Abstract
Between August 1986 and July 1997, we performed rotational acetabular osteotomy (RAO) according to the methods of Ninomiya and Tagawa in 161 patients (179 hips). Among them, 63 patients (68 hips) had advanced osteoarthritis. We assessed the outcome at a mean of 12 years after rotational acetabular osteotomy was performed for the treatment of advanced osteoarthritis in a series of patients with acetabular dysplasia. Eleven patients did not return for final follow-up and were excluded from the study, leaving 52 patients (57 hips) for analysis. The mean Merle d’Aubigné clinical score improved from 12.6 points (range 9–16) preoperatively to 14.3 points (range 7–18) postoperatively (p < 0.002), mainly because of increased scores for pain. At final follow-up, 50 of the 57 hips were still functioning. The results of rotational acetabular osteotomy for correction of advanced osteoarthritis in adults with acetabular dysplasia were satisfactory after a mean of 12.2 years.
Résumé
Entre août 1986 et juillet 1997, nous avons réalisé une ostéotomie de repositionnement du cotyle selon la méthode de Ninomiya et Tagawa chez 161 patients (179 hanches). Parmi ceux-ci, 63 patients (68 hanches) avaient une coxarthrose déjà évoluée. Nous avons évalué le devenir de ces patients à 12 ans de recul cette ostéotomie étant réalisée pour une coxarthrose déjà évoluée pour des patients présentant une dysplasie acétabulaire. 11 patients n’ont pas été revus et ont été exclus de l’étude il restait 52 patients (57 hanches) pour l’analyse. Le score moyen de Merle d’Aubigné a été amélioré de 12.6 points (de 9 à 16) en préopératoire à 14.3 points (de 7 à 18) en postopératoire (p < 0.002), ce score étant majoré surtout par la douleur. Au suivi final 50 des 57 hanches sont toujours fonctionnelles. En conclusion, on peut considérer que l’ostéotomie de rotation de l’accétabulum dans les cas de coxarthroses d’adultes déjà évoluées avec dysplasie acétabulaire permet d’avoir un résultat satisfaisant après un recul moyen de 12,2 ans.
Introduction
It is generally recognised that acetabular dysplasia is a predisposing factor for arthritis of the hip joint. The optimal treatment for advanced osteoarthritis that arises secondary to acetabular dysplasia of the hip is still controversial, particularly in young patients. Total hip arthroplasty has shown great efficacy for the treatment of advanced osteoarthritis of the hip joint, but there is a serious problem with regard to limited durability in the case of younger patients. There are also joint-preserving procedures, such as femoral osteotomy, arthrodesis, and acetabular osteotomy. Rotational acetabular osteotomy (RAO) has also been performed in patients with developmental dysplasia of the hip before the onset of osteoarthritic changes or at the early stage of osteoarthritis. Whether this procedure, when performed for the treatment of advanced osteoarthritis, can delay the need for total hip arthroplasty is not clear. Our hypothesis to perform rotational acetabular osoteotomy in the treatment of advanced osteoarthritis of the hip with dysplasia has been to focus on redistributing the weight bearing force by coverage of the osteotomised acetabulum over the femoral head and to improve joint function as well as relieve pain. In view of these objectives it has been essential to check preoperatively the widening of the joint space on plain radiograph in abduction. In this study, we assessed the outcome at a mean of 12 years after rotational acetabular osteotomy was performed for the treatment of advanced osteoarthritis in a series of patients with acetabular dysplasia.
Patients and methods
Between August 1986 and July 1997, we performed rotational acetabular osteotomy according to the methods of Ninomiya and Tagawa in 161 patients (179 hips) [5]. Among them, 63 patients (68 hips) had advanced osteoarthritis according to the criteria of the Japanese Orthopaedic Association (JOA) [7]. The definition of advanced osteoarthritis is narrowing of the joint space with cystic radiolucencies and small osteophytes, whereas end-stage osteoarthritis is characterised by loss of the joint space and large osteophytes. Grade 2 of Tönnis’s classification is equivalent to the advanced stage of the JOA radiographic classification [8]. Eleven patients did not return for final follow-up and were excluded from the study, leaving 52 patients (57 hips) for analysis.
There were 50 women and two men, and their mean age at the time of surgery was 45.2 years (range 21–59). The mean follow-up period was 148.6 months (range 24–254 months). Eighteen patients had unilateral dysplasia, and 32 patients had bilateral dysplasia.
