Abstract
New technology using magnetic resonance imaging (MRI) allows the surgeon to place total knee replacement components into each patient’s pre-arthritic natural alignment. This study evaluated the initial intra-operative experience using this technique. Twenty-one patients had a sagittal MRI of their arthritic knee to determine component placement for a total knee replacement. Cutting guides were machined to control all intra-operative cuts. Intra-operative events were recorded and these knees were compared to a matching cohort of the senior surgeon’s previous 30 conventional total knee replacements. Post-operative scanograms were obtained from each patient and coronal alignment was compared to previous studies using conventional and computer-assisted techniques. There were no intra-operative or acute post-operative complications. There were no differences in blood loss and there was a mean decrease in operative time of 14% compared to a cohort of patients with conventional knee replacements. The average deviation from the mechanical axis was 1.2° of varus, which was comparable to previously reported conventional and computer-assisted techniques. Custom-fit total knee replacement appeared to be a safe procedure for uncomplicated cases of osteoarthritis.
Résumé
Objectif: les nouvelles technologies utilisant l’IRM doivent permettre aux chirurgiens de mettre en place de façon correcte les composants articulaires d’une prothèse de genou chez les patients et ce, d’une façon identique à l’axe articulaire préexistant à l’arthrose. Le but de cette étude est d’également évaluer en peropératoire l’utilisation de cette technique. Matériels et méthodes: 21 patients ont bénéficié d’une IRM sagittale du genou de façon à déterminer le positionnement des implants lors d’une prothèse totale. Les guides de coupe ont été préparés pour permettre cette évaluation en per oprératoire. Les évènements per opératoires ont été rapportés et ces genoux ont été comparés à une cohorte de 30 genoux traités de façon conventionnelle par le même chirurgien sénior. En postopératoire, une évaluation sur un grand film radiographique, dans le plan frontal, avec mesure des axes a été réalisée pour chaque patient en comparant la technique conventionnelle et celle avec l’aide de l’IRM. Résultats: il n’y a pas eu de complications postopératoires. Il n’y a pas de différence dans les pertes sanguines. Il y a une diminution moyenne du temps opératoire de 14% quand on la compare à la technique conventionnelle. La déviation axiale moyenne est de 1,2° en varus ce qui est comparable pour la technique conventionnelle ou la technique assistée par ordinateur. Conclusion: l’utilisation d’un matériel ancillaire conventionnel dans la prothèse totale du genou est une technique suffisamment sure pour le traitement des arthroses du genou sans complication.
Introduction
Recently, there have been attempts to develop a more natural feeling and anatomical total knee replacement. Advances have been made to better match knee anatomy by changing the size and shape of components; however, alignment has remained standardised to be the same for every patient. Historically, components have been oriented along the mechanical axis. Small changes in component positioning and errors in surgical technique were believed to compromise post-operative performance [5, 9]. Computer-assisted techniques have been developed to place the components closer to the mechanical axis and minimise malalignment. However, even with mechanical axis optimisation, functional results have not been found to be improved when compared to conventional techniques [7, 10, 11]. Once again, these techniques disregard the natural alignment of each individual patient’s knee by insisting on a ‘zero’ degree mechanical axis for optimal alignment. The similar clinical outcome between computer-assisted and conventional techniques, along with the quest to improve patient function, suggests the need to re-evaluate alignment principles.
Recent studies have suggested that the natural alignment of the knee in relation to the mechanical axis can be extremely variable [2–4]. Therefore, functional improvements in total knee replacement might focus on restoring the natural kinematics of the joint rather than aligning to a standardised mechanical axis. The kinematic motion of the knee can be referenced to a single, fixed, flexion-extension axis of the distal femur [1–4]. Kinematic and cadaver studies have suggested that the posterior femoral condyles are cylindrical in shape and the true flexion-extension axis of the distal femur passes through the centre of the condyles [2–4]. It is through this trans-cylindrical axis that knee motion occurs with optimal ligament balance in the pre-arthritic knee. In the past, it has been difficult to locate the pre-arthritic trans-cylindrical axis in an arthritic knee. As a result, components were placed along a standardised mechanical axis and the flexion-extension axis passed through the epicondyles of the distal femur, rather than through the posterior femoral condyles. This trans-epicondylar axis is valgus and externally rotated when compared to the trans-cylindrical axis [2–4] (Fig. 1). Therefore, one possibility for improvement of the functional results of total knee replacement might be to align components closer to the trans-cylindrical axis rather than the mechanical axis. New technology using magnetic resonance imaging (MRI) of the arthritic knee and custom-made cutting guides has been developed to help the surgeon align the femoral and tibial components to the pre-arthritic trans-cylindrical axis.
