Abstract
This article studies the incidence and magnitude of delayed callus subsidence, which will also help in study the hypothesis of three cortex corticalisation to determine the time of fixator removal during distraction osteogenesis (DO). Eighty-one tibia segments with mean lengthening of 7.7 ± 2.9 cm were studied with age, gender, skeletal maturity, amount and percentage of lengthening, callus pattern, callus shape, number of cortices seen at the time of fixator removal, bone mineral density (BMD) ratio, and callus diameter ratio analysed for their effect on callus subsidence. All segments had tibia callus subsidence ranging from 4 mm to 3.2 cm with 54% having significant subsidence of more than 1 cm. Multivariate regression analysis revealed only the amount of lengthening and callus patterns to be significant. In conclusion, we can say that tibia callus subsidence is a significant delayed complication and factors affecting it can be used to determine the time of fixator removal.
Résumé
Le but de ce travail est d’évaluer l’importance du régénérat et de vérifier l’hypothèse selon laquelle il est nécessaire d’avoir une corticalisation des 3 corticales avant d’enlever le fixateur lors d’allongements de membres. 81 tibias ont été allongés en moyenne de 7.7 à 2.9 cm et analysés en fonction de l’âge, du sexe, de la maturité squelettique et du pourcentage d’allongement, de même en ce qui concerne l’évaluation du cal et le nombre de corticales consolidées au moment de l’ablation du fixateur. Nous avons également réalisé une étude densitométrique (BMD). Tous les régérats osseux, au niveau du tibia, avaient un écart au niveau du cal osseux de 4 mm à 3,2 cm, 54% ayant un écart de plus d’1 cm. L’analyse statistique a montré que les facteurs significatifs étaient surtout dûs à l’importance de l’allongement. En conclusion, dans l’allongement du tibia,nous pouvons affirmer que l’aspect du régénérat est un facteur important qui doit être pris en compte pour déterminer le moment de l’ablation du fixateur.
Introduction
The concept of distraction osteogenesis (DO) was established by Codivilla [8] and detailed by Ilizarov [15–17]. A significant number of complications are associated with DO [12, 23]. Among the delayed complications, refractures and axial deviation have been studied extensively [11, 22, 23]. Delayed loss of length or callus subsidence has anecdotal references in literature [1, 11, 23]. Residual limb length inequality can occur in patients with limb length discrepancy (LLD) undergoing unilateral procedure and in patients with short stature undergoing bilateral procedure. In addition, in bilateral limb lengthening DO can lead to loss of gained length. Few reports point at the factors responsible for callus subsidence. Dynamic weight bearing [22], incomplete bone healing at the time of frame removal [23], age of the patient [5, 11, 23], aetiology [22, 23], amount of lengthening [3, 9, 18, 20], and callus diameter [21] have been reported to affect the quality of the regenerate which in turn affect the callus subsidence. Also, radiographic appearance of callus [10, 19] and bone mineral density [4, 14] help to assess the quality of the regenerate.
This study focuses on detailed examination of incidence and amount of callus subsidence in tibia lengthening by distraction osteogenesis using the Ilizarov apparatus.
Material and methods
A retrospective analysis was performed involving 81 tibia segments in 48 patients that underwent tibia lengthening using the Ilizarov ring apparatus. Thirty-three patients had bilateral lengthening, and 15 patients had unilateral lengthening. Average age at surgery was a mean of 15.1 years (range 6–46 years). There were 40 females and 41 males included in the study with 23 segments in skeletally mature and 58 segments in skeletally immature patients.
Operative and follow-up details
Monofocal metaphyseal corticotomy at the proximal tibia was done in all cases with application of the modified Ilizarov ring apparatus using fully threaded Schanz pins to increase the stiffness of the apparatus. Corticotomy was performed after longitudinally incising the periosteum. Drill holes were made and then connected with a small osteotome. Completion of the osteotomy was confirmed under an image intensifier and then the periosteum was re-sutured.
Distraction was started seven days post surgery at a rate of 0.25 mm four times a day, and biweekly radiographs were taken during the distraction period with monthly radiographs thereafter. All patients were mobilised with partial weight bearing with axillary crutches during the distraction and maturation periods. The fixator was removed when at least three callus cortices were seen on plain radiographs and patients were mobilised first with a long knee cast with axillary crutches and then with a short leg brace and gradual increase in weight bearing until they could walk fully weight bearing with no discomfort.
