Abstract
Femoral malrotation in total knee arthroplasty causes flexion gap instability. Conventional instruments mostly reference the posterior condylar angle (PCA). The aim of this study was to verify whether the computer-navigated flexion gap (GAP) method produces a rectangular flexion gap and if a balanced flexion gap could also be achieved by referencing the PCA. A total of 100 knee prostheses were analysed using the navigated GAP method, and flexion gap symmetry along with femoral rotation were recorded. The GAP technique resulted in a rectangular flexion gap with adequate femoral rotational alignment. If the PCA technique had been used, only 51% of the femoral components would have been implanted in correct femoral rotation; the remaining 49% would have implanted with flexion gap instability. The GAP technique produces a rectangular flexion gap. The referencing of the PCA was shown to be less reliable. Thus, modern knee prosthesis instrumentation should not base femoral rotation solely on the PCA.
Résumé
Les anomalies de rotations fémorales peuvent être à l’origine d’instabilité dans les prothèses totales du genou. Le matériel ancillaire conventionnel a pour référence l’angle postérieur des condyles (PCA). Le but de cette étude est de vérifier grâce à la navigation (GAP) si l’on peut avoir une meilleure balance ligamentaire et un meilleur équilibrage qu’en faisant référence à la PCA. Matériel et méthode: 100 prothèses de genou ont été analysées en utilisant la navigation de type GAP et les anomalies de l’espace en flexion et rotation ont été rapportées. Résultats: la technique utilisant la navigation de type GAP permet d’avoir un bon alignement en rotation alors que la technique conventionnelle faisant référence au condyle postérieur ne permet d’avoir une bonne implantation que dans 34% des cas, les 66% de cas restant présentent une instabilité. En conclusion: la technique avec navigation permet d’avoir un espace en flexion parfaitement rectangulaire, la référence au condyle postérieur est moins fiable. Le matériel ancillaire moderne des prothèses du genou ne doit plus se baser uniquement sur les condyles postérieurs en flexion.
Introduction
Femoral component rotation in total knee arthroplasty (TKA) is essential for patellofemoral tracking, flexion gap balance and normal kinematic function [14, 18–20, 24]. Femoral malrotation frequently causes patellofemoral and flexion gap instability, one of the most common complications after TKA [1, 3, 18–20].
Proper rotational alignment of the femoral component is challenging and at least four different techniques exist: the bone landmark referencing procedures [orientation on the Whiteside line (WSL) [23], the posterior condylar angle (PCA) [8], the transepiconylar axis (TEA) [2]] and the soft tissue-dependent balanced flexion gap (GAP) method [5, 22].
The PCA technique is used by most of the conventional instruments for implantation of a TKA [2, 8, 11, 16, 21, 22]. Despite this fact, several studies indicate an alarming margin of error for the bone landmark referencing techniques, especially for the frequently used PCA method, with a rotational deviation range up to 29° [2, 6, 10, 14, 17, 21, 24].
Recent in vivo experiments indicate a more precise rotational alignment of the femoral component when using the GAP technique in combination with a computer navigation device [24].
The first goal of this study was to verify if the computer-navigated GAP method produces a balanced, symmetrical flexion gap in routine clinical practice. The second goal was to evaluate whether the correct rotation of the femoral component, and therefore a rectangular flexion gap, could have been achieved using the PCA technique.
Materials and methods
Data from 100 patients suffering from primary gonarthrosis and receiving a primary total knee replacement between April 2006 and December 2007 were retrospectively analysed. The posterior cruciate ligament-preserving PFC implant (DePuy, Leeds, UK) was implanted in all of these patients. Imageless computer navigation was performed using the Ci Software (DePuy, Leeds, UK). As described above the soft tissue-dependent balanced flexion gap method (GAP technique) was used for rotational alignment of all femoral implants.
