Abstract
The aim of the study was to assess proprioception after shoulder arthroplasty. Twenty-six patients were enrolled who underwent total shoulder arthroplasty (TSA) (n = 13) or hemi-arthroplasty (n = 8) for shoulder osteoarthritis or reversed arthroplasty (n = 5) for cuff tear arthropathy. All patients were examined before the operation and then again six months thereafter in a motion analysis study with an active angle-reproduction (AAR) test. In all groups the AAR deteriorated at 60° flexion (from 5.5° [SD 2.8] to 7.6° [SD 2.7]; p = 0.007) and at 30° external rotation (ER) (from 6.5° [SD 3.6] to 7.3° [SD 4.8°]; p = 0.023) six months after surgery. In the subgroup of TSA, there was deterioration at 30° ER (p = 0.036). Otherwise, there were no significant changes within or among the subgroups. Proprioception, assessed by the AAR test, remained unchanged or deteriorated six months after shoulder arthroplasty. This might be related to the reduced pain or to the relatively short follow-up period.
Résumé
Le but de cette étude est d’évaluer la proprioceptivité des prothèses d’épaule. 26 patients ont bénéficié d’une arthroplastie totale (TSA) (n = 13) ou d’une prothèse intermédiaire hémi-arthroplastie (n = 8). Tous les patients présentaient une arthrose de l’épaule, enfin une arthroplastie inversée de type Grammont a été mise en place chez 5 patients pour des lésions associées de la coiffe. L’âge moyen était de 68,8 ans, SD 10,1 avec 20 femmes et 6 hommes. Les patients ont été examinés avant l’intervention et à six mois post-opératoire avec analyse de la mobilité à l’aide d’un test de reproduction angulaire (AAR) et comparaison avec un groupe contrôle de sujets sain.s Le test AAR s’est dégradé à 60° de flexion (5,5° à 7,6° p = 0.007) à 30° rotation externe (6,5° à 7,3° p = 0.023) six mois après la chirurgie. Dans le sous groupe des prothèses totales cette détérioration se fait à 30° RE (p = 0,036). Il n’y a pas de différence significative entre tous les sous groupes. La proprioception qui peut être évaluée par le test AAR a un aspect inchangé ou s’est dégradé six mois après la mise en place de la prothèse. Tout ceci est secondaire à la diminution de la douleur, à la libération tissulaire durant l’intervention et/ou à la période d’hospitalisation relativement courte.
Introduction
Shoulder arthroplasty can considerably improve the function of osteoarthritic shoulders [5, 9, 12]. Generally speaking, patients with glenohumeral osteoarthritis limited to the humeral head without eccentric erosion of the glenoid can be treated with hemiarthroplasty. If the glenoid shows (mostly posterior) eccentric wear, according to our concept the patient will receive total shoulder arthroplasty. This posterior wear is a typical feature of osteoarthritis of the shoulder and may be related to a contracture of the subscapularis muscle. Patients with a cuff tear arthropathy can be treated with a reverse arthroplasty. Parameters routinely examined in previous studies include pain, satisfaction, range of motion, and strength [3]. There is little information available about the proprioception of the osteoarthritic shoulder before and after arthroplasty [4].
Proprioception is directed by the central nervous system receiving feedback from the skin, tendons, muscles, and joint receptors. Recently, proprioception of the shoulder was examined after stroke [8]. In this case-control study, detection of passive motion was impaired in the ipsi- and the contralateral arm, whereas the passive position sense was not affected. The authors concluded that control of the muscle spindles and central integration or problems in processing the afferent signals provided by muscle spindles might cause these effects. These results highlight the fact that proprioception is a complex system that relies on central integration of various afferent and efferent elements.
