Abstract
In the last few years there has been great interest in minimally invasive plate osteosynthesis (MIPO) in the treatment of humeral shaft fractures. None of these studies showed the anatomical relationship between the radial nerve and the material of the implant in vivo. We performed postoperative ultrasonographic measurement of the distance between the radial nerve and the material implanted using the MIPO technique. Nineteen patients underwent postoperative ultrasound examinations. Group A comprised midshaft fractures and group B distal third fractures. The point of greatest proximity between the radial nerve and the implant was measured. In group A the distance was between 1.6 and 19.6 mm (mean: 9.3 mm) and in group B between 1.0 and 8.1 mm (mean: 4.0 mm). The ultrasound findings reveal that the radial nerve is quite close to the implant material, especially in the transition between the third and fourth quarters of the humeral shaft.
Résumé
Ce travail est l’étude par ultrasonographie des rapports entre le nerf radial et la plaque implantée par technique mini invasive (MIPO) dans le traitement des fractures de la diaphyse humérale. Dix neuf patients sont étudiés avec fracture à mi-diaphyse pour le groupe A et fracture du 1/3 distal pour le groupe B. Le point de plus grande proximité entre l’implant et le nerf a été mesuré: entre 1,6 et 19,6 mm pour le groupe A (moyenne 9,3 mm) et entre 1,0 et 8,1 mm pour le groupe B (moyenne 4,0 mm). L’étude montre la proximité entre le nerf radial et le matériel surtout à l’union 3/4 proximal et 1/4 distal.
Introduction
As of the year 2000, several publications have demonstrated the safe and efficient use of minimally invasive osteosynthesis in humeral shaft fractures with insertion of bridge plates (MIPO). All of the authors, some through clinical and others through anatomical studies, highlighted the importance of taking particular care in cases of radial nerve lesion, vulnerable along the spiral groove on the humeral shaft [1, 5, 9–11, 20].
Such studies, some resorting to helical while others favoured conventional implants, were consistent about the placement with the highest level of safety for implant fixation, which is the anterior surface of the humeral shaft in midshaft fractures or the anterior-lateral column surface in distal fractures. None of them, however, shows how far from the implant the radial nerve actually is and which is the area of greatest nerve vulnerability as a consequence of the proximity to the implant [1, 4, 5, 7–13, 19, 20].
The objective of this study is to disclose, by means of postoperative ultrasonography, the topographic relationships of the radial nerve along the area occupied by the surgical implant, thus determining the zones of greatest vulnerability and safety for the treatment of humeral shaft fractures using the MIPO technique.
Patients and methods
In the period between November 2000 and July 2007, 35 patients with humeral shaft fractures were treated by the MIPO technique. All of the patients were operated upon by the same surgeon (LB) in three hospitals located in the region of Campinas, SP, Brazil, always following the same surgical technique [9–11]. There were no cases of iatrogenic radial nerve lesion. Postoperative ultrasound examinations were performed in all patients.
Only 19 patients agreed to and were present for the examination. Of these patients 15 were men and four women, ranging in age from 20 to 73 years (mean: 40.52 years). The time between surgery and examination ranged between one and 80 months (mean: 32.0 months).
The patients were divided into two groups: group A with midshaft fractures where the plate was fixed to the anterior surface of the humeral shaft and moulding was not necessary (Fig. 1, Table 1) and group B with distal third fractures where the plate was fixed to the anterior surface of the lateral column of the humerus (Fig. 2, Table 2). In the latter situation, the plate was pre-moulded to fit to the contour of the distal third of the humerus and its proximal extremity slightly twisted internally to rest on the anterior surface of the humerus perfectly.
Fig. 1.
a Plate on the anterior surface of humeral shaft. b Clinical example of a midshaft fracture treated by MIPO (group A)
Table 1.
Patients with midshaft fractures treated by MIPO (group A)
| Number | Gender | Postoperative time (months) | Critical point (mm) |
|---|---|---|---|
| 1 | F | 1 | 1.6 |
| 2 | M | 6 | 14.2 |
| 3 | M | 80 | 14.2 |
| 4 | M | 72 | 13.8 |
| 5 | F | 17 | 3.2 |
| 6 | M | 21 | 13.9 |
| 7 | F | 65 | 4.9 |
| 8 | M | 32 | 3.4 |
| 9 | M | 1 | 1.9 |
| 10 | M | 22 | 19.6 |
| 11 | M | 1 | 6.2 |
| 12 | M | 31 | 2.5 |
| 13 | M | 7 | 3.1 |
| 14 | M | 76 | 15.4 |
Fig. 2.
a Plate on the anterior surface of lateral column of humeral shaft. b Clinical example of distal third fracture treated by MIPO (group B)
Table 2.
