Abstract
The aim of the study was to determine whether the incidence of radiolucencies can be reduced using pulsed lavage before cementing the tibia in unicompartmental knee arthroplasty (UKA). We prospectively studied a consecutive series of 112 cemented Oxford UKA in 100 patients in two centres. In group A (n = 56) pulsed lavage and in group B (n = 56) conventional syringe lavage was used to clean the cancellous bone. The same standardised cementing technique was applied in all cases. At a minimum follow-up of one year patients were evaluated clinically and screened radiographs were obtained. The cement bone interface under the tibial plateau was divided into four zones and evaluated for the presence of radiolucent lines. All radiographs were evaluated (n = 112), and radiolucencies in all four zones were found in two cases in group A (4%) and in 12 cases in group B (22%) (p = 0.0149). Cement penetration showed a median of 2.6 mm (group A) and 1.5 mm (group B) (p < 0.0001). We recommend the routine use of pulsed lavage in Oxford UKA to reduce the incidence of radiolucency and to improve long-term fixation.
Résumé
Le but de cette étude est de déterminer les possibilités de réduction de l’incidence des liserés en utilisant un lavage pulsé avant la cimentation du tibia dans les prothèses unicompartimentales du genou (UKA). Nous avons réalisé une étude prospective consécutive de 112 prothèses (UKA) chez 100 patients, interventions réalisées dans deux centres. Dans le groupe A (n = 56): utilisation d’un lavage pulsé et dans le groupe B (n = 56): lavage conventionnel à la seringue de façon à nettoyer l’os spongieux. La même technique standardisée de cimentation a été utilisée dans tous les cas. Après un suivi minimum d’un an, les patients ont été évalués cliniquement et radiographiquement. L’interface os/ciment sous le plateau tibial a été divisé en 4 zones pour mieux analyser la présence des liserés. Toutes les radiographies ont été analysées (n = 112) et les liserés dans les 4 zones ont été trouvés dans deux cas, dans le groupe A (4%) et dans le groupe B (22%) (p = 0,0149). La pénétration médiane du ciment dans le groupe A est de 2,6 mm et dans le groupe B de 1,5 mm (p < 0,0001). Nous recommandons donc, en routine, l’utilisation d’un lavage pulsé de façon à réduire l’incidence des liserés et améliorer la fixation à long terme dans la mise en place des prothèses uni-compartimentales de type Oxford.
Introduction
Radiolucent lines (RL) at the cement bone interface of the tibial plateau are a frequent finding in total knee arthroplasty (TKA). Incidences of up to 94% have been reported [4, 9, 23]. The incidence is related to how the radiographs are taken, with the highest rate being when the X-ray beam is parallel to the bone implant interface [20]. However, standardised screened radiographs aligned with the interface are rarely used for routine follow-up in TKA.
Several studies reported rates of RL of 61–96% at the bone–cement interface following Oxford unicompartmental knee arthroplasty (UKA) using screened radiographs [17, 18, 25, 26]. The clinical relevance of this radiographic finding is still unknown. The presence of RL however does not seem to influence the clinical outcome [20, 25]. For reliable detection of RL the X-ray beam must be parallel to the tibial tray in the AP-view [5], clinically this is best achieved with the use of an image intensifier.
Most radiolucent lines are 1 mm wide and are surrounded by a radiodense sclerotic margin. Usually the so-called physiological RL develop in the first year postoperatively and do not progress in the longer term [20, 25]. RL of more than 2 mm with poorly defined margins are considered as pathological RL. However they can be associated with tibial plateau loosening [25].
The results of the Swedish hip arthroplasty register have emphasised the important role of jet lavage in cemented total hip arthroplasty (THA) and reported a risk reduction of more than 20% for aseptic loosening after revision [2]. In addition, studies in hip and knee arthroplasty have shown that pulsed lavage can improve cement penetration and implant stability [2, 3, 7, 16, 27]. To our knowledge the effect of pulsed lavage has not been studied in UKA. We therefore examined two cohorts of Oxford UKA treated at two centres with the same standardised operative and cementing technique. In one group pulsed lavage was used to clean out the tibial cancellous bone and syringe lavage was used in the other group to examine the effect of pulsed lavage on cement penetration and the potential formation of RL. The hypothesis was that pulsed lavage reduces the incidence of complete RL compared to syringe lavage.