The shoulder joint is balanced and centred by the rotator cuff and the glenohumeral ligaments. Therefore, it can be postulated that proprioception plays an important role in the postoperative outcome and rehabilitation. Proprioception can be defined as the ability to orientate the extremity without visual control and includes components of positioning, motion, and strength. There is no consensus on how proprioception should be measured because these different components are difficult to examine at the same time. Cuomo et al. performed a passive and guided angle-reproduction test in 20 patients with shoulder osteoarthritis before and six months after total shoulder arthroplasty (TSA) with only one degree of freedom at a time and reported improvement in proprioception [4]. In our study, we examined patients with different types of shoulder arthroplasties by means of an active and unlimited angle-reproduction test with 3D motion analysis to mimic the actions of their everyday life; the tests were conducted preoperatively and six months postoperatively. The findings may improve our understanding of the role of proprioception in postoperative rehabilitation after shoulder arthroplasty.
Patients and methods
Subjects
Patients with three different types of shoulder arthroplasties were examined:
Thirteen consecutive patients underwent third-generation total shoulder arthroplasty (TSA) (Aequalis Shoulder; Tornier, Lyon, France) for degenerative osteoarthritis of the humeral head and glenoid with a mean age of 69.8 years (standard deviation [SD] 7.2 years). There were eight women and five men (mean height 167 cm [SD 10]; mean weight 85.5 kg [SD 21.7]), with six right shoulders and seven left shoulders. In all cases the deltopectoral approach was used with detachment of the subscapularis tendon and release of the anterior parts of the inferior glenohumeral ligament. At the end of the surgery both structures were reattached to the humeral bone. Primary osteoarthritis was found in 11 cases and secondary post-traumatic osteoarthritis in two cases. The dominant side was involved in eight cases.
Eight consecutive patients underwent hemiarthroplasty (HEMI) for degenerative changes limited to the humeral head and a stable/minimally deformed glenoid of type A1 or A2 according to Walch [13]. There were seven women and one man, with three right shoulders and five left shoulders, three on the dominant sides and five non-dominant sides. In all cases the deltopectoral approach was used as described above. Osteoarthritis was primary in six cases and post-traumatic in two cases. The mean age was 64.6 years (SD 15), mean height was 165.3 cm (SD 5.6), and the mean weight was 72.6 kg (SD 10.9). Seven patients received a conventional third-generation hemiarthroplasty (Aequalis Shoulder; Tornier, Lyon, France) and one patient underwent humeral head resurfacing (Epoca RH CUP; Argomedical, Switzerland).
In five patients a reversed prosthesis was implanted for cuff tear arthropathy (REVERSE). All were women, their mean age was 73 (SD 4.6) years, mean height was 160 cm (SD 7.3), and mean weight was 73.6 kg (SD 7.4). In all cases the dominant right shoulder was treated. For all patients the anterior lateral approach was used with partial detachment of the anteriorlateral deltoid muscle and refixation in the end of the surgery. The subscapularis tendon was released at the humeral side and the anterior part of the inferior glenohumeral ligament at the glenoid.
A matched control group was comprised of five women and five men. Matched controls (n = 10; NORM) had a mean age of 64.5 years (SD 7.3). The mean height was 170.3 cm (9.3), and the mean weight was 78.2 kg (SD 11.6). All controls were right-hand dominant, healthy, and had normal shoulders. In this group the dominant was compared to the non-dominant hand.
The postoperative treatments with respect to medication and physical therapy were identical for all groups.
Joint angle analysis
The study protocol was approved by the local ethics committee, and informed consent was obtained from all patients and controls. The patients were examined the day before shoulder arthroplasty and six months after surgery by the same examiner.
A nine-camera motion analysis system (Vicon 612; Vicon, Lake Forest, USA) working at 120 Hz was used to monitor the patients’ movements. The spatial resolution of the system was approximately 1 mm. The underlying model consisted of seven segments: thorax, clavicles, upper arms, and forearms. The sternoclavicular joint and the glenohumeral joint were treated as a ball-and-socket joint, whereas the elbow was treated as a hinge joint. Translational degrees of freedom were not considered in any of these joints.
