 shows the values of the NASS score, the Hilibrand criteria for the ACDF group are shown in Fig. 4 and the FACD group in Fig. 5. Overall, the measuring instruments show constant and significant (p < 0.001) improvement in arm pain and activities of everyday living in both groups. After two years 85 patients (85.9%) no longer had arm pain, ten (10.1%) occasional pain or clearly reduced pain and four (4%) no essential improvement. The differences in results between the groups were not significant. Six patients (6.1%) suffered progressive neck pain (4 × ACDF, 2 × FACD).
Fig. 2.
Mean values of VAS arm and neck in the ACDF and FACD groups
Fig. 3.
Mean values of NASS pain and neurology in the ACDF and FACD groups
Fig. 4.
Clinical results according to Hilibrand criteria in the ACDF group
Fig. 5.
Clinical results according to Hilibrand criteria in the FACD group
Seven patients (of 103) (5.7%) (3 × ACDF, 4 × FACD) underwent revision due to persistent arm pain, recurrences or failure of the implant. Overall, 11 patients (11.1%) had poor results (4 × no essential improvement, 7 × revision) (6 × ACDF, 5 × FACD). . Of ten patients, 92 (89.3%) reported subjective satisfaction and would undergo the procedure again (43 × ACDF = 87.8%, 49 × FACD = 90.7%). Neurological deficits were significantly (p < 0.001) reduced when the patient’s history of pain was less than 15 days.
All results were independent of general parameters such as gender, age, height, weight, occupation or secondary illnesses. The maximum time in hospital was seven days in the ACDF group and three days in the FACD group. After three months, patients had returned to work or were able to work (30 × ACDF = 62.6%; 43 × FACD = 84.3%) (p < 0.01).
Discussion
ACDF is the standard procedure for treatment of cervical herniated discs [1–3] and produces good results. Problems with ACDF may include for example loss of height in the intervertebral space, pseudarthroses, access complications and adjacent degeneration due to the loss of mobility [4–8]. To reduce these disadvantages different modifications and techniques from anterior and posterior with or without reconstruction of the intervertebral space have been described [9, 10, 12–14, 16]. Questions about the progression of segmental sintering and kyphosis and their clinical relevance must be discussed, especially in the anterior techniques without reconstruction of the intervertebral space. These questions cannot be clearly answered as yet according to criteria of evidence-based medicine [9, 10, 23].
The good clinical results of ACD with or without fusion described in the literature were achieved in our study in the ACDF and FACD groups [1]. A significant and constant improvement was achieved in both groups without significant differences. In the FACD group soft tissue damage, operating time and complications are reduced compared to the conventional procedures [1, 5, 10, 24]. Rehabilitation was rapid, and no specific operation-related measures were required. The rate of complications and revisions is comparable to published results without significant differences in either group [1, 5, 10]. The recurrence rate of 3.7% in the FACD group is comparable to the results of other techniques without complete discectomy and reconstruction of the disc space [16].
Radiologically, there was a non-significant increase in the segmental kyphosis angle in both groups. The mean decrease in the height of the intervertebral space was significant in both groups. The absolute height of the intervertebral space was significantly higher in the ACDF group, which can be explained by the direct postoperative reconstruction [11]. Generally, comparisons of ventral decompressions with and without fusion in the literature describe higher values for decompression alone as occurred in the FACD group in this study. However, complete discectomy with curettage of the end plate is performed in studies reported in the literature [10, 11]. This probably promotes the described high rates of spontaneous fusions, which did not occur in this study. With additional fusion, too, sintering and kyphosis are described throughout the literature which sometimes lie above the values found in this study in the ACDF and FACD groups [10, 11, 25, 26].
The goal of surgical treatment of cervical disc herniations is to achieve sufficient decompression with minimisation of operation-induced soft tissue injury and its sequelae. This study shows that predictable adequate decompression can be achieved by FACD under continuous visualisation in a short operation time. Comparison of the two techniques and with the literature shows, in our opinion, the following advantage for FACD: facilitation for the surgeon by excellent presentation of the anatomical structures; good illumination and expanded field of vision thanks to the 25°-optics; economical procedure thanks to short operation time, rapid rehabilitation and low postoperative costs of care; reduced soft tissue damage; easier revision operations; image monitoring as the basis for training of assistants; and high patient acceptance. The following are cited as specific disadvantages: limited possibility to extend the operation in the event of unforeseen difficulties; only direct and no indirect decompression by reconstruction of the intervertebral space, technically limited procedure in the direction of the foramen, only mediolateral soft disc herniations accessible; possibility of recurrences; and a difficult learning curve.