Materials and methods
In two consecutive series Oxford UKA surgery was performed for anteromedial osteoarthritis of the knee. In group A pulsed lavage was applied before cementing the components and in group B manual syringe lavage was used. Both groups consisted of 56 knees. Demographics are shown in Table 1.
Table 1.
Patients’ related factors
| Description | Group A Pulsed lavage | Group B Syringe lavage |
|---|---|---|
| Patients | 54 | 46 |
| Male | 27 (50%) | 24 (52%) |
| Female | 27 (50%) | 22 (48%) |
| Number of knees (left/right) | 56 (28/28) | 56 (26/30) |
| Median age (y) | 63 (range 45–78) | 68 (range 49–80) |
| Median follow-up (mo) | 24 (range 12–48) | 19 (range 12–36) |
In all cases the Oxford UKA was performed using the phase III instruments (Biomet, Swindon, UK) by experienced knee surgeons. Two patients from group A and ten patients from group B had undergone two-stage bilateral UKA. The same cementing technique was used in both groups. After bone lavage the keel slot was filled with bone cement and a thin layer of cement was spread over the tibial surface. Palacos bone cement was used in group A (Biomet, Swindon, UK) and CMW 1 bone cement was used in group B (DePuy, Warsaw, USA). The tibial tray was introduced into the knee and the posterior part of the tray was seated first to avoid posterior cement extrusion. Then the anterior portion was seated and the implant was impacted using a light toffee hammer. For curing of the cement the knee was positioned in 45° of flexion and an appropriate spacer was inserted for gentle compression. Postoperative full weight bearing and free ROM was allowed in all patients.
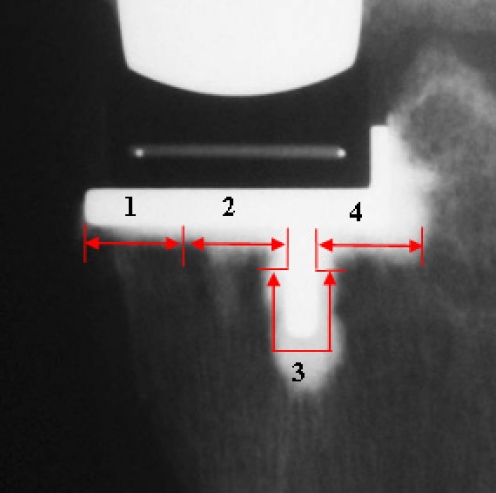
Pre- and postoperatively the Oxford knee score, the Knee Society score and the Knee function score were assessed for each patient in both groups. In addition, screened radiographs were taken and the incidence of radiolucent lines under the tibial component was assessed. Minimum radiographic follow-up was 12 months in both groups. All radiographs were taken in a standardised manner with an image intensifier. The direction of the X-ray beam was adjusted until it was parallel to the articulating surface, keel and lip of the tibial component. High resolution images were obtained and were digitised and magnified by a factor of ten. For the assessment of radiolucency and cement penetration, the bone–cement interface was divided into four zones (Fig. 1). For each zone, the presence and morphology (width, sclerotic margin) of the radiolucent lines were recorded and the minimum cement penetration was measured below the tibial component, defined as the shortest distance between the implant and the cement surface. Corrections were made for magnification based on the known size and thickness of the tibial components, which were used as a reference. For both groups, one independent experienced orthopaedic surgeon performed the measurement of radiolucencies and cement penetration digitally under blind conditions. The intrarater interclass correlation coefficient for the radiological examination was calculated (r = 0.94).
Fig. 1.
Standardised analysis of tibial bone–cement interface in four zones
Pulsed lavage is likely to have a greater effect in cancellous bone than cortical bone [2]. Our analysis therefore focussed on zones 2, 3 and 4, which are predominantly cancellous, rather than zone 1, which is predominantly cortical. For statistical evaluation the Chi-square test and exact Mann-Whitney U-test were used. A p-value <0.05 was deemed to be statistically significant, although there was multiple testing. The analysis was done using the statistical software SAS, version 9.13 for Windows (SAS Institute, Cary, NC).