Evaluation technique
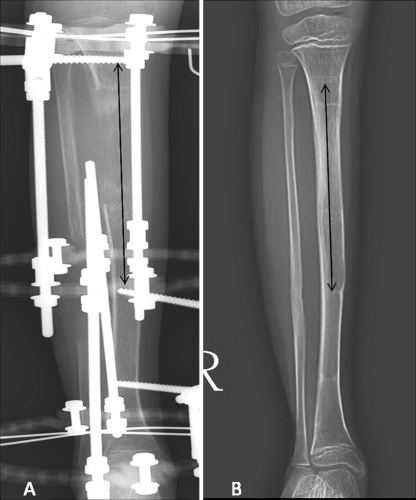
All the radiographs were taken digitally (StarPACS, Infinitt, Pi View Star 5.0 6.0). The maximum amount of distraction was measured from the radiograph at the end of distraction period. We devised an indirect radiological technique to measure the final length of the callus and tibia subsidence. The distance between the Schanz pins closest to the corticotomy site was measured at the end of distraction period. In follow-up radiographs the total length between the bony scars of the Schanz pins was measured and the difference in length from initial measurement was taken as callus subsidence (Fig. 1).
Fig. 1.
Method of measurement of callus subsidence by measuring from the Schanz pins closest to the osteotomy sites (a) and later measuring between the bone scars of the same Schanz pins on follow-up radiographs (b)
Study design
Clinical factors and radiological factors were used. We used BMD ratio and callus diameter ratio to determine the strength of the callus. All patients were classified into various groups for analysis:
Aetiology. All segments were placed into four groups according to aetiology: the dysplasia group (48 segments), LLD group (15 segments), idiopathic short stature (ISS) group (six segments), and hormonal group (ten segments).
Age. Patients were classified into three groups: age less than ten years, ten to 20 years, and more than 20 years.
Gender.
Skeletal maturity.
Amount of tibia distraction. Patients were classified into three groups: <5 cm, 5–10 cm, and >10 cm. For the three lengthening groups the distraction period (from day of starting distraction until the end of distraction), the maturation period (from the end of distraction until the time of adequate three cortices corticalisation and removal of fixator), and the total fixator period (from the day of fixator application until fixator removal) were calculated.
Percentage of tibia distraction. Patients were classified into three groups: <25%, 25–50%, and >50%
Bone mineral density. The BMD calculated by DEXA scan was available only for 36 patients in the series. A BMD ratio was calculated by taking the ratio of BMD of the callus and BMD of the normal bone.
Callus diameter ratio (CDR). CDR was calculated by measuring an average of the anteroposterior and lateral diameters of the callus and dividing it by an average of the diameters of the proximal and distal corticotomy ends.
Callus pattern. We used the method by Li et al. [19] that classified different callus patterns based on the radiographic appearance of callus pattern, density, and shape.
To study the hypothesis that presence of three cortices at the time of fixator removal prevents tibia subsidence we divided the patients into two groups. At the time of fixator removal all segments had at least three cortices regenerated. We further classified on the basis of the fourth cortex: type 1 when the fourth cortex was deficient and type 2 when the fourth cortex was also well consolidated. Since amount of lengthening is now considered a very important prognostic factor during distraction osteogenesis, we combined these factors to further study the hypothesis. Each group of amount of lengthening and percentage of lengthening was further divided into two groups on the basis of presence and deficiency of fourth cortex, and mean subsidence value was compared between these groups.
Statistical method
A univariate analysis was performed for all patient groups, with binary groups analysed using unpaired t tests and the ANOVA test in the remainder of the groups. A p value of 0.05 was taken as significant. A multivariate regression analysis was also performed to check the significance of all these factors. Since BMD values were available for only 36 patients, the BMD ratio was not included in multivariate analysis. Also, since there existed a very close correlation between the amounts of lengthening and lengthening percentage, we excluded the lengthening percentage from the multivariate analysis to decrease the confounding effect. Again, p values less than 0.05 were taken as significant in the multivariate regression analysis.
Results
For the entire group the mean amount of total tibia lengthening was 7.7 ± 2.9 cm (range 2.2–13.4 cm) and mean percentage lengthening was 36.25 ± 20% (range 6–86%) of the original tibia length. In the group with less than 5 cm distraction the mean distraction period was 2.1 months, mean maturation period was 3.8 months, and the mean fixator period was 5.05 months. For the group with distraction between 5 and 10 cm, the mean distraction period was 3.6 months, the mean maturation period was 5.7 months, and the mean fixator period was 10.1 months. For the group with more than 10 cm lengthening the mean distraction period was 4.4 cm, the mean maturation period was 6.2 cm, and the mean fixator period was 11.1 months.