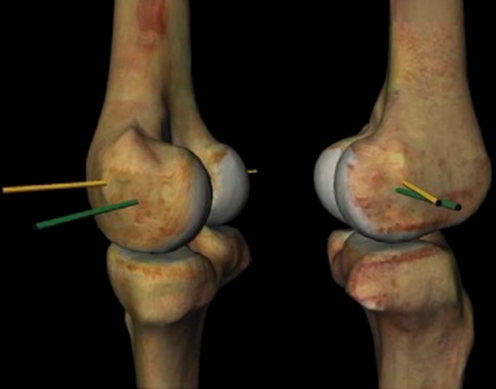
Fig. 1.
Kinematic flexion-extension axis (trans-cylindrical) passes through the centre of the femoral condyles. Trans-cylindrical axis (green) and trans-epicondylar axis (yellow) [2–4]
The purpose of this study was to evaluate the initial intra-operative experience of using custom-made cutting guides to align femoral and tibial components to the trans-cylindrical axis during total knee replacement. While the development of the custom-fit technique is based on multiple studies, to our knowledge, there are no published reports on the intra-operative use of these custom-made cutting guides or on the clinical results of this custom-fit technique. This case-controlled prospective study evaluates intra-operative events and early functional outcomes of total knee replacements using the custom-fit technique in comparison to a cohort of conventional total knee replacements. Long-leg coronal alignment was compared to two previous studies using conventional and computer-assisted techniques.
Methods
Twenty-one consecutive patients (15 women and six men) who had 21 knee replacements using the custom-fit technique between August 2007 and January 2008 were included in this prospective study. All patients had Institutional Review Board approval. The inclusion criterion was met by patients undergoing a primary total knee arthroplasty (TKA) for the diagnosis of primary osteoarthritis. Patients with a history of trauma or previous operations on the knee were excluded.
The mean age of the patients was 64 years (range: 48–80 years). Pre-operative flexion averaged 107° (range: 65–130°) and 47% of patients (10 of 21) had an extension loss with a mean of 6.4° (range: 5–15°). Pre-operative varus/valgus deformities included 58% (14 of 21) with a valgus deformity (5.6°, maximum 10°) and 24% (5 of 21) with a varus deformity (3.6°, maximum of 6°). Two patients had no pre-operative deformity.
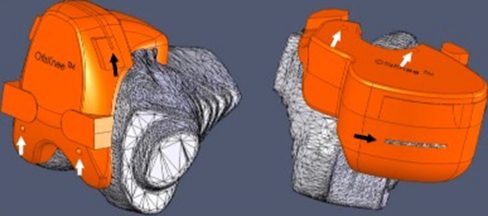
The knee replacements in the study group had components placed with the use of custom-made cutting guides. The cutting guides were created by a single company (OtisMed Inc., Hayward, CA, USA). A sagittal MRI scan of the arthritic knee was obtained at least 14 days before the procedure. A 1.5-T scanner with a dedicated knee coil was used and calibrated as per specific guidelines by the design company. The scan was then uploaded at the manufacturing facility. With the use of software, the sagittal slices were amalgamated into a three-dimensional model of the arthritic knee. Bone and cartilage defects were filled and osteophytes were removed to restore the knee to its natural pre-arthritic alignment. The trans-cylindrical flexion-extension axis of the femur was identified. Femoral and tibial components from the Triathlon system (Stryker, Mahwah, NJ, USA) were shape-matched and aligned to the trans-cylindrical axis. Cutting guides were then machined using biocompatible plastic to fit the arthritic knee (Fig. 2). The femoral and tibial cutting guides referenced all intra-operative cuts to determine the size and the 6 df placement of the femoral and tibial components.
Fig. 2.