Surgical technique A standard anterior approach was used, and the joint was opened with a medial, parapatellar incision. The patella was briefly inverted for optional trimming and was then returned to its normal, intra-surgical position. The anterior cruciate ligament was sacrificed, and arrays for the navigation device were attached on both the femoral and tibial shafts. The navigation software was started and the following point clusters were recorded: hip rotation centre, medial and lateral malleolus, medial, lateral, anterior and posterior point of the tibial head, tibial slope, tibial anterior cortex, tibia plateau, medial and lateral femoral epicondyles, WSL, femoral anterior cortex and medial and lateral condyle. From these data the Ci Software calculated an optimal tibial resection. The tibial cut was made perpendicular to the mechanical axis of the tibia, followed by a verification of cut accuracy. In order to determine the extension and flexion gap, a tension device was inserted into the joint gap and distended in full extension and 90° flexion of the knee joint. Thereafter, ligament balancing was performed. For the knees with residual varus deformity, the superficial medial collateral ligament was released subperiosteally from the medial surface of the proximal tibia down to the level proximal to the insertion of the pes anserinus. For the knees with residual valgus deformity, the iliotibial band, followed by the lateral collateral ligament, were released in sequence. The tension device was again distended in extension and flexion in order to measure extent and symmetry of the joint gaps (Fig. 1). The navigation system calculated the desired position and rotation of the femoral component, which was then adjusted to achieve a rectangular flexion gap (GAP method). The PCA was calculated by clusters of points acquired on the medial and lateral posterior condyles. With regard to the registration process of the PCA an accuracy of the navigation device of ± 1° was assumed [12, 13]. The relationship of the planned femoral rotation to TEA, WSL and PCA, as recorded by the navigated registration process, is shown in Fig. 2. Thereafter, the femoral bone cuts were performed, each followed by a verification step. Once the prostheses had been positioned correctly, the final implant position as well as flexion and extension gap symmetry were verified by the navigation system (Fig. 3). All data were recorded by the Ci Software. A t-test was performed, and results were considered significant if the p value was < 0.05.
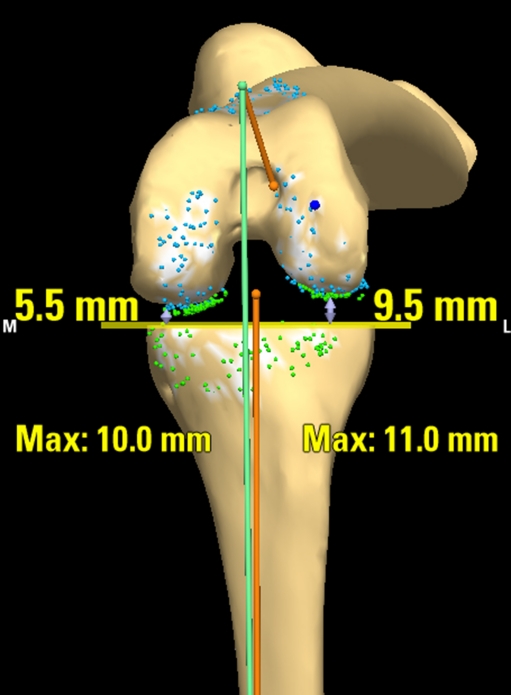
Fig. 1.
Flexion joint gap with tension device. After tibial resection and ligament balancing the tension device is inserted into the knee joint and is distracted at 90° flexion. The extent and symmetry of the flexion gap (5.5 mm medial, 9.5 mm lateral) is recorded
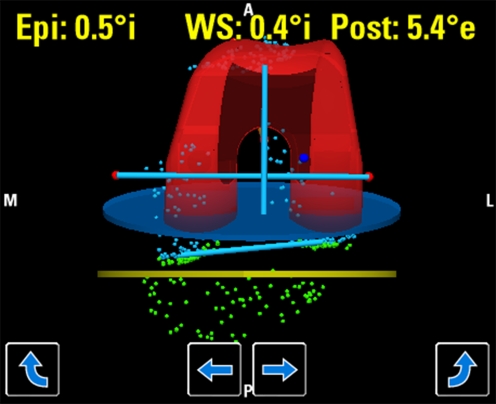
Fig. 2.