For the measurement, the patients were prepared with four markers placed on the trunk as recommended by the International Society of Biomechanics [14]. Four markers were placed on each forearm: one at the radial and one at the ulnar styloid process of the wrist and two, connected with a wand, on the ulna close to the elbow joint. One marker was placed laterally on the upper arm and one on the acromion. After a static trial, the patient was asked to perform isolated movements of elbow flexion/extension, shoulder flexion/extension and shoulder abduction/adduction to determine the shoulder joint position and the location of the elbow joint axis. Specifically, in these shoulder calibration trials the sternoclavicular joint was treated as a Cardan joint. Technical coordinate systems for the ulna/forearm, humerus, clavicle, and thorax were not deduced by optimisation methods as was done for marker clusters [1]. Instead, they were based directly on marker trajectories, i.e. the direction vectors between them, using cross-products as reviewed by Chiari et al. [2]. The technical coordinate system of the clavicle was based on the four thorax markers and the shoulder marker. This coordinate system was used only for dynamic calibration movements, which were limited to a range of shoulder motion of 0–60° flexion and abduction to exclude skin motion artefacts. Constraint least squares optimisation according to Gamage et al. was then used for joint centre determination [7].
The anatomical co-ordinate systems for the ulna/forearm, humerus, and thorax were based on the technical co-ordinate systems of these segments and on the joint axes and joint centres previously determined. A static trial was used to define the neutral position of the thorax. Angles of flexion and abduction were expressed as direction cosines relative to the proximal anatomical coordinate system, while internal/external shoulder rotation was defined according to the globe convention [6]. Elbow flexion was defined as the projected angle to the elbow axis. Custom software written in Java (Sun Microsystems, USA) was used to calculate each joint angle in each trial of the angle-reproduction tasks.
We validated our system and biomechanical model with the manual goniometer model and found intraclass correlation coefficients of 0.989 for intrasubject variability, 0.996 for intersubject variability, and 0.998 for intertester variability [11]. Differences of more than 10° between the two methods were found for shoulder flexion of more than 160° [11].
Angle-reproduction test
The test person sat on a chair with the arm hanging in 0° abduction and rotation. They were blindfolded to eliminate visual clues and wore sleeveless shirts. We ensured that the arm did not touch the trunk and, consequently, skin contact was minimised. The arm was moved to the desired position by the examiner with visual control of a manual handheld goniometer. In detail, the positions were 30° and 60° abduction, 30° and 60° flexion, and 30° external (and afterwards 30° internal rotation) in 30° of abduction (total six joint positions). In the target position the subjects were told to maintain the position for ten seconds (in the meantime a mean value of the joint position was measured), and then the initial position with the arm hanging was resumed. Afterwards, the subject was asked to move the arm back into the target position and the mean value of the joint position was measured. Standardised instructions were given to all subjects, and a test trial was conducted to acquaint them with each test condition. All tests were randomised for side and movement. Two test trials were performed at each angle, and the mean value was used for further analysis.
Statistics
The statistical analysis was performed using SPSS Version 14.0 (SPSS Inc., Chicago, IL, USA). Group mean values (MV) and standard deviations (SD) were calculated. P values <0.05 were considered significant. The distribution of the data was checked with the Shapiro-Wilk test, and the homogeneity of variance was assessed using the Levene test. The angle between the long axis of the humerus and the trunk position was determined. Differences in shoulder joint angles between target and reproduced position were compared between the pre- and postoperative examination with a paired t-test for the groups TSA, HEMI, and REVERSE. Afterwards, differences among these groups were examined by unifactorial ANOVA and post-hoc tests.
