Abstract
The Anterior Pelvic Plane (APP), defined by the anterior superior iliac spines and the pubic tubercle, was commonly used as reference for positioning and postoperative evaluation of the orientation of the acetabular cup in total hip arthroplasty. APP was assumed to be vertical, but was not observed always so, mostly because of associated spinal diseases inducing perturbations in the harmony of the sagittal balance of the pelvi-spinal unit. Consequently a sagittal rotation of the pelvis occurs, and so a tilt of the APP which alters directly the orientation of the cup in upright position. An analysis of the APP tilt related to the sagittal balance of the spine was provided and its implication on the cup orientation. It appeared essential for an individual adjustment of the cup positioning to avoid a functional mal-position which can lead to an increased risk of dislocation and impingement.
Résumé
Le plan antérieur pelvien (APP) définit par les crêtes iliaques et le pubis est communément appelé plan de référence pour le positionnement et l'orientation de la cupule acétabulaire dans les prothèses totales de hanche. Ce plan peut être modifié par la position verticale et du fait de pathologies associées au niveau de la colonne vertébrale entraînant une perturbation des courbures et de la balance pelvienne. En conséquence, une rotation sagittale du pelvis peut survenir avec conséquences sur le plan pelvien antérieur APP. Ceci peut avoir des conséquences directes sur l'orientation de la cupule en position debout. Une analyse de ce plan pelvien antérieur APP et des modifications entraînées par la balance pelvienne sont indispensables. Il apparaît essentiel d'ajuster le positionnement de la cupule de façon à éviter une mal position qui peut être responsable d'un risque accru de luxations ou de conflits.
Introduction
Acetabular component mal-positioning in total hip arthroplasty (THA) has for a long time been recognised as an important cause of dislocation, implant impingement, loss of range of movement, and can lead to increased and premature wear [7, 8, 16]. In a review of 300 THA, Lewinnek defined the “safe zone” as an inclination angle of 40 ± 10° and an anteversion of 15 ± 0° [14]. For this study, the cup anteversion was measured from the elliptical appearance of the circular marker wire on precisely oriented antero-posterior roentgenograms in supine position (Appendix-1). Therefore, he used a device consisting of three legs resting on the pubis and the antero-superior iliac spines (ASISs) and a bubble level to position the pelvis parallel to the film [14]. Hence the anterior pelvic plane (APP), or the Lewinnek’s plane was established, defined by the line joining both ASISs and the pubic symphysis. The APP was universally admitted as reference to define the target position for acetabular cup insertion and for the retrospective evaluation of its orientation.
According to the definitions of the Scoliosis Research Society (SRS) [19], this APP was a local pelvic reference system, assumed to be both horizontal in the supine position and vertical in the standing position. It was extrapolated to be similar to the global system in which the THA must act. It was initially reported to be independent of sex or age [15, 17], stable between the supine and standing position and after implantation of THA [3, 15]. However, great individual variations in the sagittal inclination of this plane were subsequently described [3, 5]. Pinoit observed it vertical in less than 50% of the cases, with a tilt of 5° in 38% and of 10° in 13% [17]. Moreover, the change in pelvic tilt between the sitting, supine, and standing position was reported to be unpredictable [5, 6, 9].
Elsewhere, a pelvic sagittal rotation was demonstrated to drastically affect the functional orientation of the acetabulum [3, 9]. A forward rotation (or flexion) of the pelvis induces a retroversion of the acetabulum, a backwards rotation (or extension) an anteversion [10, 18, 22]. A pelvic extension also decreases the coverage of the femoral head by the acetabulum [21]. Nevertheless, no one has attempted to precisely determine the individual amount of eventual mal-rotation of the pelvis or to relate the variations of the APP inclination to the sagittal balance of the spine. The purpose of this study was to correlate the APP tilt to pelvic and spinal sagittal parameters, in order to provide an easy and useful method to assess the individual amount and the nature of pelvic sagittal mal-rotation.