Relationship of the planned femoral rotation to TEA, WSL and PCA. The navigation software calculates the optimal femoral rotation to obtain a rectangular flexion gap. The differences between the rotation of the femoral component and the TEA (0.5° internal rotation), WSL (0.4° internal rotation) and PCA (5.4° external rotation) are shown
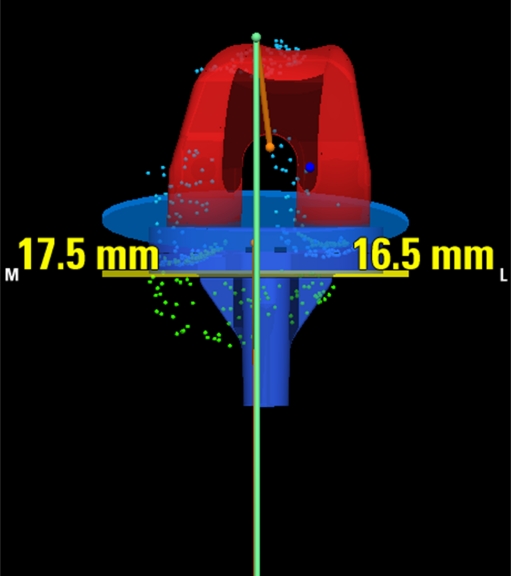
Fig. 3.
Verification of the final flexion gap. After implanting the prosthesis the symmetry of the flexion gap is measured and compared to the intra-surgical planning. For this patient, the flexion gap difference of 4.0 mm after tibial cut and ligament balancing (Fig. 1) had been reduced to 1.0 mm
Results
Complete data were available for 97 patients (97%). Navigation was aborted, and a conventional technique had to be implemented, for eight patients due to loss of the navigation arrays (8%).
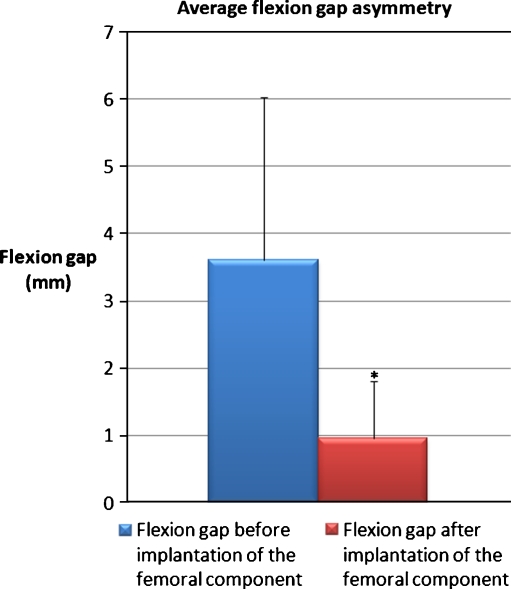
Flexion gap asymmetry The average difference between medial and lateral joint gap in 90° flexion after tibial bone cut and ligament balancing was 3.6 mm (0–9.7 mm, SD: 2.4 mm). After implantation of the prostheses, the difference between medial and lateral flexion gap at 90° was significantly reduced to 0.9 mm (0–4.0 mm, SD: 0.8 mm, p < 0.001, Fig. 4).
Fig. 4.