Custom-made cutting guides designed to control all intra-operative cuts and align components along the trans-cylindrical axis
In all patients, a tourniquet was inflated to 350 mmHg and a midline incision with a medial parapatellar arthrotomy was used. The custom-made cutting guides were used to make all intra-operative cuts. A cruciate-retaining total knee replacement was cemented in place. Patellae were not resurfaced in any cases. A drain was placed and the arthrotomy and subcutaneous layers were closed in a standard manner.
Component sizes, additional cuts, soft tissue releases and intra-operative complications were recorded to evaluate the intra-operative experience with this new technique.
The custom-fit total knee replacements were compared to a matching cohort of the previous 30 consecutive conventional total knee replacements performed by the same surgeon. In this cohort, each knee replacement was done in a similar fashion as the custom-fit technique except for the intra-operative cuts. In these patients, intra-medullary femoral and extra-medullary tibial referencing guides were used to align the components to the mechanical axis according to conventional techniques.
For both knee groups (custom and conventional), blood loss, tourniquet time and post-operative range of motion were recorded. Blood loss was determined by the difference in pre-operative haematocrit and the haematocrit at 48 hours post-operatively. Tourniquet time was recorded at deflation after dressings were applied. Range of motion was recorded for all patients at three and six months post-operatively with the use of a long-arm goniometer.
Patients with knees implanted using the custom-fit technique were then measured for alignment. Long-leg coronal alignment was determined by a computed tomography scanogram obtained on the second post-operative day. Mechanical axis was defined as a line from the centre of the femoral head to the centre of the talus. The overall alignment of the lower extremity and the alignment of the femoral and tibial components were measured in reference to the mechanical axis. The alignment of the custom-fit knees were recorded and compared to two recently published studies on conventional and computer-assisted total knee replacements using similar data collection.
The arithmetic mean, standard deviation and distribution of values were determined for each measure. Comparisons between the study group and the matching cohort were made with an unpaired Student’s t-test. Differences in long-leg coronal alignment between the study group and two previous studies using conventional and computer-assisted techniques were also determined with an unpaired Student’s t-test. All data were evaluated at a level of significance of 0.05.
Results
There were no adverse intra-operative events with the use of the custom-made cutting guides. All components were accurately sized and fitted securely. Distal femoral resection averaged 2 mm less and tibial resection averaged 2 mm more than the conventional technique. One tibia had to be recut to remove an additional 2 mm of bone to make room for the liner. The thickness of the tibial liner was 9 mm in nine patients and 11 mm in 12 patients. Marginal osteophytes were removed which indirectly lengthened tight ligaments. No additional soft tissue balancing was required. There were no discrepancies in flexion and extension gaps and all knee replacements felt stable through a full range of motion. There were no haematomas, infections, manipulations or reoperations.
In comparison to the cohort of conventional total knee replacements, the drop in haematocrit at 48 hours was similar between the custom-fit group (8.9 ± 2.8%) and the conventional group (8.6 ± 3.1%). Tourniquet time was lower for the custom-fit group (80 ± 17 min) when compared to the conventional group (93 ± 12 min). Post-operative flexion was greater for the custom-fit group when compared to the conventional group at three months (120 ± 13° versus 113 ± 13°) and at six months (130 ± 8° versus 122 ± 13°); however, this was not statistically significant, p ≥ 0.05.
Alignment was measured as deviation from the mechanical axis. Mean coronal alignment of the custom-fit technique (this study) was 1.2° varus ± 2.4° (range: 6° valgus to 4° varus). Mean deviation of the femoral component from the mechanical axis was 1.6° valgus ± 1.8° and mean deviation of the tibial component was 2.9° varus ± 2.1°. Comparisons with mean coronal alignment in two previous studies on conventional and computer-assisted techniques are outlined in Tables 1 and 2 with the custom group having similar alignment values. If one assumes a tolerance level of 3°, two patients in the custom-fit group were outside this tolerance.
Table 1.
Comparison of this study with two previous studies
| Study | Deviation from mechanical axis |
|---|---|
| Custom-fit TKA (this study, N = 21) | 1.2° varus ± 2.4° (range: 6° valgus to 4° varus) |
| Conventional TKA (Matziolis et al. [4], N = 28) | 2.6° varus ± 1.7° (range: 5° valgus to 7° varus) |
| Computer-assisted TKA (Matziolis et al. [4], N = 32) | 1.4° varus ± 0.8° (range: 3° valgus to 3° varus) |
| Conventional TKA (Stulberg et al. [5], N = 40) | 0.4° varus ± 3.3° (range: 6° valgus to 8° varus) |
| Computer-assisted TKA (Stulberg et al. [5], N = 38) | 1.9° varus ± 2.9° (range: 4° valgus to 8° varus) |
Table 2.