Patients with distal third fractures treated by MIPO (group B)
| Number | Gender | Postoperative time (months) | Critical point (mm) |
|---|---|---|---|
| 1 | M | 79 | 8.1 |
| 2 | M | 2 | 7.0 |
| 3 | F | 40 | 1.0 |
| 4 | M | 20 | 1.3 |
| 5 | M | 11 | 5.6 |
All examinations were carried out between July and August of 2007 by the same examiner (AKC) and with the same device, a Voluson 730 EXPERT® with a multifrequency linear probe manufactured by GE®.
The patients were seated on the examining table, with the upper limb at rest on the table and the elbow slightly bent. Longitudinal and transversal cuts were made to identify the radial nerve and its entire route, analysing its relationship to the plate fixed on the humerus. The distance between the nerve and the plate was then measured at the point where the distance was smaller, which was named the “critical point”.
To avoid distortion of the anatomical relationships of the structures being analysed, the pressure of the probe on the arm was minimal, just sufficient to identify and measure distances of interest.
After ultrasonographic determination of the critical point, the shaft of the humerus was clinically divided into four equal parts and then the critical point location was related to these four parts. Thus, there would be practical applicability of ultrasound findings. In other words, the surgeon would be able to easily identify, during the surgical procedure, the region of greater proximity between the nerve and the material to be implanted. This region was clinically determined and named the “critical zone”.
Results
In patients with midshaft fractures (group A), the distances obtained at the “critical point” ranged between 1.6 and 19.6 mm (mean: 9.3 mm). In patients with distal third fractures (group B), the distances obtained at the “critical point” ranged between 1.0 and 8.1 mm (mean: 4.0 mm).
As a consequence of sample heterogeneity, the chosen option was statistical analysis by a non-parametric method. There was no statistically significant difference between the two groups (p = 0.091).
Discussion
Whether its onset occurs during conservative or operative treatment, radial nerve palsy is the most common nervous lesion, causing long bone fracture complications [14, 15].
The radial nerve is the continuation of the posterior fascicle of the brachial plexus (C5, C6, C7, C8 and T1). Beginning in the shoulder behind the axillary artery, it continues along the posterior axillary wall (in front of the subscapularis, latissimus dorsi and teres major muscles) and then crosses the triangular space between the long head of the triceps brachii muscle, the shaft of the humerus and under the teres major muscle. In the arm, the nerve is located in the groove that takes its name, on the posterior surface of the humerus, between the lateral and medial heads of the triceps brachii. After crossing the back of the humerus, the nerve traverses the lateral intermuscular septum and goes into the anterior compartment, between the brachialis and brachioradialis muscles [16, 17].
Whitson (1954) [18] demonstrated that the radial nerve does not cross the radial groove located in the humeral shaft. Instead, for most of its route the nerve is separated from the humerus by 1.0–5.0 cm of muscle. The nerve is closely connected to the inferior portion of the radial groove, but not in direct contact with the same. Only a small part of the supracondylar ridge of the humerus is in close contact with the nerve and it is in this region that the nerve crosses the lateral intermuscular septum before reaching the surface of the brachioradialis muscle. At this point that the nerve has less mobility and greater susceptibility to mechanical lesions [6, 16–18].
In this last decade, minimally invasive osteosynthesis of humeral shaft fractures by means of bridge plates (MIPO) has been extensively used worldwide. Some authors choose helical implants, others prefer locking compression plates (LCP), while some, like us, use conventional implants. The common ground among all authors, with only small technical variations, is that the only safe region for this procedure is the anterior surface of the humerus. This is evidently due to anatomical peculiarities of the radial nerve, as already discussed [1, 4, 5, 7–13, 18, 20].
In 2007, Lau et al. published their experience with the MIPO technique using LCP implants in proximal humeral shaft fractures. The authors suggest that LCP implants be used especially in elderly and osteoporotic patients. In order to minimise complications, the authors advise staying at least 8.0 cm proximal to the lateral epicondyle to avoid radial nerve injury at the intermuscular septum [8].
Bodner et al. reported the use of the ultrasonographic examination to diagnose radial nerve compression syndromes. In these articles, the nerve was easily, clearly and safely identified, which motivated us to make use of the postoperative ultrasonographic examination for patients treated for humeral shaft fractures by the MIPO technique. The intention was to demonstrate in vivo, through an innocuous examination, the topographic relationship between the radial nerve and the material to be implanted [2, 3].