Average flexion gap asymmetry. The average differences between medial and lateral flexion gap before and after implantation of the femoral component are shown. After implantation of the femoral prosthesis the flexion gap asymmetry was significantly reduced from 3.6 mm to 0.9 mm (*p > 0.001)
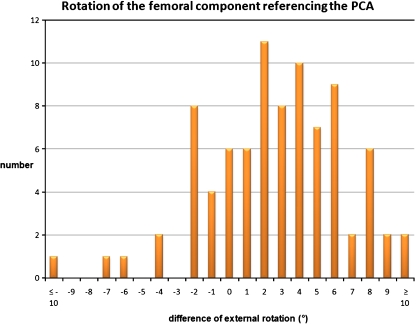
Rotation of the femoral implant As mentioned in the methods section the rotation of the femoral implant was compared to the registered PCA. Referencing the PCA the femoral components were implanted with an average external rotation of 4.4° (11.5° internal rotation - 11.8° external rotation, SD: 3.7°; Fig. 5). The common fixed possibilities if using conventional instruments along with the PCA method for rotational alignment are 0° or 3° external rotation. In our study only 45 femoral components (51%) were implanted in 0° (±1°) or 3° (±1°) external rotation referenced to the PCA. Hence, the remaining 49% of the prostheses would have been implanted with flexion gap instability using the PCA method. Furthermore, in 38 patients (44%) the femoral prosthesis would have been inserted in an internal malrotation.
Fig. 5.
Rotation of the femoral component referencing the PCA. The differences between rotation of the femoral component and the PCA are shown. Only 45 femoral components (51%) were implanted in 0° (± 1°) or 3° (± 1°) external rotation referenced to the PCA. Furthermore by use of the PCA method 38 prostheses (44%) would have been implanted in an internal malrotation
Discussion
The proper rotation of the femoral component in total knee arthroplasty is essential in avoiding symptomatic flexion gap asymmetry and patellar complications [14, 17, 22]. A well-established guideline concerning femoral component rotation is to avoid an internal rotation of the implant, as such malrotation of the femoral component makes the patella appear laterally tilted and increases the Q angle [1, 18].
It is generally accepted that the optimal rotation of the femoral component is parallel to the TEA, as the TEA approximates the flexion-extension axis of the knee [4, 6, 14, 22, 24]. However, finding the correct rotation during surgery is challenging because the tips of the medial and lateral epicondyles are often covered by soft tissue such as collateral ligaments and are therefore difficult to locate exactly [9, 25]. Studies show an alarming margin of error. A femoral malrotation over 5° from the TEA was found in 83% of all cases where only bone landmarks, such as the epicondyles, were referenced for rotational alignment [21, 24]. A recently published anatomical study using computer navigation and the TEA technique showed that only 17% of the knees were rotated < 5° from the referenced TEA [25].
In vivo studies compared these bone landmark techniques (TEA, WSL, PCA) and the soft tissue-dependent GAP technique. It was shown that in order to achieve a proper rotation of the femoral component as well as a rectangular flexion gap the GAP method was superior [22, 24]. Therefore, this technique was chosen and combined with a computer navigation device.
In this study the GAP technique resulted in a rectangular flexion gap with a reliable rotational alignment of the femoral component. Similar results have been published by other workgroups [22, 24]. In contrast, Handa et al. performed an anatomical study and reported an external malrotation of the femoral component when using the GAP technique [7]. It should be noted that Handa et al. had not carried out ligament balancing before femoral rotational adjustment. However, when using the GAP technique, an adequate ligament release, resolving ligament contractions, is always obligatory before rotational alignment of the femoral component. Correct rotation cannot be achieved should this step be omitted.
A shortcoming of this study is that the femoral rotation, referencing the anatomical TEA, was not verified on a computed tomography (CT) scan. Studies have proven an accuracy of navigation devices of ± 1° [12, 13]. But as mentioned above, referencing bone landmarks such as the epicondyles during the surgical procedure is always critical [9–11, 21, 24, 25]; furthermore, a magnification of the measurement error due to the small distance to the knee joint occurs. Hence, the accuracy of navigation devices with respect to the rotational alignment of the femoral component by registration of the epicondyles or WSL is certainly more imprecise [25]. Hence, in our study no correlation between registered TEA and rotation of the femoral component was calculated as the assumed accuracy was too uncertain.