Results
For clinical assessment, the preoperative and postoperative mean functional scores of both groups are shown in Table 2. The differences were not statistically significant.
Table 2.
Clinical scores pre- and postoperatively
| Scores | Group A | Group B | ||
|---|---|---|---|---|
| Preop | Postop | Preop | Postop | |
| Oxford knee score (SD) | 19.6 (6.8) | 41.9 (13.3) | 18.0 (6.2) | 39.9 (10.2) |
| Knee Society score (SD) | 45.5 (15.9) | 90.0 (19.4) | 35.4 (12.5) | 91.2 (14.1) |
| Knee function score (SD) | 55.0 (19.9) | 90.0 (23.6) | 49.9 (10.3) | 82.5 (20.8) |
For the radiographic assessment, radiolucent lines were seen in both groups, but no pathological RL were detected. Differences were found in different zones for both groups. The results for the presence of RL are shown in Table 3. The difference between the two groups was statistically significant (Chi-square test p = 0.0149).
Table 3.
Appearance of radiolucent lines (RL) independent from location
| Group | No RL | Partial RL | Complete RL |
|---|---|---|---|
| Group A (pulsed lavage) | 26 (46%) | 28 (50%) | 2 (4%) |
| Group B (syringe lavage) | 20 (36%) | 24 (43%) | 12 (21%) |
In zones 2, 3 and 4 (Table 4), representing the area of trabecular bone, group A showed a significantly lower incidence of radiolucent lines (p = 0.0065).
Table 4.
Radiolucent lines (RL) in zones 2, 3 and 4 (appearance independent from location)
| Group | No RL | RL in one zone | RL in two zones | RL in all zones |
|---|---|---|---|---|
| Group A (pulsed lavage) | 37 (66%) | 13 (23%) | 4 (7%) | 2 (4%) |
| Group B (syringe lavage) | 22 (39%) | 13 (23%) | 9 (16%) | 12 (22%) |
Table 5 shows the distribution of radiolucent lines depending on location of the four zones. The minimum cement penetration in different zones is shown in Table 6. Group A had a significantly deeper cement penetration in all zones compared to group B.
Table 5.
Incidence of radiolucent lines
| Group | Zone 1 | Zone 2 | Zone 3 | Zone 4 |
|---|---|---|---|---|
| Group A (Pulsed lavage) | 29 (52%) | 17 (30%) | 4 (7%) | 6 (11%) |
| Group B (syringe lavage) | 26 (46%) | 23 (41%) | 19 (34%) | 24 (43%) |
| p value | 0.5707 | 0.2086 | 0.0005 | <0.0001 |
Table 6.
Mean values of minimum cement penetration
| Group | Zone 1 (mm) | Zone 2 (mm) | Zone 3 (mm) | Zone 4 (mm) |
|---|---|---|---|---|
| Group A (SD) | 1.3 (0.9) | 2.4 (1.0) | 1.4 (0.5) | 4.0 (1.2) |
| Group B (SD) | 0.8 (0.6) | 1.6 (0.8) | 0.7 (0.4) | 2.4 (0.9) |
| p value | 0.001 | <0.0001 | <0.0001 | <0.0001 |
Discussion
This study confirms that radiolucencies are common under the tibial tray of Oxford unicompartmental knee arthroplasty [20, 25]. The overall incidence of radiolucencies in our study was 58%. This incidence is high as the radiographs were obtained using image intensifiers that were aligned parallel to the implant bone interface. With standard radiographs the incidence is lower as the X-ray beams are not parallel to the interface and the RL are often obscured by the metal component [25].
Our data clearly showed that RL can occur irrespective of the lavage technique used; however, the incidence of radiolucency can be reduced significantly by using pulsed lavage as postulated. This is probably due to the deeper penetration of bone cement into the lavaged cancellous bone.
The clinical significance and the aetiology of the RL are poorly understood [20]. Radiolucencies in cemented total hip arthroplasty are usually associated with implant motion and loosening of the components [22]. They are observed more frequently beneath the socket [6, 19]. When diagnosed they tend to progress leading to revision over time [19].