Materials and methods
Angular measurements of sagittal pelvic and spinal parameters were performed on 223 plain lateral X-rays of the spine, including the pelvis, the femoral heads and the upper part of the femoral diaphysis. All were performed in the standing position with the arms supported [12]. Forty were obtained several years ago from healthy volunteers (23 women and 17 men) for original orthopaedic studies of the functional balance of the spine and the location of the loads of the upper body weight (the “gravity”) relative to the vertebral structures [11, 12]. At this time, these subjects provided their consent for the use of their radiographic and clinical data. They were the normal group, without disturbance of the sagittal balance. One hundred and eighty-three other X-rays from subjects suffering from low back pain (127 women and 56 men) were also analysed. None of these cases had spinal deformities such as scoliosis or spondylolysis, often associated with pelvic asymmetry. They suffered from common chronic spinal degenerative diseases, none underwent surgical treatment. The data were obtained from anonymous radiographic imaging performed clinical low back pain. The Chairman of our Ethics Committee attested that the data collection from the patients and healthy subjects was in agreement with the recommendation of the Institutional Review board of the institution.
For each subject, the APP inclination was linked to sagittal pelvic and spinal parameters already described in the literature for the evaluation of the sagittal balance of the spine [11, 12].
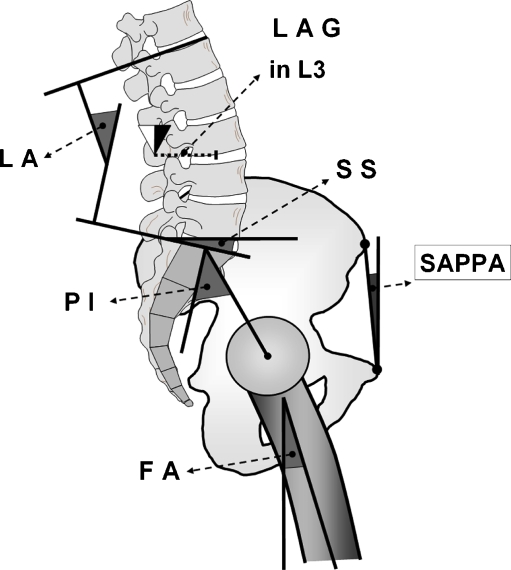
The angular parameters were reported in degrees. In accordance with the definitions of the glossary of the SRS [19], a positive value was posterior, a negative anterior. They were: (Fig. 1)
The sagittal anterior pelvic plane angle (SAPPA): value of the angle between the vertical and the APP. For each case, the distance between the projections of the ASISs was less than 1 cm and the bony landmarks were clearly discernible (i.e. no superimposition of intestinal gas or other causes of local lack of definition).
The “pelvic incidence” (PI): value of the angle between the line perpendicular to the superior plate of the first sacral vertebra (S1) at its midpoint and the line connecting this point to the middle axis of the femoral heads [11, 12].
The “sacral slope” (SS): value of the angle between the superior plate of S1 (or sacral plate) and a horizontal line. A vertical sacrum was described by a low value of SS, a horizontal sacrum by a high value.
The “lordosis angle” (LA): the value of the angle between the sacral plate and the more backward tilted plate of another lumbar or thoracic vertebra (in our series always L1 or T12).
The “kyphotic angle” (KA): the value of the angle between the more backward tilted plate used for “LA” measurement and the more forward tilted upper vertebral plate.
Fig. 1.
The angular sagittal pelvic parameters: the sagittal anterior pelvic plane angle (SAPPA), the pelvic incidence (PI), the sacral slope (SS), the lordosis angle (LA), the lever arm of the gravity in the third lumbar vertebra (LAG), the femoral axis (FA)
These angles have been thoroughly described several years ago in the orthopaedic literature for the analysis of the sagittal balance of the spine [11, 12]. The anatomical parameter “pelvic incidence” was demonstrated to be the “key parameter” [18]. A strict relationship was described between this anatomical parameter PI and the sagittal tilt of the sacral plate (SS), and between this “SS” and the amount of lumbar lordosis (LA) [12].
 |
For each subject, the observed values of SS and LA were compared with the theoretically optimal values required by these two equations for a harmonious sagittal balance. The differences between the observed and theoretical values were reported as:
The “difference in sacral slope” (DSS): difference between the observed and theoretical values of sacral slope.
The “difference in lordosis angle” (DLA): difference between the observed and theoretical values of lordosis angle.