The average follow-up was 35 months (range 25–80 months); however, measurement of the tibia subsidence was possible up to 12–16 months after fixator removal. Subsidence of tibia callus was noted in all tibia segments with mean subsidence being 1.19 ± 0.78 cm (range 0.4–3.2 cm). More than 1 cm loss of callus length was considered to be significant. There were 44 segments (54.4%) with subsidence of more than 1 cm and 37 segments (45.6%) with subsidence of less than 1 cm. From 33 patients undergoing bilateral lengthening, 23 had one limb with subsidence more than 1 cm and the other limb with subsidence less than 1 cm. Five patients of LLD had subsidence more than 1 cm.
The fixator was removed when ‘adequate’ corticalisation was seen and adequate corticalisation was defined as 2 mm of cortex seen with density similar to the normal bone and three such cortices visible on radiograph. None of our patients had nonunion, delayed union, or fracture after fixator removal.
In the univariate analysis (Tables 1 and 2) among the three age groups, the mean subsidence was less in the age group of more than 20 years, yet this was not statistically significant. Results of the ANOVA test indicate that the dysplasia group had maximum mean subsidence while the ISS group had minimum subsidence. The subsidence increased significantly along with amount of tibia distraction and percentage of tibia distraction. The tibia subsidence was found to be significantly more in callus having a lateral shape as compared to other shapes. The fusiform and concave calluses have lowest mean subsidence. There were five types of callus patterns noted on radiographs at the time of fixator removal: types 6, 7, 8, 9, and 10. The tibia subsidence was lowest for type 6 and highest for type 8; however, this was not statistically significant. The tibia subsidence was significantly more when the BMD was less than 85% of normal bone. The subsidence was not statistically significant between the two genders and CDR groups.
Table 1.
Univariate analysis of various factors affecting tibia callus subsidence
| Variables | No. of segments | Subsidence mean ± SD | p value |
|---|---|---|---|
| Gender | |||
| Male | 40 | 1.18 ± 0.83 | 0.23 |
| Female | 41 | 1.2 ± 0.74 | |
| Skeletal maturity | |||
| Immature | 58 | 1.25 ± 0.79 | 0.21 |
| mature | 23 | 1.01 ± 0.73 | |
| Cortical callus types | |||
| Type 1 | 45 | 1.22 ± 0.82 | 0.62 |
| Type 2 | 36 | 1.14 ± 0.73 | |
| Callus diameter ratio | |||
| ≥1 | 29 | 1.12 ± 0.72 | 0.55 |
| <1 | 52 | 1.22 ± 0.81 | |
| BMD ratio | |||
| ≥0.85 | 16 | 0.81 ± 0.4 | 0.01 |
| <0.85 | 20 | 1.26 ± 0.65 | |
All p vales are for the unpaired t test
Table 2.
Comparison among various factors affecting tibia callus subsidence
| Variables | No. of segments | Subsidence | p value | |
|---|---|---|---|---|
| Mean | SD | |||
| Age | ||||
| <10 years | 29 | 1.266 | 0.827 | 0.23 |
| 10–20 years | 35 | 1.269 | 0.810 | |
| >20 years | 17 | 0.900 | 0.606 | |
| Aetiology | ||||
| ISS | 6 | 0.850 | 0.281 | |
| LLD | 15 | 0.947 | 0.549 | 0.003 |
| Dysplasia | 50 | 1.424 | 0.847 | |
| Hormonal | 10 | 0.590 | 0.407 | |
| Tibia distraction | ||||
| <5 cm | 17 | 0.735 | 0.389 | |
| 5–10 cm | 41 | 1.010 | 0.584 | <0.0001 |
| >10 cm | 23 | 1.848 | 0.911 | |
| Percentage distraction | ||||
| <25% | 26 | 0.719 | 0.409 | |
| 25–50% | 37 | 1.330 | 0.805 | <0.0003 |
| >50% | 18 | 1.583 | 0.853 | |
| Callus pattern | ||||
| Type 6 | 18 | 0.989 | 0.801 | |
| Type 7 | 18 | 1.078 | 0.686 | |
| Type 8 | 9 | 1.600 | 0.958 | 0.24 |
| Type 9 | 22 | 1.127 | 0.665 | |
| Type 10 | 14 | 1.429 | 0.890 | |
| Callus shape | ||||
| Cylindrical | 60 | 1.277 | 0.823 | |
| Concave | 7 | 0.633 | 0.266 | 0.047 |
| Fusiform | 6 | 0.633 | 0.250 | |
| lateral | 8 | 1.371 | 0.678 | |
All p values are for the ANOVA test
The groups classified on the basis of presence or deficiency of fourth cortex did not show any statistical difference among the mean tibia subsidence. When these groups were analysed according to amount of lengthening, the mean subsidence was significantly high in the type1 callus group as compared to the type 2 group when amount of lengthening was more than 10 cm. Also, when the percentage of lengthening was more than 50%, the mean tibia subsidence was significantly more in the type 1 group as compared to the type 2 group (Table 3).
