Abstract
This study compares MRI with examination under anaesthesia to surgical findings in evaluating soft tissue injuries in acute multi-ligament knee trauma. Pre-operative MRI was done for 44 patients who underwent surgery for grade III ACL and grade III medial collateral ligament (MCL) injury. In 21 cases both ACL and MCL were treated surgically, but in 23 only ACL. Intra-operative and MRI findings were compared. Accuracy of MRI for medial meniscal tears was 88.6%, sensitivity 80%, and specificity 91.2%; accuracy for lateral meniscal tears was 72.7%, sensitivity 55% and specificity 87.5%. Accuracy and sensitivity for severity of ACL tear was 93.2% and of MCL tear 86.4%. In 88.6% of the knees, bone bruises were visible, with anterolateral femoral and posterolateral tibial bone bruise being the most common. MRI revealed no chondral lesion, but arthroscopy revealed 11. In combined ACL–MCL ruptures, the incidence of concomitant injuries is high and the injuries are best detected with MRI.
Résumé
Cette étude a pour but de comparer les données de l’IRM avec les résultats de l’examen sous anesthésie et les constatations chirurgicales après traumatismes aigus du genou. Une IRM préopératoire a été réalisée chez 44 patients qui ont bénéficié d’un geste chirurgical pour des lésions de grade III du ligament croisé antérieur et de grade III du ligament médio collatéral. Dans 21 cas, le ligament croisé antérieur et le ligament latéral interne ont été réparés chirurgicalement mais dans 23 cas les patients ont bénéficié simplement d’une réparation du ligament croisé antérieur. Les constatations per opératoires et les constations IRM ont été comparées. Pour l’IRM le diagnostic est fait à 88,6% pour les lésions méniscales avec une sensibilité de 80% et une spécificité de 91,2%. En ce qui concerne les lésions du ménisque externe latéral, les constatations IRM sont de 72,7% avec une sensibilité de 55% et une spécificité de 87,5%. Pour les ligaments croisés antérieurs, la sensibilité est de 93,2% et pour le ligament latéral interne de 86,4%. Les érosions osseuses sont visibles et leurs constatations sur le fémur antéro latéral et sur le tibia postéro latéral sont habituelles. L’IRM n’a révélé aucune lésion cartilagineuse mais l’arthroscopie a montré qu’il y en avait 11. Les ruptures combinées du ligament croisé antérieur et du ligament latéral interne sont d’une association fréquente et peuvent être détectées de façon plus facile par l’IRM.
Introduction
A complete tear of the anterior cruciate ligament (ACL) and medial collateral ligament (MCL) is a severe injury with associated knee pathology [8, 12, 13]. It is usually the result of motor vehicular or sports-related trauma [8]. Clinical examination can raise suspicion of ligamentous injury, but MRI is the noninvasive imaging modality of choice for the evaluation of overall knee pathology [15]. MRI accuracy is comparable to that of diagnostic arthroscopy [6, 7], and MRI also allows assessment of the internal architecture of the knee. It can distinguish partial from complete rupture and evaluate the knee for associated injuries. Indirect signs such as bone bruises and osteochondral fractures can assist in the diagnosis of such a ligamentous injury [15].
In this prospective study we compared MRI and surgical findings in patients with combined injury to their ACL and MCL.
Materials and methods
We evaluated preoperative MRI and arthroscopic findings in 44 patients (25 female and 19 male; mean age 38.6, range 21–64) who had total acute ACL and MCL injury on a clinical basis. Every patient underwent MRI before the operation.
MRI was performed with either a 1.5T scanner (Sigma LX 1.5T, GE Medical Systems, Milwaukee, WI) or a 0.23T open scanner (Outlook GP, Picker Nordstar, Helsinki, Finland), with routine clinical sequences and dedicated knee coils. For 0.23T (N 33), the routine protocol included coronal STIR (TR 1000 ms, TE 16 ms, TI 90 ms) and T1 SE (TR 380 ms, TE 25 ms) images, axial T2 FSE (TR 1900 ms, TE ef 80 ms) images, and sagittal DE (TR 2400, TE 22/80) images, completed with oblique coronal T2 SE (TR 1600 ms, TE 81 ms) images when necessary. Typically, 1.5T (N 11) MR scans included coronal T2 FSE fat-saturated (TR 4740 ms, TE ef 40 ms) images, axial PD FSE fat-saturated (TR 2640 ms, TE ef 26 ms) images, and sagittal images typically obtained with a DE (TR 2340 ms, TE 20/90 ms) sequence, or a PD SE (TR 1800–2700 ms, TE 20 ms) sequence. Oblique coronal T2 FSE (TR 3500–5200 ms, TE ef 96 ms) images were obtained when necessary.