Although our previously published case study, along with those of other authors, might corroborate the safety of the method, we believe that the ultrasound mapping of the radial nerve in connection with the implant might better clarify how safe this technique actually is, in addition to providing data on sites of greater vulnerability and susceptibility to iatrogenic nervous lesion.
Our findings show that the nerve is closely related to the implant, mainly in the distal third of the humerus. Actually, the highest risk zone is located in the transition between the third and fourth quarters of the humeral shaft (Fig. 3). Such findings are consistent with classic anatomical studies that reveal that the radial nerve is closer to the diaphysis in the lateral intermuscular septum region, especially in its distal extremity [6, 14–18]. The surgeon should be aware of this fact when choosing the therapeutic method, mainly in more distal fractures (group B), where the plate will go up to the end of the distal third of the humerus.
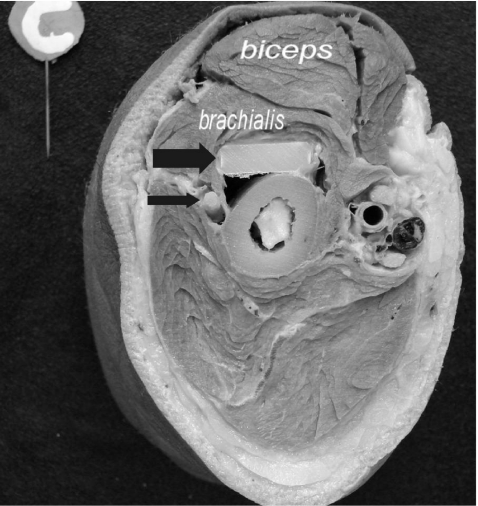
Fig. 3.
Anatomical piece of a distal fourth humeral shaft cut showing the close relationship between the radial nerve (narrow arrow) and the plate (broad arrow) inserted on the anterior surface of humeral shaft
From a statistical viewpoint, we were not able to demonstrate any significant difference between the two groups of operations performed concerning the higher probability of radial nerve lesion, since the number of cases with more distal fractures was very low. Perhaps with a larger number of cases, especially those involving more distal fractures, it will be possible to conclude that one or the other group presents a higher statistical risk of radial nerve lesion when treated by the MIPO technique.
Ultrasound findings show great variability of what we call the critical point, that is the point where the nerve is closest to the implant. In some patients, this distance was practically non-existant (1.0 mm) and in others around 14.0 mm. This great variation may be related to with the muscular mass of the patient, the presence of fracture haematoma in more acute cases, variations of fracture configurations or individual anatomical build, besides the possibility of small technical variations during the moulding process or site for implant fixation. Despite these variations, one constant factor of great practical importance can be found in every case: the critical point (determined by ultrasound) was closely related to the transition between the third and fourth quarters of the humeral diaphysis. In other words, the surgeon who opts for this technique should know beforehand that the critical zone, that is the point where the nerve is most vulnerable and susceptible to a lesion caused by the implant, is quite close to the transition between the third and fourth quarters of the humeral shaft.
In any case, as a result of the data obtained, it is extremely important for the surgeon to be aware of the required technical details to perform this procedure. Special care should be taken to introduce the implant delicately, in the subperiosteal region, in a distal to proximal direction in more distal fractures and from proximal to distal in midshaft fractures, always with the elbow joint in semi-flexion. Soft tissue handling should be as gentle and atraumatic as possible. Retractors should be very carefully handled to avoid damage to the radial nerve, by stretching or contusion. Retractors of the Hohmann type should be avoided. The implant should be accurately positioned, fixed and set on the anterior surface of the humeral shaft [9–11, 20]. It should be emphasised that the team interested in the use and application of this technique should undertake studies and training in an anatomy laboratory.
This study allows us to conclude that, although the clinical results presented by several authors in recent years have revealed that the MIPO technique applied to the treatment of diaphyseal humeral fractures is a safe and efficient method, the risk for radial nerve lesions is real and should not be undervalued, even when all technical precautions are followed. The decision to choose this method should be taken individually and on a case-by-case basis, analysing the type of fracture, staff training and its acceptance by the patient, after being duly informed of the potential risks involved.