In cemented unicompartmental arthroplasty two different types of tibial RL have been described [8]. “Physiological RL”, which are usually 1 mm thick with a sclerotic margin, are a frequent finding. They commonly develop during the first year. Thereafter, although they consolidate, they do not progress. However, “pathological” tibial radiolucencies, which are more than 2 mm thick without a sclerotic margin and progressive, are usually indicative of infection or loosening. The differentiation between “physiological RL” can be difficult, such that unnecessary revision may be the consequence of their presence [8].
The histological appearance of the RL is fibrocartilaginous tissue and the radiodense margin is due to a lamella of subchondral bone [25]. Their presence is not related to pain or a poor clinical outcome [25].
The nature of the junctional tissues between implant and bone depends substantially on mechanical factors [14]. There can be osseointegration, a fibrous or fibrocartilaginous interface, or early loosening. The nature of the interface depends on the balance between the strength of the initial mechanical interlock between cement and bone, and the magnitude of the applied loads. The surgeon is responsible for the strength of the initial interlock, whereas loads are applied by the patient after the operation. High interface strength is associated with osseointegration, low interface strength plus high loads will give rise to a soft tissue layer between implant and bone [13]. Iwaki et al. [11] have shown that with good initial fixation, minimal migration of the implant and no radiolucent lines are likely to develop in total hip replacement (THR) and that the long-term outcome is determined at the time of the initial operation. With knee arthroplasties the situation is different. Although all loose knee implants are associated with radiolucency, not all implants with radiolucencies are loose [20]. In cases of “physiological” radiolucency, with the Oxford UKA compressive loads are transmitted through a thin layer of fibrous tissue and mechanics and biology are balanced. However, a strong interface with osseointegration of the tibial component is probably more desirable.
The Swedish hip arthroplasty register demonstrates that a third generation cementing technique improves the long-term outcome of THR. The aim of modern cementing techniques is to improve the mechanical interlock between bone and cement. This is achieved by pressurisation and the use of the pulsed lavage for cleaning the cancellous bone from fat and bone marrow. Numerous studies have shown that the strength of the bone-cement interface is dependant on cement penetration and interdigitation [1, 10, 12, 15]. Our data on UKA tibial component fixation also support this. In our series the pulsed lavage group had significantly higher cement penetration than the syringe lavage group. As a result of the deeper penetration rate the incidence of RLs was significantly reduced. Cement penetration and decrease in RL was best achieved in zones 3 and 4, where mainly cancellous bone is found and pulsed lavage is most effective. In the cortical bone of zone 1 pulsed lavage was less effective.
Our study does have limitations. The study was not randomised, but rather was a comparison between two different centres with different operating surgeons. Factors other than the type of lavage used may have influenced the outcome. Although most demographic factors (Table 1) were similar in both groups the pulsed lavage group tended to be younger and had longer follow-up. Young patients tend to have more dense bone in which it may be more difficult to obtain cement penetration so the positive effect of pulsed lavage might be underestimated in our study. Although radiolucencies tend to appear during the first year, they can also develop during the second [8]. Therefore, their incidence might have been even lower in the pulsed lavage group if the follow-up had been the same as in the syringe lavage group.
Cement penetration into cancellous bone is dependant on many factors other than the type of bone lavage. The amount of fluid used for cleansing the bone bed was not measured or standardised in both groups. Moreover, the two centres used different bone cements (group A used Palacos R; group B used CMW 1). The difference in cement viscosity may have affected the result. There is however no consensus about the relationship between cement viscosity and penetration; Breusch demonstrated in an animal model that penetration is significantly higher with high viscosity bone cements whereas some clinical studies did not show any difference between low and high viscosity bone cements, and others found higher penetration rates with the use of low viscosity cements [21, 24]. Cement penetration is also influenced by pressurisation and bleeding. As both centres routinely used a tourniquet during the operation, bleeding during cementation is unlikely to have influenced the conclusion of the study. Pressurisation of cement, which is a mandatory part of modern hip cementing techniques, is not used in UKA for anatomical reasons. Pressure is usually applied in two stages during the cementation process: first, when implanting and impacting the tibial component and second, due to the tension of the ligaments when the spacer is inserted in 45° of knee flexion. Both centres pressurised in the same manner.