Comparison of this study with a previous study
| Study | Deviation of femoral component from mechanical axis | Deviation of tibial component from mechanical axis |
|---|---|---|
| Custom-fit TKA (this study, N = 21) | 1.6° valgus ± 1.8° (range: 4° valgus to 2° varus) | 2.9° varus ± 2.1° (range: 6° valgus to 4° varus) |
| Conventional TKA (Matziolis et al. [4], N = 28) | 2.2° varus ± 3.2° (range: 2° valgus to 5° varus) | 2.0° varus ± 1.7° (range: 4° valgus to 6° varus) |
| Computer-assisted TKA (Matziolis et al. [4], N = 32) | 1.0° varus ± 0.6° (range: 2° valgus to 3° varus) | 1.4° varus ± 0.89° (range: 3° valgus to 3° varus) |
Discussion
The purpose of this study was to evaluate our initial experience with a custom-fit total knee replacement that aims to recreate the natural trans-cylindrical axis. Although conventional knee replacements restore a significant degree of function, improvements might be needed to restore motion closer to normal for more active patients that continue to perform physically demanding activities. Changing the shape of the components or placing the components closer to the mechanical axis may not always lead to improved functional results [7, 10, 11]. Recent studies have suggested that aligning the components to the anatomical flexion-extension axis of the distal femur instead of the mechanical axis may help improve functional results [1–4]. New technology allows the surgeon to place components along the flexion-extension axis by controlling all intra-operative cuts. However, to date there are no published results on the intra-operative experience or functional outcome using this technique, which prompted this study.
One important finding was that the new custom-fit technique for implanting a total knee replacement did not lead to any adverse events. All guides fitted securely to the arthritic knee even though there was little room for error. All components were accurately sized and fitted precisely with the intra-operative cuts. We did notice that there was slightly less femoral resection and slightly more tibial resection when compared to the conventional technique. The purpose of these cuts was to allow for restoration of the joint line so that the femoral component can be aligned to the natural flexion-extension axis. All polyethylene inserts were either a size 9 or 11 indicating that conservative bone cuts were able to be achieved.
There was no need for soft tissue balancing in any of the custom-fit knees. It is believed that, by removing osteophytes and aligning the components to the anatomical axis, ligament balance was restored. All knees were felt to be stable through a full range of motion and there was no lift-off of the tibial tray when actively testing the component. It is important to note that the patient population in this study did not have any severe pre-operative deformities (range: 10° valgus to 6° varus).
Most new techniques in joint replacement require increased operative time; however, the procedure time for this technique decreased. Although there was only a mean difference in tourniquet time of 13 minutes, this included a short learning curve for the custom-fit technique. The final two procedures in the study had a tourniquet time of 48 and 54 minutes compared to the surgeon’s mean tourniquet time of 93 min for the conventional technique. There was also a decrease in operative set-up time. Because the size of the components was already known, there was a reduction in cleaning and processing of instruments between cases. This could reduce turnover time; however, these data were not studied.
The custom-fit technique is designed to align components to the natural flexion-extension axis of the knee instead of the mechanical axis. By ignoring the mechanical axis there may be concern about post-operative coronal alignment and long-term wear rates with the custom-fit technique. The principle of placing components along the mechanical axis to reduce wear is based on a single publication based on components placed from 1976 to 1981 [5]. This study (N = 139) showed an increased rate in component loosening with knees placed outside of 3° of the mechanical axis at the eight-year follow-up. A more recent study (N = 395) showed no correlation between wear rates and alignment to the mechanical axis at 15 years [8]. They suggested that wear rates might be more determined by other factors, such as balancing and restoration of normal kinematics. Although aligning components to the mechanical axis is not a goal of the custom-fit knee, the knees averaged 1.2° varus which is closer to the mechanical axis than many previously reported results using conventional and computer-assisted techniques [7, 11]. The custom-fit technique also had fewer outliers if a 3° tolerance is accepted.