Results
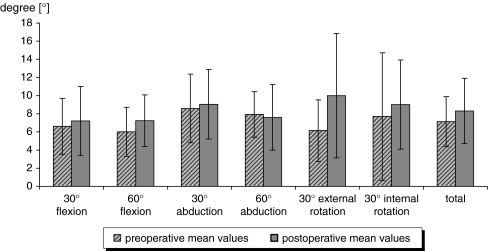
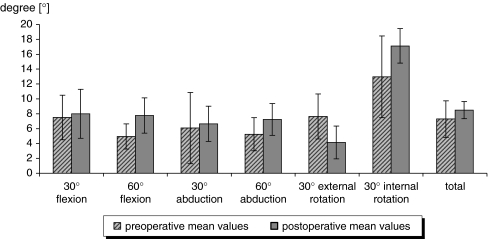
All results are summarised in Figs. 1, 2, 3 and 4 and Tables 1 and 2. In all groups, six months after arthroplasty the active angle reproduction (AAR) had deteriorated at 60° flexion (from 5.5° [SD 2.8] to 7.6° [SD 2.7]; p = 0.007) and at 30° external rotation (ER) (from 6.5° [SD 3.6] to 7.3° [SD 4.8°]; p = 0.023) (Table 1). There was significant deterioration of the mean AAR from 7° (SD 2.7) to 8.1° (SD 2.4°) (p = 0.005). In the TSA cohort, there was deterioration at 30° ER (p = 0.036) (Fig. 1). Otherwise, there were no significant changes within the subgroups or among the subgroups (Figs. 2 and 3; Table 2). There was no difference between the dominant and the non-dominant hand in the control group NORM (Fig. 4).
Fig. 1.
The total shoulder arthroplasty (TSA) subgroup revealed significantly lower AAR at 30° of external rotation six months after surgery
Fig. 2.
The hemiarthroplasty (HEMI) subgroup displayed no significant differences between pre- and postoperative AAR
Fig. 3.
The reversed arthroplasty (REVERSE) subgroup showed no significant differences between pre- and postoperative AAR, although the values at 60° of flexion almost attained significance (p = 0.057)
Fig. 4.
In the controls, the AAR test revealed no significant differences between the dominant and the non-dominant hand
Table 1.
Active angle reproduction (AAR) in all groups (TSA, HEMI, and REVERSE) before operation and six months thereafter
| Movement | Preoperatively | Six months postoperatively | P value | ||
|---|---|---|---|---|---|
| Mean (°) | SD (°) | Mean (°) | SD (°) | ||
| 30° of flexion | 7.2 | ±3.2 | 8.2 | ±2.9 | 0.067 |
| 60° of flexion | 5.5 | ±2.8 | 7.6 | ±2.7 | 0.007 |
| 30° of abduction | 7.2 | ±3.7 | 7.8 | ±3.4 | 0.431 |
| 60° of abduction | 6.5 | ±2.8 | 6.9 | ±2.9 | 0.320 |
| 30° of external rotation | 6.5 | ±3.6 | 7.3 | ±4.8 | 0.023 |
| 30° of internal rotation | 9.7 | ±6.2 | 10.8 | ±5.3 | 0.111 |
| Overall | 7.0 | ±2.7 | 8.1 | ±2.4 | 0.005 |
Positive values indicate deterioration of AAR
TSA total shoulder arthroplasty, HEMI hemiarthroplasty, REVERSE reversed arthroplasty, SD standard deviation
Table 2.
Comparison of AAR test in different types of arthroplasty before and six months after operation
| Movement | TSA | HEMI | REVERSE | P values | |||
|---|---|---|---|---|---|---|---|
| Diff. (°) | SD (°) | Diff (°) | SD (°) | Diff (°) | SD (°) | ||
| 30° of flexion | 1.6 | ±3.0 | 0.6 | ±3.1 | 0.5 | ±2.0 | 0.681 |
| 60° of flexion | 2.2 | ±4.9 | 1.2 | ±2.7 | 2.8 | ±2.3 | 0.697 |
| 30° of abduction | 0.7 | ±3.5 | 0.5 | ±4.6 | 0.6 | ±3.8 | 0.991 |
| 60° of abduction | 0.4 | ±4.2 | −0.3 | ±2.4 | 2.0 | ±2.8 | 0.522 |
| 30° of external rotation | 0.5 | ±3.8 | 3.8 | ±7.9 | −3.5 | ±4.0 | 0.765 |
| 30° of internal rotation | −0.7 | ±7.3 | 1.4 | ±5.8 | 4.2 | ±4.2 | 0.104 |
| Mean values | 0.8 | ±1.7 | 1.2 | ±1.9 | 1.1 | ±1.8 | 0.527 |
TSA total shoulder arthroplasty, HEMI hemiarthroplasty, REVERSE reversed arthroplasty, Diff difference, SD standard deviation
Positive values indicate deterioration of AAR. The p values indicate whether there were significant differences between the groups TSA, HEMI, and REVERSE
Discussion
The findings demonstrate that a component of proprioception, i.e. AAR, remains unchanged or deteriorates over the course of six months after shoulder arthroplasty.