The MRI scans were reviewed by staff radiologists and an independent emergency radiologist. Findings recorded were those of ligamentous structures, meniscal tears, cartilage damage, bone marrow abnormalities, and bone lesions.
All diagnostic arthroscopies were performed within three weeks after the initial trauma with intraoperative findings noted, and then surgical procedures followed. Twenty-one patients had open operative management of the MCL, with the focus on the localisation and severity of the MCL rupture. These findings were then compared with those predicted by the preoperative MRIs.
For the statistical analysis, interobserver agreement correlations were calculated with the Kappa-test.
The study was conducted in conformity with the principles of the Declaration of Helsinki and approved by our institutional committee of ethics. The subjects gave informed consent to participate in the study.
Results
Menisci
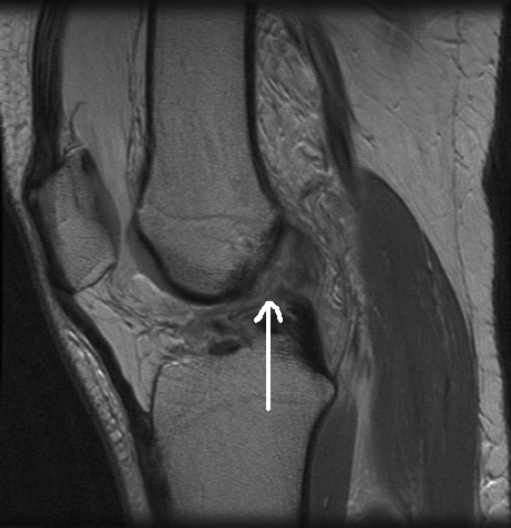
MRI revealed 11 medial and 14 lateral meniscal tears; arthroscopy revealed a respective 10 and 20 providing an accuracy of MRI for medial meniscal tears of 88.6%, a sensitivity of 80% (0.23 T 71.8% and 1.5 T 100%), and a specificity of 91.2% (0.23 T 88.5% and 1.5 T 100%). For lateral meniscal tears, accuracy was 72.7%, sensitivity 55% (0.23 T 64.3% and 1.5 T 33.3%), and specificity 87.5% (0.23 T 88.5% and 1.5T 100%) (Table 1). Medial meniscal tears (Fig. 1) were detected with acceptable interobserver agreement (Kappa = 0.88), but agreement was lower for lateral meniscal tears (Kappa = 0.56).
Table 1.
Percentage validity of the medial and lateral meniscal, ACL, and MCL diagnoses in MRI
| Validity | Medial meniscus | Lateral meniscus | ACL | MCL |
|---|---|---|---|---|
| Accuracy | 88.6 (39/44) | 72.7 (32/44) | 93.2 (41/44) | 86.4 (38/44) |
| Sensitivity | 80.0 (8/10) | 55.0 (11/20) | 93.2 (41/44) | 86.4 (38/44) |
| Specificity | 91.2 (31/34) | 87.5 (21/24) | * | * |
| Negative predictive value | 93.9 (31/33) | 70.0 (21/30) | * | * |
| Positive predictive value | 72.7 (8/11) | 78.6 (11/14) | * | * |
ACL anterior cruciate ligament, MCL medial collateral ligament, MRI magnetic resonance imaging
*Could not be calculated; no true negatives
Fig. 1.