These differences were reported in absolute values in Table 1 to emphasise the existence of sagittal perturbations, but the real values were used afterwards for the analysis of the sagittal imbalances. A backward rotation of the pelvis (i.e. a positive value of the SAPPA) denoted a rotation along an axis joining the two femoral heads such that the pubis became anterior to the ASISs (pelvis extension or retroversion) and a decrease of the value of the SS. Inversely, a pelvic forward rotation (pelvis flexion or anteversion) was expressed by a negative value.
The “femoral axis” (FA) was the value of the angle between the upper part of the femoral diaphysis and the vertical. It expresses a flexion of the hips and the knees as a compensation for a global sagittal imbalance.
The “lever arm of the gravity” (LAG) supported by the vertebral structures in L3 (GL3) was also reported. It was calculated by a specific software (“Similibary©”) using a predictive equation including radiographic and anthropometric parameters [12]. It was expressed in millimeters between the middle of the inferior plate of L3 and the projection at this level of the gravity of the bodily segment supported by this vertebra. The lever arm was expressed negative if anterior, positive if posterior. It was reported normal for a value of 24 ± 15 mm.
The “body mass index” (BMI): measure of the body fat using the weight divided by the square of the height (kg/m2).
Table 1.
Mean values and standard deviation (S.D.) of the parameters and “t Values” of the Student’s tests performed for the comparisons between the “Normal” and “Low back pain” clinical groups. The significant symbols were: * for p<0.05, ** for p< 0.01, *** for p<0.001*.
| Normal | Low back pain | |||||
|---|---|---|---|---|---|---|
| n = 40 | n = 183 | |||||
| Mean | S.D. | Mean | S.D. | t | ||
| Age (years) | 44 | 17 | 61 | 19 | 5.61 | *** |
| Anterior pelvic plane (°) | −1 | 4 (−7, 7) | 1 | 8 (−24, 21) | 2.31 | * |
| Pelvic incidence (°) | 50 | 12 | 49 | 13 | 0.47 | N.S. |
| Sacral slope (°) | −39 | 7 | −33 | 11 | 4.37 | *** |
| Difference in sacral slope (° in absolute values) | 3 | 2 ( 0, 6) | 7 | 5 (0, 19) | 8.22 | *** |
| Lordosis angle (°) | 50 | 9 | 31 | 16 | 10.27 | *** |
| Difference in lordosis angle (° in absolute values) | 6 | 5 | 29 | 12 | 19.36 | *** |
| Kyphosis angle (°) | −44 | 11 | −53 | 11 | 4.63 | *** |
| Femoral axis (°) | 2 | 2 | 7 | 5 | 10.28 | *** |
| Lever arm of the gravity in L3 (mm) | −6 | 22 | 2 | 29 | 1.96 | ** |
| Body mass index (kg/m2) | 24.8 | 4.4 | 28.9 | 14 | 3.29 | *** |
Results
The mean values and standard deviations of the parameters were reported in Table 1. Student tests were performed to compare both populations. The significantly higher mean age of the low back pain population was in accordance with the usual age of the subjects’ candidate for a THA. In any event, the sagittal morphology of the pelvis, expressed by the PI, was reported to be stable with ageing, as observed here similar for both groups. The comparisons between the two populations were so allowed.
The mean values of the pelvic and spinal parameters observed for normal subjects were in concordance with the data in the literature [11, 12]. In the same way, the harmony between PI, SS, and LA was expressed by insignificant values of DSS and DLA. For low back pain cases, the SS was observed to be significantly more horizontal and the lordosis less pronounced than for normal cases.
Moreover, the disturbance of the sagittal balance for 77 of the low back pain cases results in a significant difference between the observed and theoretical values (DSS and DLA), in one or the other direction according to subjects. A significant relative backward rotation of the pelvis was observed in 34 cases (mean value of DSS 12 ± 4°), a relative forward rotation in 43 cases (mean value of DSS −11 ± 4°). In the same way, a relative hyper-lordosis was observed in 20 cases (mean value of DLA 7 ± 5°), a hypo-lordosis in 74 cases (mean value of DLA 9 ± 4°). Pelvises in extension (retroversion) were always combined with a hypo-lordosis. Fixed flexion of the hips (i.e. a noteworthy value of FA) expressed an additional pelvic retroversion because of a lumbar lordosis insufficient to compensate an upper sagittal imbalance.