Table 3.
Analysis of tibia callus subsidence by taking into account calluses of type 1 and type 2, amount of lengthening, and percentage of lengthening
| Amount of lengthening | |||
|---|---|---|---|
| <5 cm | 5–10 cm | >10 cm | |
| Type 1 callus | 0.97 ± 0.68 | 0.96 ± 0.5 | 2.2 ± 0.86 |
| Type 2 callus | 0.55 ± 0.25 | 1.04 ± 0.63 | 1.3 ± 0.87 |
| p value | 0.26 | 0.67 | 0.025 |
| Percentage of lengthening | |||
| <25% | 25–50% | >50% | |
| Type 1 callus | 0.71 ± 0.40 | 1.4 ± 0.77 | 2.1 ± 0.84 |
| Type 2 callus | 0.74 ± 0.41 | 1.2 ± 0.85 | 1.1 ± 0.65 |
| p value | 0.89 | 0.5 | 0.02 |
The values in the tables are mean subsidence ± standard deviation. Type 1 callus is segment with only three cortices seen at the time of fixator removal. Type 2 callus is segment with all four cortices seen at the time of fixator removal. All p values are for unpaired t test
The results of the multivariate regression analysis indicate that only two factors have significant influence on the tibia callus subsidence, namely, amount of tibia distraction and callus pattern. The multivariate analysis indicates that subsidence increases proportional to the amount of lengthening. Among the callus patterns the minimum subsidence was seen with type 9 callus followed by type10 callus with types 7 and 8 having maximum subsidence.
Discussion
Adequate corticalisation is defined as 2 mm of cortex seen with density similar to the normal bone and three such cortices visible on radiograph [11]. This theory is proposed to help the surgeon to decide the time of fixator removal in order to decrease the incidence of delayed complications. Callus refractures, delayed tibia angulation, and tibia subsidence depend on the strength of the callus to withstand the unprotected weight bearing. Thus, the three delayed complications of DO seem to be part of a continuous spectrum. When the callus strength is good there is minimal callus subsidence. When callus is weak differentially, i.e. one side of the callus is weaker than the other side, the bone tends to angulate on that side [2]. Lastly, a poor regenerate or cases having delayed or nonunion with unexpected excessive weight bearing will cause the callus to fracture [12]. We had no cases of fracture in our study.
Healing in patients less than 20 years of age and skeletally immature patients has been reported to be better [11, 23]. However, this effect was restricted to callus formation and no difference in delayed callus subsidence is seen in our study. Noonan et al. [22] reported that tibia lengthening in patients with ISS and LLD is associated with more problems than lengthening in patients with bone dysplasia, but Barreto et al. [6] reported no significant difference between the complications of leg lengthening using the Ilizarov technique in patients with leg length discrepancy and those with short stature. In our study, the dysplasia group had maximum tibia subsidence, LLD and ISS patients had subsidence in midrange, while patients with hormonal disorder had lowest subsidence. These results indicate that the process of callus subsidence and process of callus formation–consolidation during DO in these aetiologies follow different principles. Amount of lengthening has been a significant indicator of the outcome of leg lengthening procedures [3, 9, 18, 20], and in our study the tibia subsidence was also significantly affected by the amount of lengthening, both in univariate and multivariate analysis results, with greater amount of tibia lengthening leading to greater tibia subsidence. Thus, caution should be exercised during fixator removal, and regular follow-ups should be advised in cases with greater lengthening to detect any callus subsidence. In cases of callus subsidence, patients can be advised to observe a period of non-weight bearing or protected weight bearing until the callus is fully consolidated. BMD of the regenerate has good correlation with callus strength [14]. In our study we found that amount of subsidence was significantly lower in patients with BMD ratio more than 0.85 (mean ±SD, 0.81 ± 0.4 cm) when compared with patients with BMD ratio less than 0.85 (mean ±SD, 1.26 ± 0.65 cm). Thus we can conclude that a BMD ratio of 0.85 can be taken as a criterion to decide the time of fixator removal with respect to preventing delayed callus subsidence. Study of callus pattern and its correlation with clinical outcome was first performed