By contrast the registration process of the posterior condyles is not comparable to the registration and therefore calculation of the TEA: the reasons for the low accuracy of the registered epicondyles are covering soft tissue, an overhanging lateral patella and uncertain identification due to anatomical variations [9, 10, 21, 24, 25]. These limitations do not exist for the registration process of the posterior condyles: they are not covered by any soft tissue and are always identified clearly. Furthermore, the software calculates the PCA from point clusters acquired on the medial and lateral posterior condyles. Thus, the PCA is not calculated from simply two points anymore, but it is instead determined from approximately 150 points. Summing up; in our opinion there is no doubt that in view of the registered PCA the proven accuracy of ± 1° for navigation devices can be assumed [12, 13].
A central question in this work was whether the rectangular flexion gap could also be achieved by referencing the PCA for rotational alignment of the femoral component. The PCA method with a fixed external rotation of 0° or 3° is used by most of the conventional TKA instruments [15, 22]. This study identified a significant discrepancy between the PCA and the required rotation of the femoral component to reach a rectangular flexion gap after ligament balancing. Hence, a correct rotational alignment of the femoral component would have been achieved for only 51% of the patients by using instruments which reference the posterior condyles with a fixed external rotation. The remaining 49% of the prostheses would have been implanted with flexion gap instability. Furthermore, 44% of the femoral components would have been implanted in an internal malrotation, an undoubtedly unfavourable situation. Analogous to these findings, other workgroups reported an inconsistent relationship between PCA and the correct rotation of the femoral component: This was especially true for valgus knee deformities, as the increased stress across the lateral joint surface leads to an increased abrasion of the lateral posterior condyle and therefore a greater PCA [6]. Furthermore, hypoplasia of the lateral posterior condyle is common in valgus deformities also resulting in an increased PCA [14]. In some patients PCAs differ up to 5° between the right and the left knee [6]. Others found a gender-specific difference between PCA and TEA [2].
Conclusion
This study showed that the navigated, ligament balancing GAP technique leads to a rectangular flexion gap with a reliably adequate femoral rotation. An accurate ligament balancing, which minimises contractures, is mandatory before rotational alignment of the femoral component. Ongoing CT-based studies are necessary to verify femoral components rotation after the ligament balancing GAP technique.
Our findings indicate that the commonly used referencing of the posterior condyles is unreliable in achieving a correct rotation of the femoral component along with a rectangular flexion gap. Thus, modern knee prosthesis instrumentation should not base femoral rotation solely on the PCA. Furthermore, it should allow for a flexible rotational adjustment of the femoral prosthesis.
References
- 1.Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–153. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–47. [PubMed] [Google Scholar]
- 3.Boyd AD, Jr, Ewald FC, Thomas WH, Poss R, Sledge CB. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am. 1993;75:674–681. doi: 10.2106/00004623-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Churchill DL, Incavo SJ, Johnson CC, Beynnon BD. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res. 1998;356:111–118. doi: 10.1097/00003086-199811000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Fehring TK. Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res. 2000;380:72–79. doi: 10.1097/00003086-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Griffin FM, Insall JN, Scuderi GR. The posterior condylar angle in osteoarthritic knees. J Arthroplasty. 1998;13:812–815. doi: 10.1016/S0883-5403(98)90036-5. [DOI] [PubMed] [Google Scholar]