The inclusion criteria for this study were an age younger than 60 years, advanced osteoarthritis of the hip according to the JOA classification, and improved femoral head coverage, joint congruency, and widening of the joint space on preoperative anteroposterior plain radiographs of the hip in abduction. No patient had end-stage arthritis according to JOA criteria, and seven hips were converted to total arthroplasty at operation.
Surgical procedure
RAO was performed according to the method of Tagawa and Ninomiya. The osteotomy line was marked about 1–1.5 cm from the acetabular rim, and a straight osteotome was inserted into the bone to a depth of about 1.5 cm. Then a curved osteotome was used to complete osteotomy through the inner wall of the ilium. After this was done, adequate coverage of the femoral head could be achieved by moving the acetabulum inferiorly and laterally. Capsulotomy was not performed. We inserted two to three cortical bone struts (about 5 mm thick) into the space between the rotated acetabulum and the ilium, and we supplemented these grafts with cancellous bone chips [6]. Two Kirchner wires (2 mm in diameter) were used to fix the rotated acetabulum and the cortical bone grafts to the ilium.
Postoperative management
Isometric exercises of the quadriceps femoris were performed during the first two weeks after surgery. Transfer to a wheelchair was commenced at two weeks postoperatively, and non-weight-bearing walking on two crutches was started at three weeks. Partial weight bearing was permitted after two months, while full weight bearing was resumed from four to six months after surgery [6].
Assessment
We investigated the symptoms of the patients and the findings on plain anteroposterior radiographs obtained at regular intervals (a minimum of one year). Clinical data were obtained by interview and physical examination. The hip joint scoring system of Merle d’Aubigné and Postel was used to grade function preoperatively and at the latest follow-up visit [4]. This system involves assigning scores for pain, mobility, and walking ability that range from zero to six points (higher scores reflect more normal performance). Then these scores are totalled to obtain overall clinical score. A score of 18 points is considered excellent, 15–17 is good, 13–14 is fair, and less than 13 implies a poor result. Radiological evaluation was performed by two coauthors (M.N. and K.M.). To compare coverage of the femoral head by the acetabulum before and after surgery, we determined the CE angle of Wiberg [10] and the acetabular head quotient (AHQ) of Heyman and Herndon [2]. To assess arthritic changes, the width of the joint space at the weight-bearing region was measured before surgery and at latest follow-up. Measurement was done at the lateral border, the medial border, and the centre of the weight-bearing region, and the average value was calculated. To assess medialisation of the femoral head, the postoperative change of the distance between the symphysis pubis and the medial border of the femoral head was measured. To assess distal translation of the femoral head, the distance between the lower margin of the lateral part of the pubis and the femoral head–neck junction was compared before and after surgery [6].
Statistical analysis
Preoperative and follow-up clinical hip scores and the radiographic parameters of acetabular position were compared with the paired t-test. The radiographic parameters of hip progression or improvement were compared with the unpaired t-test. Significance was defined as a p value <0.05.
Results
Clinical findings
The mean Merle d’Aubigné clinical score improved from 12.6 points (range 9–16) preoperatively to 14.3 points (range 7–18) postoperatively (p < 0.002), mainly because of increased scores for pain (i.e. reduction of pain). The mean pain score improved significantly from 3.1 points (range 1–5) to 4.7 points (range 1–6; P <0.0000000001). Although the mean mobility score decreased significantly from 5.4 points (range 3–6) to 4.9 points (range 2–6; P < 0.008), the mean walking ability score increased significantly from 4.0 points (range 2–6) to 4.6 points (range 2–6; P < 0.005). The total score decreased in 14 patients (14 hips), from a mean of 12.1 points (range 9–15) to a mean of 9.1 points (range 7–13). The postoperative score was ≧15 points for 35 hips and ≧17 points for 20 hips, but was <15 points for 22 hips. At final follow-up, 50 of the 57 hips were still functioning and only seven hips required total hip arthroplasty (THA). In six patients, THA was performed within ten years of the osteotomy procedure and it was performed after an interval of 12 years in the seventh patient. In these seven patients, the mean clinical score was 10.9 points (range 9–13) preoperatively.