Medial meniscal posterior horn tear in MRI
Anterior cruciate ligament
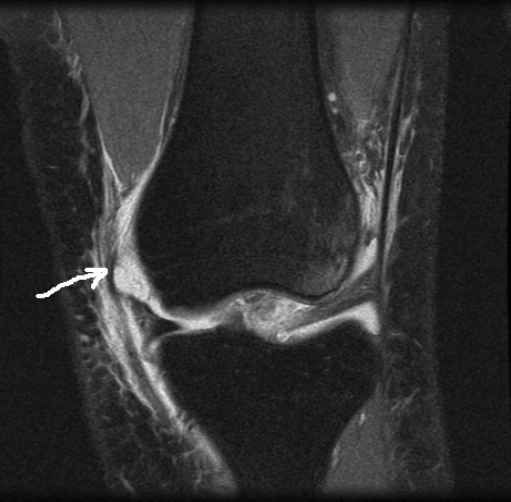
MRI revealed three grade II and 41 grade III tears; on a clinical and surgical basis, all these tears were complete grade III tears. Thus, sensitivity and accuracy were 93.2%. In MRI, 28 tears were proximal, two proximal and midsubstance, 12 midsubstance, one distal, and one proximal and distal. In arthroscopy, 40 tears were proximal and four in the midsubstance (Fig. 2).
Fig. 2.
Complete ACL rupture in MRI
Medial collateral ligament
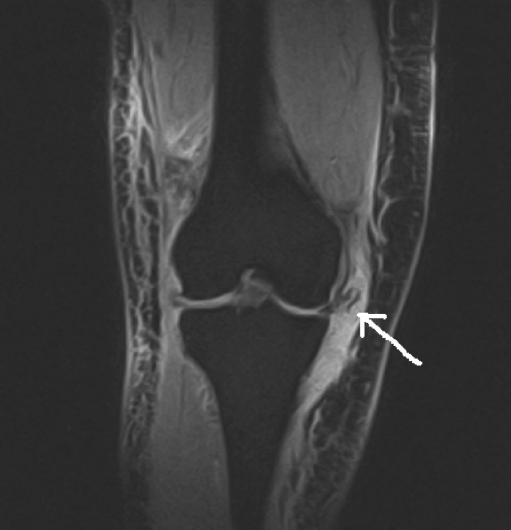
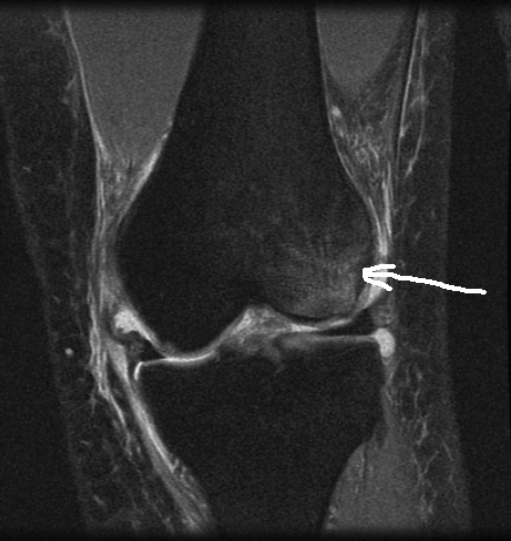
In the surgically treated MCL group, MRI revealed three grade II and 18 grade III tears. Clinically and surgically all 21 were grade III. Sensitivity and accuracy were 86.4%. In MRI, 28 tears were proximal, eight distal, two proximal and distal, two proximal and midsubstance, one midsubstance and distal, and three midsubstance only. In 21 cases MCL had been operated on, and in this group of MRIs, the MCL tear location was exactly the same as during surgery in 11 cases (52.4%); nine cases included some mismatch (42.9%); and one case showed a distal tear which at surgery appeared proximal (Table 2, Figs. 3 and 4).
Table 2.
Grade and location of surgically treated medial collateral ligament rupture (N = 21)
| Patient | Surgical findings | MRI findings | ||||||
|---|---|---|---|---|---|---|---|---|
| Grade | Proximal | Medial | Distal | Grade | Proximal | Medial | Distal | |
| 1 | 3 | x | 2 | x | ||||
| 2 | 3 | x | x | 3 | x | |||
| 3 | 3 | x | 3 | x | ||||
| 4 | 3 | x | 3 | x | x | |||
| 5 | 3 | x | 3 | x | ||||
| 6 | 3 | x | 3 | x | ||||
| 7 | 3 | x | 3 | x | ||||
| 8 | 3 | x | 3 | x | ||||
| 9 | 3 | x | 3 | x | ||||
| 10 | 3 | x | x | 3 | x | x | ||
| 11 | 3 | x | 3 | x | ||||
| 12 | 3 | x | 3 | x | ||||
| 13 | 3 | x | 3 | x | ||||
| 14 | 3 | x | 3 | x | ||||
| 15 | 3 | x | 3 | x | ||||
| 16 | 3 | x | x | 3 | x | |||
| 17 | 3 | x | x | 3 | x | |||
| 18 | 3 | x | 2 | x | ||||
| 19 | 3 | x | 2 | x | ||||
| 20 | 3 | x | 3 | x | ||||
| 21 | 3 | x | 3 | x | ||||
Fig. 3.