To our knowledge there is no other clinical study evaluating the influence of pulsed lavage on the incidence of radiolucent lines in unicompartmental knee arthroplasty. A prospective randomised clinical study with one surgeon using one bone cement could exclude the bias of a possible difference in the frequency of RL in different bone cements. However, it seems that pulsed lavage decreases the incidence of RL and increases cement penetration. Therefore, we think that the evidence produced in our study is strong enough to recommend that pulsed lavage should be used before cementing in Oxford UKA. As a result of our study the surgeons of hospital B have changed their clinical practice and now routinely use the pulsed lavage.
In conclusion, we recommend a thorough pulsed lavage of the cancellous bone surface of the tibial plateau as a standard procedure to improve cement penetration and to decrease the incidence of radiolucent lines.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Askew MJ, Steege JW, Lewis JL, et al. Effect of cement pressure and bone strength on polymethylmethacrylate fixation. J Orthop Res. 1984;1:412–420. doi: 10.1002/jor.1100010410. [DOI] [PubMed] [Google Scholar]
- 2.Breusch SJ, Norman TL, Schneider U, et al. Lavage technique in total hip arthroplasty: jet lavage produces better cement penetration than syringe lavage in the proximal femur. J Arthroplasty. 2000;15:921–927. doi: 10.1054/arth.2000.8098. [DOI] [PubMed] [Google Scholar]
- 3.Breusch SJ, Schneider U, Reitzel T, et al. Significance of jet lavage for in vitro and in vivo cement penetration. Z Orthop Ihre Grenzgeb. 2001;139:52–63. doi: 10.1055/s-2001-11871. [DOI] [PubMed] [Google Scholar]
- 4.Duus BR, Boeckstyns M, Kjaer L, et al. Radionuclide scanning after total knee replacement: correlation with pain and radiolucent lines. A prospective study. Invest Radiol. 1987;22:891–894. doi: 10.1097/00004424-198711000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Ecker ML, Lotke PA, Windsor RE, et al. Long-term results after total condylar knee arthroplasty. Significance of radiolucent lines. Clin Orthop Relat Res. 1987;216:151–158. [PubMed] [Google Scholar]
- 6.Garcia-Cimbrelo E, Diez-Vazquez V, Madero R, et al. Progression of radiolucent lines adjacent to the acetabular component and factors influencing migration after Charnley low-friction total hip arthroplasty. J Bone Joint Surg Am. 1997;79:1373–1380. doi: 10.2106/00004623-199709000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Gisep A, Curtis R, Flutsch S, et al. Augmentation of osteoporotic bone: effect of pulsed jet-lavage on injection forces, cement distribution, and push-out strength of implants. J Biomed Mater Res B Appl Biomater. 2006;78:83–88. doi: 10.1002/jbm.b.30472. [DOI] [PubMed] [Google Scholar]
- 8.Goodfellow JW, O’Connor JJ, Dodd CAF et al (2006) Unicompartmental arthroplasty with the Oxford knee. Oxford University Press, UK
- 9.Guha AR, Debnath UK, Graham NM. Radiolucent lines below the tibial component of a total knee replacement (TKR)—a comparison between single-and two-stage cementation techniques. Int Orthop. 2008;32:453–457. doi: 10.1007/s00264-007-0345-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Halawa M, Lee AJ, Ling RS, et al. The shear strength of trabecular bone from the femur, and some factors affecting the shear strength of the cement-bone interface. Arch Orthop Trauma Surg. 1978;92:19–30. doi: 10.1007/BF00381636. [DOI] [PubMed] [Google Scholar]