Radiological findings
Radiological assessment showed progression of osteoarthritis in 26 hips, as reflected by narrowing of the joint space and enlargement of osteophytes or larger cysts. In the remaining 31 hips, the width of the joint space was preserved, and arthritic changes actually improved in 23 of these 31 hips (cysts in the acetabulum or femoral head diminished in nine hips). The mean correction of the centre-edge angle achieved by RAO was 36° (range 9–70°), with the mean value of the angle being 6° (range −27° to +21°) preoperatively and 42°(range 17–61°) postoperatively. The mean correction of the acetabular head quotient by RAO was 32% (range −6% to +65%), with a mean of 57% (range 33–78%) preoperatively and 89% (range 66–115%) postoperatively. The mean width of the joint space was 2.0 mm (range 0–6.0 mm) preoperatively which improved to 2.2 mm (range 0–5.0 mm) at the time of final follow-up (P = 0.5). The joint space was narrower postoperatively in all seven hips that were treated by THA. Medialisation of the femoral head was assessed from the mean change of the distance between the symphysis pubis and the medial border of the femoral head after surgery, and mean extent was 1.1 mm (range −15 to +15 mm). Twenty-nine hips showed medialisation, and 21 hips showed lateralisation. The mean change in the distance between the inferior margin of the lateral part of the pubis and the femoral head–neck junction after surgery was 4.5 mm (range −7 to +14 mm), with the mean preoperative distance being 6.3 mm (range −5 to +30 mm) and the mean postoperative distance being 1.8 mm (range −18 to +18 mm) (P < 0.001). In 44 hips, caudal shift was noted.
Comparison of radiological indices between the 26 hips with progression of arthritic changes and the 23 hips with improvement showed that the mean postoperative correction of the CE angle was 33° (range 9–70°) for the former hips versus 40° (range 22–62°) for the latter (P < 0.05). The mean postoperative correction of acetabular head quotient was 29% (range −6 to +65%) for hips with progression versus 36% (range 18–52%) for hips with improvement (P = 0.06). The mean preoperative joint space width was 1.7 mm (range 0–4.0 mm) in hips with progression and 2.8 mm (range 0.5–6.0 mm) in hips with improvement (P < 0.02), while the mean postoperative joint space width was 1.7 mm (range 0–5.0 mm) and 3.5 mm (range 0.5–6.0 mm), respectively (P < 0.0001) (Table 1). The mean extent of medialisation of the femoral head was 0.2 mm (range −12 to +10 mm) in hips with progression versus 3.0 mm (range −15 to +20 mm) in hips with improvement (P = 0.2).
Table 1.
Mean and range of the radiological indices for 26 hips with progression of arthritic changes and 23 hips with improvement of arthritic changes
| Improvement (n = 26) | Progression (n = 23) | |||
|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | |
| CE-angle (°) | 5 (−17 to +21) | 45* (27–59) | 6 (−14 to 20) | 39* (18–61) |
| Acetabular head quotient (%) | 56 (34–71) | 92 (78–110) | 57 (40–78) | 86 (67–115) |
| Width of the joint space (mm) | 2.8** (0.5–6.0) | 3.5*** (0.5–6.0) | 1.7** (0–4.0) | 1.7*** (0–5.0) |
*P < 0.05 compared with the preoperative value
**P < 0.01 compared with the preoperative value
***P < 0.0001 compared with the preoperative value
No intraoperative complications or postoperative complications were observed, including perforation of the joint by the chisel, infection, avascular necrosis of the rotated acetabulum, or delayed union at the osteotomy site. Heterotopic ossification also did not occur.
In the patients who required THA, operations were uneventful procedures with no need for acetabular reconstruction, and there was no loosening of the acetabular component at the latest follow-up.
Discussion
The management of comparatively young patients with acetabular dysplasia and concurrent degenerative hip joint disease is controversial. The most physiological solution for a young adult who has a dysplastic hip with degenerative osteoarthritis seems to involve shifting the acetabulum to a more normal position. Trousdale et al. [9] reported that patients who had severe osteoarthrosis did not fare as well and obtained significantly lower Harris hip scores and a higher rate of additional operations after periacetabular osteotomy. Hellemondt et al. [1] reported on 51 dysplastic hips treated by triple osteotomy, with good to excellent results in 64% after a mean follow-up period of 15 years. The variables that predicted poor long-term results in their study were the presence of osteoarthritic changes and a fair or poor clinical score preoperatively. They suggested that osteotomy involving the movement of hyaline cartilage might not be suitable for the treatment of advanced osteoarthritis. Ito et al. [3] reported that the Chiari osteotomy may be an option for younger patients with osteoarthritis who prefer a joint-conserving procedure to total hip arthroplasty and accept that the outcome will probably be less optimal than that achieved by total arthroplasty. On the other hand, Yasunaga et al. [11] reported that patients with advanced arthritis (according to the JOA criteria) and at least fair preoperative congruency, good postoperative congruency, a minimum preoperative joint space ≧2.2 mm, and a minimum postoperative joint space width ≧2.5 mm, could have a successful outcome following RAO, even in the sixth decade of life.