Proximal MCL tear in MRI
Fig. 4.
Distal MCL tear in MRI
Lateral collateral ligament
No clinically lateral instabilities were observable in any case, but MRI revealed three grade III, two grade II, and 12 grade I LCL injuries.
Bone bruises
Bone bruises were visible in MRI for 88.6% of the knees, with only five patients free of these. Anterolateral femoral and posterolateral tibial bone bruises were most common (N 25, 56.8%); posterolateral tibial bone bruises numbered eight (18.2%), anterolateral femoral 3 (6.8%), and a combination of anterolateral femoral, postreolateral tibial, and posteromedial tibial bone bruises numbered three (6.8%) (Fig. 5).
Fig. 5.
Lateral femoral bone bruise in MRI
Fractures and chondral lesions
MRI revealed ten fractures: five tibial lateral fractures, two proximal fibular fractures, two MCL avulsion fractures, and one posteromedial tibial impression fracture. MRI revealed no chondral lesions, but 11 appeared in arthroscopy. Six Segond’s fractures were visible in conventional radiograpy but only two in MRI.
Discussion
In combined ACL–MCL ruptures concurrent injuries are common and the injuries are best detected with MRI. In this study, the ability of MRI to detect medial meniscal, ACL and MCL tears, and bone bruises was good, but sensitivity to lateral meniscal tears was only 55%. Nor were any of the 11 chondral lesions seen in arthroscopy detected. For ACL, MCL, and medial meniscal tears, imaging at 1.5 T field strength outperformed 0.23 T techniques. Despite lower image detail and more limited sequences, for those claustrophobic patients who cannot undergo conventional closed-bore MRI, scanning with an open MR unit proved a viable option.
In an acute ACL tear of the valgus, the rotational force compressing the lateral compartment makes lateral meniscal tears more common [4, 10, 14]. The injury triad of ACL–MCL–lateral meniscus appeared twice as often as the ACL–MCL–medial meniscus combination. In alpine ski injuries, the ACL–MCL–lateral meniscus combination may be nine times more common [4]. In this study, 45.5% patients had lateral and 22.7% medial meniscal tears. Medial meniscal tears are more common with chronic instability, however, because of the secondary restraining effect of the medial meniscus to anterior tibial translation [1, 9].
For medial meniscal tears, sensitivities have ranged from 86% to 96% and specificities from 75% to 94%; respectively, values for lateral meniscal tears have been 64–89% and 87–98% [2, 6, 16].
Detection of a meniscal tear in the setting of an acute ligamentous injury is more difficult than of an isolated tear. We had sensitivity for medial meniscal tears of 80%. In the literature the sensitivity for medial meniscal tears decreases to 84–88%, while the sensitivity of diagnosing lateral meniscal tears decreases to 68–83% in the setting of a concurrent ACL injury [2, 16]. Our sensitivity of 55% for lateral meniscal tears was lower than that reported in the literature. For tears of the lateral meniscus, false-negative diagnoses outnumbered false-positives three to one (9 vs. 3). High false-negative rates in lateral meniscal tears have also been reported previously [6, 11]. Considerable interobserver variation also occurred in detection of lateral meniscal tears (Kappa = 0.56). Due to the more complex anatomy of the lateral meniscus, these tears are difficult to detect and thus require excellent tissue contrast and better spatial resolution of the MRI.
De Smet and Graf reported that many of the false-negative findings involved subtle tears of the peripheral posterior horn, and these were particularly common in the lateral meniscus and were associated with tears of the ACL [2]; 40% of the interpretation errors have been unavoidable even in retrospective readings [3].