References
- 1.Fraser JF, Hartl R. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine. 2007;6:298–303. doi: 10.3171/spi.2007.6.4.2. [DOI] [PubMed] [Google Scholar]
- 2.Baba H, Furusawa N, Tanaka Y, Wada M, Imura S, Tomita K. Anterior decompression and fusion for cervical myeloradiculopathy secondary to ossification of the posterior ligament. Int Orthop. 1994;18:204–209. doi: 10.1007/BF00188323. [DOI] [PubMed] [Google Scholar]
- 3.Chen Y, Chen D, Wang X, Lu X, Guo Y, He Z, Tian H (2008) Anterior corperectomy and fusion for severe ossification of posterior longitudinal ligament in the cervical spine. Int Orthop April 12 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 4.Tureyen K. Disc height loss after anterior cervical microdiscectomy with titanium intervertebral cage fusion. Acta Neurochir (Wien) 2003;145:565–569. doi: 10.1007/s00701-003-0050-1. [DOI] [PubMed] [Google Scholar]
- 5.Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, Lee GP, Robinson JS. Anterior cervical discectomy and fusion associated complications. Spine. 2007;32:2310–2317. doi: 10.1097/BRS.0b013e318154c57e. [DOI] [PubMed] [Google Scholar]
- 6.Naito M, Kurose S, Oyama M, Sugioka Y. Anterior cervical fusion with the Caspar instrumentation system. Int Orthop. 1993;17:73–76. doi: 10.1007/BF00183545. [DOI] [PubMed] [Google Scholar]
- 7.Suk KS, Kim KT, Lee SH, Park SW. Prevertebral soft tissue swelling after anterior cervical discectomy and fusion with plate fixation. Int Orthop. 2006;30:290–294. doi: 10.1007/s00264-005-0072-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maiman DJ, Kumaresan S, Yoganadan N, Pintar FA. Biomechanical effect of anterior cervical spine fusion on adjacent segments. Biomed Mater Eng. 1999;9:27–38. [PubMed] [Google Scholar]
- 9.Savolainen S, Rinne J, Hernesniemi J. A prospective randomized study of anterior single-level cervical disc operations with long-term follow-up: surgical fusion is unnecessary. Neurosurgery. 1998;43:51–55. doi: 10.1097/00006123-199807000-00032. [DOI] [PubMed] [Google Scholar]
- 10.Hauerberg J, Kosteljanetz M, Boege-Rasmussen T, Dons K, Gideon P, Springborg JB, Wagner A. Anterior cervical discectomy with or without fusion with ray titanium cage: a prospective randomized clinical study. Spine. 2008;33:458–464. doi: 10.1097/BRS.0b013e3181657dac. [DOI] [PubMed] [Google Scholar]
- 11.Oktenoglu T, Cosar M, Ozer AF, Iplikcioglu C, Sasani M, Canbulat N, Bavbek C, Saioglu C. Anterior cervical microdiscectomy with or without fusion. J Spinal Disord Tech. 2007;20:361–368. doi: 10.1097/BSD.0b013e31802f80c8. [DOI] [PubMed] [Google Scholar]
- 12.Saringer WF, Reddy B, Nobauer-Huhmann I, Regatschnig R, Reddy M, Tschabitscher M, Knosp E. Endoscopic anterior cervical foraminotomy for unilateral radiculopathy: anatomical morphometric analysis and preliminary clinical experience. J Neurosurg. 2003;98:171–180. doi: 10.3171/spi.2003.98.2.0171. [DOI] [PubMed] [Google Scholar]
- 13.Choi G, Lee SH, Bhanot A, Chae YS, Jung B, Lee S. Modified transcorporeal anterior cervical microforaminotomy for cervical radiculopathy: a technical note and early results. Eur Spine J. 2007;16:1387–1393. doi: 10.1007/s00586-006-0286-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahn Y, Lee SH, Chung SE, Park HS, Shin SW. Percutaneous endoscopic cervical discectomy for discogenic cervical headache due to soft disc herniation. Neuroradiology. 2005;47:924–930. doi: 10.1007/s00234-005-1436-y. [DOI] [PubMed] [Google Scholar]
- 15.Roh SW, Kim DH, Cardoso AC, Fessler RG. Endoscopic foraminotomy using MED system in cadaveric specimens. Spine. 2000;25:260–264. doi: 10.1097/00007632-200001150-00019. [DOI] [PubMed] [Google Scholar]
- 16.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine. 2008;33:940–948. doi: 10.1097/BRS.0b013e31816c8b67. [DOI] [PubMed] [Google Scholar]
- 17.Yang YC, Nie L, Cheng L, Hou Y (2008) Clinical and radiographic reports following cervical arthroplasty: a 24-month follow-up. Int Orthop May 22 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 18.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine. 2008;33:931–939. doi: 10.1097/BRS.0b013e31816c8af7. [DOI] [PubMed] [Google Scholar]
- 19.Ruetten S, Komp M, Merk H, Godolias G Recurrent lumbar disc herniation following conventional discectomy: A prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J Spinal Disord Tech (in press) [DOI] [PubMed]
- 20.Pose B, Sangha O, Peters A, Wildner M. Validation of the North American Spine Society Instrument for assessment of health status in patients with chronic backache (in German) Z Orthop. 1999;137:437–441. doi: 10.1055/s-2008-1037387. [DOI] [PubMed] [Google Scholar]
- 21.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlmann HH. Radiculopathy and myelopathy at segments adjacent to the site of previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Smith GW, Robinson RA. The treatment of certain cervical spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A:607–624. [PubMed] [Google Scholar]
- 23.Abd-Alrahman N, Dokmak AS, Abou-Madawi A. Anterior cervical discectomy (ACD) versus anterior cervical fusion (ACF), clinical and radiological outcome study. Acta Neurochir (Wien) 1999;141:1089–1092. doi: 10.1007/s007010050487. [DOI] [PubMed] [Google Scholar]
- 24.Peng-Fei S, Yu-Hua J. Cervical disc prosthesis replacement and interbody fusion: a comparative study. Int Orthop. 2008;32:103–106. doi: 10.1007/s00264-006-0287-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murphy MA, Trimble MB, Piedmonte MR, Kalfas IH. Changes in the cervical foraminal area after anterior discectomy with and without a graft. Neurosurgery. 1994;34:93–96. doi: 10.1097/00006123-199401000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Liao JC, Niu CC, Chen WJ, Chen LH. Polyetheretherketone (PEEK) cage filled with cancellous allograft in anterior cervical discectomy and fusion. Int Orthop. 2008;32:643–648. doi: 10.1007/s00264-007-0378-x. [DOI] [PMC free article] [PubMed] [Google Scholar]