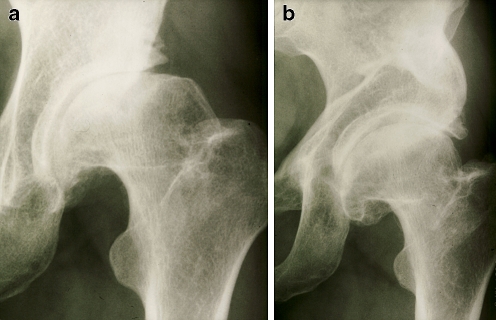
In our study, the postoperative joint space width was the most important factor that influenced the results of RAO. Postoperative narrowing of the joint space was usually associated with progression of arthritic changes. Accordingly, preoperative widening of the joint space in abduction seems to be required before performing RAO for the treatment of advanced osteoarthritis of the hip with dysplasia. Moreover, postoperative correction of the CE angle was significantly better in the 23 hips with improvement of arthritic changes; thus, along with the joint space width, adequate acetabular coverage after surgery is important. Okano et al. [7] reported that a less spherical femoral head led to progression of osteoarthritis over the long term after RAO in patients with advanced osteoarthritis, and concluded that postoperative results were dependent on the grade of femoral head deformity. In our series, if the joint space became wider in abduction preoperatively, the clinical and radiographic results were acceptable for more than ten years in spite of preexisting femoral head deformity (Fig. 1a,b).
Fig. 1.
a Radiographs of a 41-year-old woman with advanced osteoarthritis show narrowing of the joint space, femoral head deformity, and femoral head cyst. b Widening of the joint space and a decrease in the size of the cyst at 15 years after surgery
In 44 hips (77%), the femoral head was moved caudally and shortening of the lower limb did not occur. The extent of femoral head movement in the horizontal plane did not affect the postoperative results, because such movement of the femoral head was restricted by joint deformity.
We performed total hip arthroplasty after RAO in seven patients, and found that osteotomy did not adversely affect the acetabular anatomy or cause technical difficulties that compromised the outcome of total arthroplasty.
In conclusion, the results of rotational acetabular osteotomy for correction of advanced osteoarthritis in adults with acetabular dysplasia were satisfactory after a mean of 12.2 years. We found that widening of the joint space in abduction on preoperative radiographs was essential for a good result, as well as obtaining adequate coverage of the femoral head by acetabular rotation.
References
- 1.Hellemondt GG, Sonneveld H, Schreuder MHE, Kooijman MAP, Kleuver M. Triple osteotomy of the pelvis for acetabular dysplasia. J Bone Joint Surg [Br] 2005;87-B:911–915. doi: 10.1302/0301-620X.87B7.15307. [DOI] [PubMed] [Google Scholar]
- 2.Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg [Am] 1950;32-A:767–778. [PubMed] [Google Scholar]
- 3.Ito H, Matsuno T, Minami A. Chiari pelvic osteotomy for advanced osteoarthritis in patients with hip dysplasia. J Bone Joint Surg [Am] 2004;86-A:1439–1445. doi: 10.2106/00004623-200407000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Merle d’Aubigné R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg [Am] 1954;36-A:451–475. [PubMed] [Google Scholar]
- 5.Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg [Am] 1984;66-A:430–436. [PubMed] [Google Scholar]
- 6.Nozawa M, Shitoto K, Matsuda K, Maezawa K, Kurosawa H. Rotational acetabular osteotomy for acetabular dysplasia. J Bone Joint Surg [Br] 2002;84-B:59–65. doi: 10.1302/0301-620X.84B1.12299. [DOI] [PubMed] [Google Scholar]
- 7.Okano K, Enomoto H, Osaki M, Shindo H. Rotational acetabular osteotomy for advanced osteoarthritis secondary to developmental dysplasia of the hip. J Bone Joint Surg [Br] 2008;90-B:23–26. doi: 10.1302/0301-620X.90B1.19665. [DOI] [PubMed] [Google Scholar]
- 8.Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. New York: Springer; 1987. pp. 165–171. [Google Scholar]
- 9.Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg [Am] 1995;77-A:73–85. doi: 10.2106/00004623-199501000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand Suppl. 1939;83:1–135. [Google Scholar]
- 11.Yasunaga Y, Ochi M, Terayama H, Tanaka R, Yamasaki T, Ishii Y. Rotational acetabular osteotomy for advanced osteoarthritis secondary to dysplasia of the hip. J Bone Joint Surg [Am] 2006;88-A:1915–1919. doi: 10.2106/JBJS.E.00715. [DOI] [PubMed] [Google Scholar]