by Catagni [7], later by Hamanishi et al. [13], and recently by Ru Li et al. [19]. In our study we used callus patterns seen at the time of fixator removal with only five out of ten patterns noted at the time of fixator removal. Our results indicate type 9 to have the least subsidence while type 8 had maximum subsidence. According to Ru Li et al. [19], there are three pathways of callus pattern progression; the 2–6–9 pathway is a homogeneous pathway with the best result and the 3–7–10 is a heterogeneous pathway with a good result. The other callus patterns are included in mixed types and give variable results. Callus types 6, 9, and 10 were considered good and types 7 and 8 represented abnormality in bone regeneration. Thus our results confirm the findings of Ru Li et al. [19], and callus pattern can be used to judge the time of fixator removal to prevent callus subsidence. Subsidence varied significantly among the callus shapes with fusiform and concave having minimum subsidence, cylindrical having intermediate subsidence, and lateral having maximum subsidence. Ru Li et al. [19] also claimed that the fusiform and cylindrical callus indicated better healing potential with lateral callus having poor healing potential. However, the concave callus also indicated poor healing potential and in our study it had lowest subsidence. This may be due to confounding factors such that all cases with concave pattern had type 9 calluses and all of them had lengthening less than 10 cm. Mamada et al. [21] demonstrated a significant increase in the fracture rate when the CDR was less than 80%. We did not find a correlation between CDR and tibia subsidence in our study, but only four of our patients had a CDR less than 0.8 or 80% and there were no fractures in our series.
Cases with complete formation of fourth cortex (type 2 callus) at the time of fixator removal did not significantly decrease the overall subsidence rate when compared to limbs having only three cortices (type 1 callus) at the time of fixator removal. This indicates that callus with at least three cortices visible on plain radiograph has capacity comparable to callus having all four cortices regenerated in resisting callus subsidence. Thus the hypothesis of removing the fixator when at least three cortices have regenerated is a sound hypothesis to judge the time of fixator removal. However, when these two types were compared on the basis of amount of lengthening, patients with three cortices at time of fixator removal had significantly more subsidence than the patients with fourth cortex regenerated at the time of fixator removal. Thus, in cases with lengthening more than 10 cm or more than 50% of original length, it would be advisable to wait for the fourth cortex to be fully formed before removing the external fixator.
Our study has few drawbacks. The study tries to link the tibia subsidence to various factors in retrospective analysis. The results of univariate analysis showed few factors to significantly affect the results; however, multiple regression analysis showed only two factors, namely, amount of distraction and callus pattern, to be significant; thus, showing the major effect of the confounding factors in the univariate analysis. Thus the combined results would just help us detect the general trend in the factors that affect the tibia subsidence. The conclusions of our study might be stated as:
Tibia callus subsidence is a significant delayed complication seen in about half of the patients in our series.
Factors like aetiology, amount of distraction, callus pattern, callus shape, and BMD ratio significantly affect tibia subsidence.
Factors that affect tibia subsidence can be considered in determining the time of fixator removal in tibia lengthening by the Ilizarov ring fixator. BMD ratio more than 0.85 significantly prevents tibia subsidence and, in turn, prevents callus fracture and delayed callus angulation.
Patients having negative attributes at the time of fixator removal such as BMD ratio less than 0.85, lengthening beyond 50% or more than 10 cm, and patients with bone dysplasia will have high chances of callus subsidence.
In cases with lengthening more than 10 cm or more than 50% of original tibia length, presence of three cortices seems inadequate, and extending the time of fixator removal until the fourth cortex is also well formed is advisable to prevent delayed tibia subsidence.