Our findings can be compared to those of Cuomo and colleagues [4]. They prospectively analysed 20 consecutive patients with unilateral advanced glenohumeral arthritis who underwent TSA. Shoulder proprioception testing for passive position sense and detection of motion was performed one week before surgery and six months after TSA. Six months after TSA, position sense and the sensitivity of detection of motion were significantly improved (p < 0.05) and did not differ significantly from the contralateral shoulder or the controls. Cuomo et al. used a hydraulic machine that passively moved the arm. The patient had to indicate when he or she noted movement (“detection of motion”) and, in a separate approach, when he or she passively reassumed a joint position that was previously defined (“passive position sense”). Cuomo and colleagues thus measured two entities of proprioception separately. The AAR test that was used in our setting has more elements that can influence the outcome. The test person has to actively move the arm and is not limited regarding the direction of movement. Consequently, a more comprehensive concept of proprioception is used, comprising the elements of position sense, motion sense, and the strength that is necessary to reassume the position. This more comprehensive approach has more degrees of freedom and this might explain the difference between our findings and those of Cuomo and colleagues.
Moreover, nociceptors may play an important role. During the repeat measurement six months after arthroplasty, the patients mentioned that they were lacking the information input of pain that they had usually had during motion of the arm before surgery. The lacking afferent input might adversely influence the postoperative proprioception performance with the AAR. However, even if proprioception may not be improved after implantation of shoulder arthroplasty, a pain free increase of range of motion is the main improvement for the patient after surgery.
The AAR has been used to assess proprioception before, for example, in shoulder instability where Pötzl and colleagues examined the proprioceptive capabilities of 14 patients with recurrent anterior shoulder instability preoperatively and for at least five years postoperatively using the AAR test [10]. In their series the joint position sense improved significantly in abduction, flexion, and rotation (p < 0.05). They concluded that five years after surgical repair for shoulder instability the joint position sense improved significantly, to the same level as normal, healthy shoulders. It is possible that longer follow-up might show better results of the AAR in our cases, too. The operative approach for implantation of a shoulder TSA and hemiarthroplasty includes the cutting (and subsequent repair) of the subcapularis muscle and usually release of the inferior glenohumeral ligaments. In cuff tear arthropathy the subcapularis is damaged from the beginning or released during surgery. These structures contain afferent and efferent structures important for proprioception. The function of these structures might not have fully recovered by six months after the operation. Since the approach in TSA and hemiarthroplasty is identical, a comparison seems to be valid. The different approach and the lack of the rotator cuff in cuff tear arthropathy limits a direct comparison with the latter groups. However, the aim of the study was not the comparison of different approaches on proprioception, but the comparison of different types of implants that were implanted for different indications.
Our study has some limitations. The inclusion of consecutive patients resulted in an uneven distribution with regard to the type of arthroplasty. The numbers within the groups, especially in the REVERSE group, were relatively low. This can be partly explained by the complex and time-consuming nature of the measurements, but this should be addressed in future studies. The standard deviations within the subgroups were relatively high, which made it difficult to reach the level of significance. Nevertheless, there was a clear trend and several significant findings with deterioration or at least no improvement of the AAR test after shoulder arthroplasty. Since the AAR data also had a high standard deviation in the healthy control group (Fig. 4), this seems to be related not to the parameter evaluated (pre- and postoperative AAR), but rather to the person performing the test. Most likely the high standard deviations are not related to any inaccuracy of the measuring system, because its accuracy has been demonstrated in previous studies [11].