A significant number of the low back pain population were overweight. Its harmful effect was the result both of an increase of the gravity loads and of muscular insufficiency. A significant forward displacement of the application point of gravity (LAG) was observed for the low back pain population. This resulted in disturbances of the harmony between the positional parameters, including the pelvic tilt, as a compensatory effort to maintain the gravitational loads as posterior as possible.
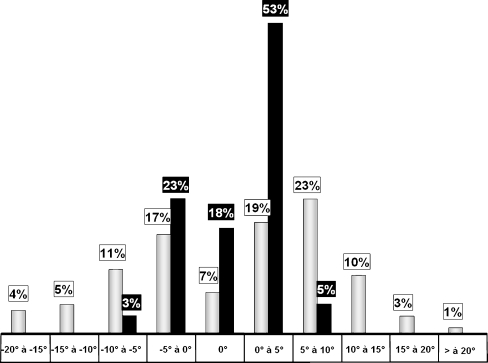
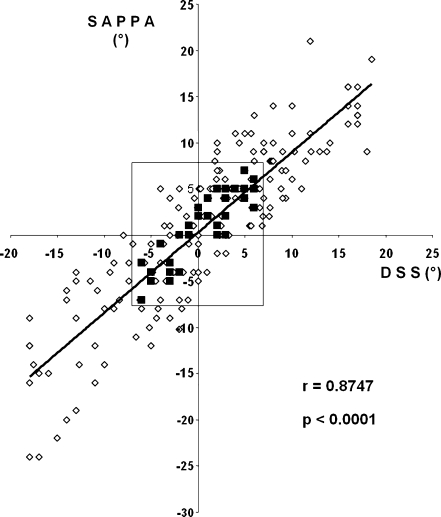
The mean values of the sagittal tilt of the APP were observed to be weakly significantly different (t = 2.31, p < 0.05) between both populations when expressed in real values (i.e. positive and negative). However, when expressed in absolute value, the APP were observed almost vertical for the normal subjects (mean value 3 ± 2°), but significantly (t = 8.947, p < 0.001) more tilted for the low back pain cases (mean value 9 ± 5°). In Fig. 2 the relationship of the sagittal anterior pelvic plane angle for both groups is shown. The SAPPA was less than 5° in 94% of the normal subjects, but in only 43% of the low back pain cases. For the low back pain group, the SAPPA was from 5 to 10° in 21% of the cases and more than 10° in 13%, for some forwards, for other backwards. Moreover, a close relationship (Pearson’s correlation coefficient 0.8747, p < 0.0001) was observed for all the subjects, between the SAPPA and the difference between the observed and theoretical values of sacral slope DSS (Fig. 3). It makes the strict relation between the SAPPA and a disturbance of the sagittal balance of the spine obvious.
Fig. 2.
Relationship of the forward and backward variability of the angle of the sagittal anterior pelvic plane angle (SAPPA) (black columns for the normal subjects, white columns for the low back pain cases)
Fig. 3.
Relationship between the sagittal anterior pelvic plane angle (SAPPA) and the difference between the observed and theoretical values of sacral slope (DSS) (black points were for the normal subjects, white points were for the low back pain cases)
Discussion
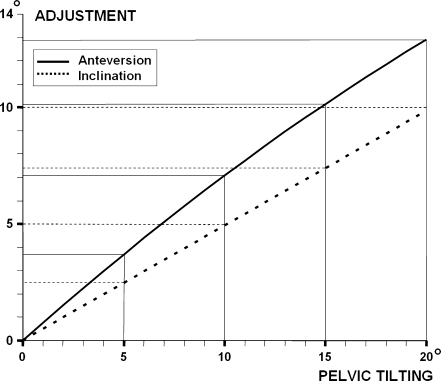
The close relationship between pelvic tilt and cup orientation has been pointed out by several authors. First McCollum proposed a standing lateral roentgenogram for direct measurement of the cup flexion [16]. Lazennec expressed the sagittal inclination of the cup by a morphological angle, the sacro-acetabular angle (between the sagittal axis of the prosthetic cup and the upper sacral plate) which was the geometric sum of the positional angle SS and the sagittal acetabular tilt [9]. Chen, by a mathematical model and on a “Sawbone”, reported a variation of the cup position from 15° anteversion in 0° pelvic inclination to 0.5° retroversion in 15° forwards sagittal pelvic tilting [4].The influence of the spine on the sagittal pelvic tilt and on the cup orientation was pointed out by Tang and Chiu for patients with ankylosing spondylitis [20]. They advised adapting the usual positioning of the cup by reducing the inclination and anteversion by 5° for each 10° of sagittal mal-rotation beyond 20°. But they advised using only the shape of the obturator foramen to assess this sagittal mal-rotation on antero-posterior radiographic imaging [20]. To date, a precise assessment of the exact amount of pelvic mal-rotation was not achievable. However, our study has displayed an easy clinical method using the analysis of the sagittal balance of the spine, clearly described and validated in the spinal literature. The difference between the observed and theoretical values of the SS allows a precise assessment of the pelvic sagittal mal-rotation. The overall analysis of the sagittal balance allows the origin of an imbalance to be established. The pelvic tilt could be either forward, directly induced by fixed flexion of the hips or of the knees, either backward (generally in the elderly) in relation to a low value of LA insufficient to compensate a kyphosis. A graph was provided in Fig. 4 for an immediate evaluation of the necessary correction of the anteversion and inclination angles of the cup in the individual pelvic mal-rotation. If a backward mal-rotation is observed (or likely), the corrective angle has to be subtracted from the target angle. The suggested corrections were in accordance with those reported by Tang et al. [20]. Other authors proposed a correction of 0.5 to 0.7° for 1° of pelvic sagittal rotation [2, 3, 10, 13]. However our analysis was more precise and three-dimensional by including the aimed anteversion and inclination angles (See in “Appendix-2”). For this reason, we recommend a routine pre-operative lateral X-ray view of total vertebral column in upright position to assess the global sagittal balance and its probable future evolution. In the same way, we think that the current use of CAOS should be cautious, because these systems are referenced to the APP to regulate the positioning of the cup making malpositioning more likely. The retrieved data will allow fascinating CAOS system re-development taking into account the functional total balance on a purely individual basis so as to allow an adequate orientation of the cups in conformity with the particular patient. The positioning of the cup in THA must so be not only three-dimensional, but also dynamic and functional.
Fig. 4.
Relation between the pelvic sagittal tilting and the angle of inclination and anteversion of the acetabular cup for an aimed 45° inclination
Conclusion
A detailed analysis of individual sagittal balance allows a precise evaluation of the amount of sagittal pelvic mal-rotation which influences acetabular cup orientation and allows preventive or prospective adjustment of the cup positioning. The usefulness of the APP as reference was corroborated for all eventual corrections applied for an individually adjusted cup orientation, even with CAOS.
Appendix
Anteversion of a circle measured from the elliptical appearance of a circular marker wire is: arc sin of the ratio between the lengths of the minor and major axes [1].
The impact of a sagittal pelvic rotation (γ) on the acetabular orientation is three-dimensional and acts as a sagittal rotation of a local axis system into a global reference system. This influence on the acetabular anteversion is so connected to the amount of lateral inclination (β), as described in 1986 by Ackland et al. [1]: it is total for a “β” angle strictly horizontal; nil if it is vertical.
The consequence of a pelvic rotation “γ” on the anteversion (α) of a cup with an inclination “β” is
 |
All angles expressed in degrees.