References
- 1.Aldegheri R, Renzi-Brivio L, Agostini S. The callotasis method of limb lengthening. Clin Orthop Relat Res. 1989;241:137–145. [PubMed] [Google Scholar]
- 2.Aldegheri R. Distraction osteogenesis for lengthening of the tibia in patients who have limb-length discrepancy or short stature. J Bone Joint Surg [Am] 1999;81:624–634. doi: 10.2106/00004623-199905000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Antoci V, Ono CM, Antoci V, Jr, Raney EM. Bone lengthening in children: how to predict the complications rate and complexity? J Pediatr Orthop. 2006;26(5):634–640. doi: 10.1097/01.bpo.0000229977.31931.69. [DOI] [PubMed] [Google Scholar]
- 4.Aronson J, Good B, Stewart C, Harrison B, Harp J. Preliminary studies of mineralization during distraction osteogenesis. Clin Orthop Relat Res. 1990;250:43–49. [PubMed] [Google Scholar]
- 5.Aronson J, Gao GG, Shen XC, McLaren SG, Skinner RA, Badger TM, Lumpkin CK., Jr The effect of aging on distraction osteogenesis in the rat. J Orthop Res. 2001;19(3):421–427. doi: 10.1016/S0736-0266(00)90025-1. [DOI] [PubMed] [Google Scholar]
- 6.Vargas Barreto B, Caton J, Merabet Z, Panisset JC, Pracros JP. Complications of Ilizarov leg lengthening: a comparative study between patients with leg length discrepancy and short stature. Int Orthop. 2007;31:587–591. doi: 10.1007/s00264-006-0236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Catagni MA, Lovisetti L, Guerreschi F, Combi A, Ottaviani G. Cosmetic bilateral leg lengthening: experience of 54 cases. J Bone Joint Surg [Br] 2005;87(10):1402–1405. doi: 10.1302/0301-620X.87B10.16468. [DOI] [PubMed] [Google Scholar]
- 8.Codivilla A. On the means of lengthening, in the lower limbs, the muscles and tissues which are shortened through deformity. Am J Orthop Surg. 1905;2:353–369. [Google Scholar]
- 9.Dahl MT, Gulli B, Berg T. Complications of limb lengthening: a learning curve. Clin Orthop Relat Res. 1994;301:10–18. [PubMed] [Google Scholar]
- 10.Donnan LT, Saleh M, Rigby AS, McAndrew A. A radiographic assessment of bone formation in tibia during distraction osteogenesis. J Pediatr Orthop. 2002;22(5):645–651. doi: 10.1097/00004694-200209000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop Relat Res. 1994;301:31–37. [PubMed] [Google Scholar]
- 12.Gross RH. An evaluation of tibial lengthening procedures. J Bone Joint Surg [Am] 1971;53(4):693–700. [PubMed] [Google Scholar]
- 13.Hamanishi C, Yasuwaki Y, Kikuchi H, Tanaka S, Tamura K. Classification of the callus in limb lengthening. Radiographic study of 35 limbs. Acta Orthop Scand. 1992;63(4):430–433. doi: 10.3109/17453679209154761. [DOI] [PubMed] [Google Scholar]
- 14.Harp JH, Aronson J, Hollis M. Noninvasive determination of bone stiffness for distraction osteogenesis by quantitative computed tomography scans. Clin Orthop Relat Res. 1994;301:42–48. [PubMed] [Google Scholar]
- 15.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;238:249–281. [PubMed] [Google Scholar]
- 16.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;239:263–285. [PubMed] [Google Scholar]
- 17.Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990;250:8–26. [PubMed] [Google Scholar]
- 18.Kawamura B, Hosono S, Takahashi T, Yano T, Kobayashi Y, Shibata N, Shinoda Y. Limb lengthening by means of subcutaneous osteotomy. Experimental and clinical studies. J Bone Joint Surg [Am] 1968;50-A:851–878. [PubMed] [Google Scholar]
- 19.Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res. 2006;24(3):339–347. doi: 10.1002/jor.20026. [DOI] [PubMed] [Google Scholar]
- 20.Maffulli N, Lombari C, Matarazzo L, Nele U, Pagnotta G, Fixsen JA. A review of 240 patients undergoing distraction osteogenesis for congenital post-traumatic or postinfective lower limb length discrepancy. J Am Coll Surg. 1996;182(5):394–402. [PubMed] [Google Scholar]
- 21.Mamada K, Nakamura K, Matsushita T, Okazaki H, Shiro R, Ou W, Tanaka K, Kurokawa T. The diameter of callus in leg lengthening: 28 tibial lengthenings in 14 patients with achondroplasia. Acta Orthop Scand. 1998;69(3):306–310. doi: 10.3109/17453679809000936. [DOI] [PubMed] [Google Scholar]
- 22.Noonan KJ, Leyes M, Forriol F, Canadell J. Distraction osteogenesis of the lower extremity with use of monolateral external fixation. A study of two hundred and sixty-one femora and tibiae. J Bone Joint Surg [Am] 1998;80(6):793–806. doi: 10.2106/00004623-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]