- 7.Hanada H, Whiteside LA, Steiger J, Dyer P, Naito M. Bone landmarks are more reliable than tensioned gaps in TKA component alignment. Clin Orthop Relat Res. 2007;462:137–142. doi: 10.1097/BLO.0b013e3180dc92e7. [DOI] [PubMed] [Google Scholar]
- 8.Hungerford DS, Krackow KA. Total joint arthroplasty of the knee. Clin Orthop Relat Res. 1985;192:23–33. [PubMed] [Google Scholar]
- 9.Jenny JY, Boeri C. Low reproducibility of the intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Orthop Scand. 2004;75:74–77. doi: 10.1080/00016470410001708150. [DOI] [PubMed] [Google Scholar]
- 10.Jerosch J, Peuker E, Philipps B, Filler T. Interindividual reproducibility in perioperative rotational alignment of femoral components in knee prosthetic surgery using the transepicondylar axis. Knee Surg Sports Traumatol Arthrosc. 2002;10:194–197. doi: 10.1007/s00167-001-0271-x. [DOI] [PubMed] [Google Scholar]
- 11.Jiang CC, Insall JN. Effect of rotation on the axial alignment of the femur. Pitfalls in the use of femoral intramedullary guides in total knee arthroplasty. Clin Orthop Relat Res. 1989;248:50–56. [PubMed] [Google Scholar]
- 12.Laskin RS, Beksac B. Computer-assisted navigation in TKA: where we are and where we are going. Clin Orthop Relat Res. 2006;452:127–131. doi: 10.1097/01.blo.0000238823.78895.dc. [DOI] [PubMed] [Google Scholar]
- 13.Malik MH, Wadia F, Porter ML. Preliminary radiological evaluation of the Vector Vision CT-free knee module for implantation of the LCS knee prosthesis. Knee. 2007;14:19–21. doi: 10.1016/j.knee.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 14.McPherson EJ. Patellar tracking in primary total knee arthroplasty. Instr Course Lect. 2006;55:439–448. [PubMed] [Google Scholar]
- 15.Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE. Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:38–45. doi: 10.1097/00003086-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Newbern DG, Faris PM, Ritter MA, Keating EM, Meding JB, Berend ME. A clinical comparison of patellar tracking using the transepicondylar axis and the posterior condylar axis. J Arthroplasty. 2006;21:1141–1146. doi: 10.1016/j.arth.2006.02.171. [DOI] [PubMed] [Google Scholar]
- 17.Olcott CW, Scott RD. A comparison of 4 intraoperative methods to determine femoral component rotation during total knee arthroplasty. J Arthroplasty. 2000;15:22–26. doi: 10.1016/S0883-5403(00)91051-9. [DOI] [PubMed] [Google Scholar]
- 18.Rhoads DD, Noble PC, Reuben JD, Mahoney OM, Tullos HS. The effect of femoral component position on patellar tracking after total knee arthroplasty. Clin Orthop Relat Res. 1990;260:43–51. [PubMed] [Google Scholar]
- 19.Romero J, Stahelin T, Binkert C, Pfirrmann C, Hodler J, Kessler O. The clinical consequences of flexion gap asymmetry in total knee arthroplasty. J Arthroplasty. 2007;22:235–240. doi: 10.1016/j.arth.2006.04.024. [DOI] [PubMed] [Google Scholar]
- 20.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ. The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am. 2005;87:2276–2280. doi: 10.2106/JBJS.D.02945. [DOI] [PubMed] [Google Scholar]
- 22.Stiehl JB, Cherveny PM. Femoral rotational alignment using the tibial shaft axis in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:47–55. doi: 10.1097/00003086-199610000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Whiteside LA, Arima J. The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res. 1995;321:168–172. [PubMed] [Google Scholar]
- 24.Yau WP, Chiu KY, Tang WM. How precise is the determination of rotational alignment of the femoral prosthesis in total knee arthroplasty: an in vivo study. J Arthroplasty. 2007;22:1042–1048. doi: 10.1016/j.arth.2006.12.043. [DOI] [PubMed] [Google Scholar]
- 25.Yau WP, Leung A, Liu KG, Yan CH, Wong LL, Chiu KY. Interobserver and intra-observer errors in obtaining visually selected anatomical landmarks during registration process in non-image-based navigation-assisted total knee arthroplasty. J Arthroplasty. 2007;22:1150–1161. doi: 10.1016/j.arth.2006.10.010. [DOI] [PubMed] [Google Scholar]