Conclusion
Performing shoulder arthroplasty did not positively affect the component of proprioception that was evaluated by the active angle-reproduction test. This is most likely attributable to the relatively short rehabilitation period of six months, which may well be insufficient for improvement of the complex central system responsible for the active joint position sense.
Footnotes
The study was supported by a grant of the Orthopaedic Hospital of the University of Heidelberg and the “Deutsche Arthrosehilfe e.V.”.
References
- 1.Carman AB, Milburn PD. Determining rigid body transformation parameters from ill-conditioned spatial marker co-ordinates. J Biomech. 2006;39:1778–1786. doi: 10.1016/j.jbiomech.2005.05.028. [DOI] [PubMed] [Google Scholar]
- 2.Chiari L, Della CU, Leardini A, Cappozzo A. Human movement analysis using stereophotogrammetry. Part 2: instrumental errors. Gait Posture. 2005;21:197–211. doi: 10.1016/j.gaitpost.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 160–164 [PubMed]
- 4.Cuomo F, Birdzell MG, Zuckerman JD. The effect of degenerative arthritis and prosthetic arthroplasty on shoulder proprioception. J Shoulder Elbow Surg. 2005;14:345–348. doi: 10.1016/j.jse.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14:471–479. doi: 10.1016/j.jse.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 6.Doorenbosch CA, Harlaar J, Veeger DH. The globe system: an unambiguous description of shoulder positions in daily life movements. J Rehabil Res Dev. 2003;40:147–155. [PubMed] [Google Scholar]
- 7.Gamage SS, Lasenby J. New least squares solutions for estimating the average centre of rotation and the axis of rotation. J Biomech. 2002;35:87–93. doi: 10.1016/S0021-9290(01)00160-9. [DOI] [PubMed] [Google Scholar]
- 8.Niessen MH, Veeger DH, Koppe PA, Konijnenbelt MH, Dieen J, Janssen TW. Proprioception of the shoulder after stroke. Arch Phys Med Rehabil. 2008;89:333–338. doi: 10.1016/j.apmr.2007.08.157. [DOI] [PubMed] [Google Scholar]
- 9.Orfaly RM, Rockwood CA, Jr., Esenyel CZ, Wirth MA. A prospective functional outcome study of shoulder arthroplasty for osteoarthritis with an intact rotator cuff. J Shoulder Elbow Surg. 2003;12:214–221. doi: 10.1016/S1058-2746(02)86882-3. [DOI] [PubMed] [Google Scholar]
- 10.Potzl W, Thorwesten L, Gotze C, Garmann S, Steinbeck J. Proprioception of the shoulder joint after surgical repair for instability: a long-term follow-up study. Am J Sports Med. 2004;32:425–430. doi: 10.1177/0363546503261719. [DOI] [PubMed] [Google Scholar]
- 11.Raiss P, Rettig O, Wolf S, Loew M, Kasten P. Range of motion of shoulder and elbow in activities of daily life in 3D motion analysis. Z Orthop Unfall. 2007;145:493–498. doi: 10.1055/s-2007-965468. [DOI] [PubMed] [Google Scholar]
- 12.Sande MA, Brand R, Rozing PM. Indications, complications, and results of shoulder arthroplasty. Scand J Rheumatol. 2006;35:426–434. doi: 10.1080/03009740600759720. [DOI] [PubMed] [Google Scholar]
- 13.Walch G, Boulahia A, Boileau P, Kempf JF. Primary glenohumeral osteoarthritis: clinical and radiographic classification. The Aequalis Group. Acta Orthop Belg. 1998;64(Suppl 2):46–52. [PubMed] [Google Scholar]
- 14.Wu G, Helm FC, Veeger HE, Makhsous M, Roy P, Anglin C, Nagels J, Karduna AR, McQuade K, Wang X, Werner FW, Buchholz B. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion–Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38:981–992. doi: 10.1016/j.jbiomech.2004.05.042. [DOI] [PubMed] [Google Scholar]