It is important to note a recent case series of four patients which suggested that the custom-fit technique resulted in malalignment [6]. Component positioning, as measured by computer navigation and referenced to the mechanical axis, ranged from 5° valgus to 7.5° varus. This was not the experience found in our study.
There were several limitations in this study or in using this technique. First, patients with previous operations or trauma were excluded and no patient had a varus/valgus deformity of greater than 10°. Adding these patients might have increased the complication rate or alignment errors of this technique. Finally, coronal alignments were not compared to the senior surgeon’s own conventional technique, but rather a cohort of patients from recent publications. However, the purpose of the coronal alignment was not to measure how close the custom-fit knee was to the mechanical axis in comparison to other techniques, but rather to determine if the custom-fit technique would cause a gross deviation from the mechanical axis, which would certainly be a cause for concern. This was not found.
In summary, this study was designed to evaluate our initial experience with the custom-fit technique for total knee replacements. There were no significant intra-operative complications. All guides fitted properly and components were accurately sized. The post-operative coronal alignment was close to the mechanical axis, which allays concerns about early wear rates. The custom-fit total knee replacement is designed to recreate the natural pre-arthritic alignment of the patient’s knee with the goal of increasing function. This report did not determine long-term functional outcome; however, it does suggest that the custom-fit technique is a safe procedure for uncomplicated cases of osteoarthritis. This technique should continue to be studied as an alternative to conventional and computer-assisted techniques with the goal of increasing function in total knee replacement.
References
- 1.Coughlin KM, Incavo SJ, Churchill DL, Beynnon BD. Tibial axis and patellar position relative to the femoral epicondylar axis during squatting. J Arthroplasty. 2003;18(8):1048–1055. doi: 10.1016/S0883-5403(03)00449-2. [DOI] [PubMed] [Google Scholar]
- 2.Eckhoff DG, Bach JM, Spitzer VM, et al. Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am. 2005;87(Suppl 2):71–80. doi: 10.2106/JBJS.E.00440. [DOI] [PubMed] [Google Scholar]
- 3.Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, et al. Three-dimensional morphology and kinematics of the distal part of the femur viewed in virtual reality. J Bone Joint Surg Am. 2003;85(Suppl 4):97–104. doi: 10.2106/00004623-200300004-00012. [DOI] [PubMed] [Google Scholar]
- 4.Eckhoff DG, Dwyer TF, Bach JM, Spitzer VM, et al. Three-dimensional morphology of the distal part of the femur viewed in virtual reality. J Bone Joint Surg Am. 2001;83(Suppl 2):43–50. doi: 10.2106/00004623-200100021-00010. [DOI] [PubMed] [Google Scholar]
- 5.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73(5):709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 6.Klatt BA, Goyal N, Austin MS, Hozack WJ. Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. J Arthroplasty. 2008;23(1):26–29. doi: 10.1016/j.arth.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 7.Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, ramdomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007;89(2):236–243. doi: 10.2106/JBJS.F.00386. [DOI] [PubMed] [Google Scholar]
- 8.Parratte S, Trousdale R, Berry DJ, Pagnano MW (2008) Reproducing the mechanical axis did not improve the 15-year survival of 398 modern TKA. Scientific presentation, AAOS Annual Meeting, San Francisco, CA
- 9.Piazza SJ, Delp SL, Stulberg SD, Stern SH. Posterior tilting of the tibial component decreases femoral rollback in posterior-substituting knee replacement: a computer simulation study. J Orthop Res. 1998;16(2):264–270. doi: 10.1002/jor.1100160214. [DOI] [PubMed] [Google Scholar]
- 10.Spencer JM, Chauhan SK, Sloan K, Taylor A, Beaver RJ. Computer navigation versus conventional total knee replacement: no difference in functional results at two years. J Bone Joint Surg Br. 2007;89(4):477–480. doi: 10.1302/0301-620X.89B4.18094. [DOI] [PubMed] [Google Scholar]
- 11.Stulberg SD, Yaffe MA, Koo SS. Computer-assisted surgery versus manual total knee arthroplasty: a case-controlled study. J Bone Joint Surg Am. 2006;88(Suppl 4):47–54. doi: 10.2106/JBJS.F.00698. [DOI] [PubMed] [Google Scholar]