References
- 1.Ackland MK, Bourne WB, Uhthoff HK. Anteversion of the acetabular cup. Measurement of angle after total hip replacement. J Bone Joint Surg Br. 1986;68:409–413. doi: 10.1302/0301-620X.68B3.3733807. [DOI] [PubMed] [Google Scholar]
- 2.Anda S, Svennneingen S, Grontvdt T, Benum P. Pelvic inclination and spatial orientation of the acetabulum. A radiographic, computed tomographic and clinical investigation. Acta Radiol. 1990;31(4):389–394. doi: 10.3109/02841859009172013. [DOI] [PubMed] [Google Scholar]
- 3.Babisch JW, Layher F, Amiot LP. The rationale for tilt-adjusted cup navigation. J Bone Joint Surg Am. 2008;90(2):357–365. doi: 10.2106/JBJS.F.00628. [DOI] [PubMed] [Google Scholar]
- 4.Chen E, Goertz W, Lill CA. Implant position calculation for acetabular cup placement considering pelvic lateral tilt and inclination. Comput Aided Surg. 2006;11(6):309–316. doi: 10.1080/10929080601090516. [DOI] [PubMed] [Google Scholar]
- 5.DiGioia AM, Hafez MA, Jaramaz B, Levison TJ, Moody JE. Functional pelvic orientation measured from lateral standing and sitting radiographs. Clin Orthop Relat Res. 2006;453:272–276. doi: 10.1097/01.blo.0000238862.92356.45. [DOI] [PubMed] [Google Scholar]
- 6.Eddine TA, Migaud H, Chantelot C, Cotten A, Fontaine C, Duquennoy A. Variations of pelvic anteversion in the lying and standing positions: analysis of 24 control subjects and implications for CT measurement of position of a prosthetic cup. Surg Radiol Anat. 2001;23(2):105–110. doi: 10.1007/s00276-001-0105-z. [DOI] [PubMed] [Google Scholar]
- 7.Kalteis T, Handel M, Bäthis H, Perlick L, Tingart M, Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty. J Bone Joint Surg Br. 2006;88(2):163–167. doi: 10.1302/0301-620X.88B2.17163. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear and component migration. J Arthroplasty. 1998;13(5):530–534. doi: 10.1016/S0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 9.Lazennec JY, Charlot N, Gorin M, Roger B, Arafati N, Bissery A, Saillant G. Hip-spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat. 2004;26:136–144. doi: 10.1007/s00276-003-0195-x. [DOI] [PubMed] [Google Scholar]
- 10.Leenders T, Vandevelde D, Mahieu G, Nuyts R. Reduction in variability of acetabular abduction using computer-assisted surgery: a prospective and randomized study. Computed Aided Surg. 2002;7:99–106. doi: 10.3109/10929080209146021. [DOI] [PubMed] [Google Scholar]
- 11.Legaye J, Duval-Beaupere G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Legaye J, Duval-Beaupère G (2007) Gravitational forces and sagittal shape of the spine. Clinical estimation of their relations. Int Orthop, Epub jul 25, 2007 [DOI] [PMC free article] [PubMed]
- 13.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76(4):517–523. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 14.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplaties. J Bone Joint Surg Am. 1978;60(2):217–220. [PubMed] [Google Scholar]
- 15.Mayr E, Kessler O, Prassl A, Rachbauer F, Krismer M, Nogler M. The frontal pelvic plane provides a valid reference system for implantation of the acetabular cup: spatial orientation of the pelvis in different positions. Acta Orthop. 2005;76(6):848–853. doi: 10.1080/17453670510045471. [DOI] [PubMed] [Google Scholar]
- 16.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res. 1990;261:159–170. [PubMed] [Google Scholar]
- 17.Pinoit Y, May O, Girard J, Laffargue P, Ala Eddine T, Migaud H. Low accuracy of the anterior pelvic plane to guide the position of the cup with imageless computer assistance: variation of position in 106 patients. Rev Chir Orthop Reparatrice Appar Mot. 2007;93(5):455–460. doi: 10.1016/s0035-1040(07)90327-x. [DOI] [PubMed] [Google Scholar]
- 18.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 19.Stokes IA. Three-dimensional terminology of spinal deformities. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group a 3D terminology of spinal deformity. Spine. 1994;19:236–248. doi: 10.1097/00007632-199401001-00020. [DOI] [PubMed] [Google Scholar]
- 20.Tang WM, Chiu KY, Kwan MF, et al. Sagittal pelvic mal-rotation and positioning of the acetabular component in total hip arthroplasty: three-dimensional computer model analysis. J Orthop Res. 2007;25(6):766–771. doi: 10.1002/jor.20225. [DOI] [PubMed] [Google Scholar]
- 21.Watanabe W, Sato K, Itoi E, Yang K, Watanabe H. Posterior pelic tilt in patients with decreased lumbar lordosis decreases acetabular femoral head covering. Orthopaedics. 2002;25(3):321–324. doi: 10.3928/0147-7447-20020301-16. [DOI] [PubMed] [Google Scholar]
- 22.Zilber S, Lazennec JY, Gorin M, Saillant G. Variations of caudal, central, and cranial acetabular anteversion according to the tilt of the pelvis. Surg Radiol Anat. 2004;26(6):462–465. doi: 10.1007/s00276-004-0254-y. [DOI] [PubMed] [Google Scholar]