References
- 1.Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005;36(4):530–538. doi: 10.1016/j.injury.2004.05.036. [DOI] [PubMed] [Google Scholar]
- 2.Bodner G, Buchberger W, Schocke M, Bale R, Huber B, Harpf C, Gassner E, Jaschke W. Radial nerve palsy associated with humeral shaft fracture: evaluation with US-initial experience. Radiology. 2001;219(3):811–816. doi: 10.1148/radiology.219.3.r01jn09811. [DOI] [PubMed] [Google Scholar]
- 3.Bodner G, Huber B, Schwabegger A, Lutz M, Waldenberger P. Sonographic detection of radial nerve entrapment within a humerus fracture. J Ultrasound Med. 1999;18(10):703–706. doi: 10.7863/jum.1999.18.10.703. [DOI] [PubMed] [Google Scholar]
- 4.Fernández Dell’Oca AA. The principle of helical implants. Unusual ideas worth considering. Injury. 2002;33(Suppl 1):SA1–SA27. doi: 10.1016/s0020-1383(02)00064-5. [DOI] [PubMed] [Google Scholar]
- 5.Hernández S, Dario R. Placa puente en húmero. Perspectiva de una técnica. Rev Colomb Ortop Traumatol. 2003;17(3):69–73. [Google Scholar]
- 6.Holstein A, Lewis GM. Fractures of the humerus with radial-nerve paralysis. J Bone Joint Surg Am. 1963;45:1382–1388. [PubMed] [Google Scholar]
- 7.Jiang R, Luo CF, Zeng BF, Mei GH. Minimally invasive plating for complex humeral shaft fractures. Arch Orthop Trauma Surg. 2007;127(7):531–535. doi: 10.1007/s00402-007-0313-z. [DOI] [PubMed] [Google Scholar]
- 8.Lau TW, Leung F, Chan CF, Chow SP. Minimally invasive plate osteosynthesis in the treatment of proximal humeral fracture. Int Orthop. 2007;31(5):657–664. doi: 10.1007/s00264-006-0242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Livani B, Belangero WD. Osteossíntese de fratura diafisária do úmero com placa em ponte: apresentação e descrição da técnica. Acta Ortop Bras. 2004;12(2):112–117. doi: 10.1590/S1413-78522004000200007. [DOI] [Google Scholar]
- 10.Livani B, Belangero WD. Bridging plate osteosynthesis of humeral shaft fractures. Injury. 2004;35(6):587–595. doi: 10.1016/j.injury.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Livani B, Belangero WD, Castro de Medeiros R. Fractures of the distal third of the humerus with palsy of the radial nerve: management using minimally-invasive percutaneous plate osteosynthesis. J Bone Joint Surg Br. 2006;88(12):1625–1628. doi: 10.1302/0301-620X.88B12.17924. [DOI] [PubMed] [Google Scholar]
- 12.Numbela BX, Aceves LH, González AB, Castro CT. Minimally invasive surgery in diaphyseal humeral fractures with helicoidal plate. One year result in seven patients (in Spanish) Acta Ortop Mex. 2007;21(05):239–426. [PubMed] [Google Scholar]
- 13.Pospula W, Abu Noor T. Percutaneous fixation of comminuted fractures of the humerus: initial experience at Al Razi hospital, Kuwait. Med Princ Pract. 2006;15(6):423–426. doi: 10.1159/000095487. [DOI] [PubMed] [Google Scholar]
- 14.Shao YC, Harwood P, Grotz MR, Limb D, Giannoudis PV. Radial nerve palsy associated with fractures of the shaft of the humerus: a systematic review. J Bone Joint Surg Br. 2005;87(12):1647–1652. doi: 10.1302/0301-620X.87B12.16132. [DOI] [PubMed] [Google Scholar]
- 15.Sisk TD. Fractures of shoulder girdle and upper extremity. In: Crenshaw AH, editor. Campbell’s operative orthopaedics, vol 3. 7. St. Louis: Mosby; 1987. pp. 1794–1799. [Google Scholar]
- 16.Testut L, Latarjet A. Tratado de anatomía humana, vol III. Barcelona: Salvat Editores; 1954. pp. 305–312. [Google Scholar]
- 17.Testut L, Jacob O. Tratado de anatomía topográfica con aplicaciones medicoquirúrgicas, vol II. Barcelona: Salvat Editores; 1977. pp. 708–723. [Google Scholar]
- 18.Whitson RO. Relation of the radial nerve to the shaft of the humerus. J Bone Joint Surg Am. 1954;36(1):85–88. [PubMed] [Google Scholar]
- 19.Zhiquan A, Bingfang Z, Yeming W, Chi Z, Peiyan H. Minimally invasive plating osteosynthesis (MIPO) of middle and distal third humeral shaft fractures. J Orthop Trauma. 2007;21(9):628–633. doi: 10.1097/BOT.0b013e31815928c2. [DOI] [PubMed] [Google Scholar]
- 20.Ziran BH, Belangero WD, Livani B, Pesantez R. Percutaneous plating of the humerus with locked plating: technique and case report. J Trauma. 2007;63(1):205–210. doi: 10.1097/01.ta.0000231870.11908.3e. [DOI] [PubMed] [Google Scholar]