- 11.Iwaki H, Scott G, Freeman MA. The natural history and significance of radiolucent lines at a cemented femoral interface. J Bone Joint Surg Br. 2002;84:550–555. doi: 10.1302/0301-620X.84B4.11931. [DOI] [PubMed] [Google Scholar]
- 12.Krause WR, Krug W, Miller J. Strength of the cement-bone interface. Clin Orthop Relat Res. 1982;163:290–299. [PubMed] [Google Scholar]
- 13.Lee C (2005) The importance of establishing the best bone-cement interface. In: Breusch S, Malchau H (ed) The well-cemented total hip arthroplasty—theory and practice. Springer Verlag, Heidelberg
- 14.Ling RS. Observations on the fixation of implants to the bony skeleton. Clin Orthop Relat Res. 1986;210:80–96. [PubMed] [Google Scholar]
- 15.MacDonald W, Swarts E, Beaver R. Penetration and shear strength of cement-bone interfaces in vivo. Clin Orthop Relat Res. 1993;286:283–288. [PubMed] [Google Scholar]
- 16.Mann KA, Ayers DC, Werner FW, et al. Tensile strength of the cement-bone interface depends on the amount of bone interdigitated with PMMA cement. J Biomech. 1997;30:339–346. doi: 10.1016/S0021-9290(96)00164-9. [DOI] [PubMed] [Google Scholar]
- 17.Pandit H, Jenkins C, Barker K, et al. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br. 2006;88:54–60. doi: 10.1302/0301-620X.88B1.17114. [DOI] [PubMed] [Google Scholar]
- 18.Price AJ, Waite JC, Svard U. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2005;435:171–180. doi: 10.1097/00003086-200506000-00024. [DOI] [PubMed] [Google Scholar]
- 19.Ranawat CS, Peters LE, Umlas ME. Fixation of the acetabular component. The case for cement. Clin Orthop Relat Res. 1997;344:207–215. doi: 10.1097/00003086-199711000-00021. [DOI] [PubMed] [Google Scholar]
- 20.Rea P, Short A, Pandit H, et al. Radiolucency and migration after Oxford unicompartmental knee arthroplasty. Orthopedics. 2007;30:24–27. [PubMed] [Google Scholar]
- 21.Reading AD, McCaskie AW, Barnes MR, et al. A comparison of 2 modern femoral cementing techniques: analysis by cement-bone interface pressure measurements, computerized image analysis, and static mechanical testing. J Arthroplasty. 2000;15:479–487. doi: 10.1054/arth.2000.5266. [DOI] [PubMed] [Google Scholar]
- 22.Ritter MA, Zhou H, Keating CM, et al. Radiological factors influencing femoral and acetabular failure in cemented Charnley total hip arthroplasties. J Bone Joint Surg Br. 1999;81:982–986. doi: 10.1302/0301-620X.81B6.9634. [DOI] [PubMed] [Google Scholar]
- 23.Smith S, Naima VS, Freeman MA. The natural history of tibial radiolucent lines in a proximally cemented stemmed total knee arthroplasty. J Arthroplasty. 1999;14:3–8. doi: 10.1016/S0883-5403(99)99999-0. [DOI] [PubMed] [Google Scholar]
- 24.Stone JJ, Rand JA, Chiu EK, et al. Cement viscosity affects the bone-cement interface in total hip arthroplasty. J Orthop Res. 1996;14:834–837. doi: 10.1002/jor.1100140523. [DOI] [PubMed] [Google Scholar]
- 25.Tibrewal SB, Grant KA, Goodfellow JW. The radiolucent line beneath the tibial components of the Oxford meniscal knee. J Bone Joint Surg Br. 1984;66:523–528. doi: 10.1302/0301-620X.66B4.6746686. [DOI] [PubMed] [Google Scholar]
- 26.Weale AE, Murray DW, Crawford R, et al. Does arthritis progress in the retained compartments after ‘Oxford’ medial unicompartmental arthroplasty? A clinical and radiological study with a minimum ten-year follow-up. J Bone Joint Surg Br. 1999;81:783–789. doi: 10.1302/0301-620X.81B5.9197. [DOI] [PubMed] [Google Scholar]
- 27.Wirtz D, Sellei RM, Portheine F, et al. Effect of femoral intramedullary irrigation on periprosthetic cement distribution: jet lavage versus syringe lavage. Z Orthop Ihre Grenzgeb. 2001;139:410–414. doi: 10.1055/s-2001-17983. [DOI] [PubMed] [Google Scholar]