Causes of false MRI interpretations are many, including technical and anatomy-related causes. Some errors in the MRI interpretation may be related to problems in the use of arthroscopic findings as the standard of reference, including lack of imaging of some tears under the surface of the posterior horn, reliance on probing or compression to diagnose tears, and differences in descriptive terminology for disease of or damage to the meniscus [11]. One arthroscopist may describe meniscal free edge pathology as fraying and another as a small tear.
ACL tears are associated with at least one bone bruise in 71% of patients, and most commonly involve the midportion of the lateral femoral condyle near the terminal sulcus and the posterior lateral tibial plateau [5]. Our incidence of bone bruises was even higher (88.6%).
None of the chondral lesions we diagnosed at surgery was visible in MRI. MRI’s low sensitivity for chondral lesions has been reported before [17]. Our study form included no formal classification of chondral lesions, so we do not know the true nature of the chondral lesions we have missed. These may also have included partial-thickness chondral lesions of varying sizes.
Medial collateral tears are not always in one plane, and components of tears exist at different levels of the ligament. Classification of tear location was not always easy. For example, “MCL tear was oblique and total going proximally and backwards. Also the posterior capsule was torn.” This was classified by the surgeon as proximal and by the radiologist as distal. We suppose that both were only partly right in this case; the anterior part of the tear may have been distal.
Conclusion
In multi-ligament injury, MRI ability to detect lateral meniscal tears was less than hoped, but medial meniscal tears, ligamentous injuries, and bone bruises were seen more precisely. In combined ACL–MCL ruptures the incidence of concomitant injuries is high and the injuries are best detected with MRI.
References
- 1.Dandy DJ. The arthroscopic anatomy of symptomatic meniscal lesions. J Bone Joint Surg Br. 1990;72(4):628–633. doi: 10.1302/0301-620X.72B4.2380218. [DOI] [PubMed] [Google Scholar]
- 2.Smet AA, Graf BK. Meniscal tears missed on MR imaging: relationship to meniscal tear patterns and anterior cruciate ligament tears. AJR Am J Roentgenol. 1994;162(4):905–911. doi: 10.2214/ajr.162.4.8141016. [DOI] [PubMed] [Google Scholar]
- 3.De Smet AA, Tuite MJ, Norris MA, Swan JS, et al. MR diagnosis of meniscal tears: analysis of causes of errors. AJR Am J Roentgenol. 1994;163:1419–1423. doi: 10.2214/ajr.163.6.7992739. [DOI] [PubMed] [Google Scholar]
- 4.Duncan JB, Hunter R, Purnell M, et al. Meniscal injuries associated with acute anterior cruciate ligament tears in alpine skiers. Am J Sports Med. 1995;23(2):170–172. doi: 10.1177/036354659502300208. [DOI] [PubMed] [Google Scholar]
- 5.Graf BK, Cook DA, Smet AA, et al. ‘Bone bruises’ on magnetic resonance imaging evaluation of anterior cruciate ligament injuries. Am J Sports Med. 1993;21(2):220–223. doi: 10.1177/036354659302100210. [DOI] [PubMed] [Google Scholar]
- 6.Fischer SP, Fox JM, Pizzo W, et al. Accuracy of diagnoses from magnetic resonance imaging of the knee: a multi-center analysis of one thousand and fourteen patients. J Bone Joint Surg Am. 1991;73(1):2–10. [PubMed] [Google Scholar]
- 7.Ha TP, Li KC, Beaulieu CF, et al. Anterior cruciate ligament injury: fast spin-echo MR imaging with arthroscopic correlation in 217 examinations. Am J Roentgenol. 1998;170:1215–1219. doi: 10.2214/ajr.170.5.9574587. [DOI] [PubMed] [Google Scholar]
- 8.Halinen J, Lindahl J, Hirvensalo E, Santavirta S. Operative versus nonoperative treatment of medial collateral rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med. 2006;34(7):1134–1140. doi: 10.1177/0363546505284889. [DOI] [PubMed] [Google Scholar]
- 9.Indelicato PA, Bittar ES. A perspective of lesions associated with ACL insufficiency of the knee: a review of 100 cases. Clin Orthop. 1985;198:77–80. [PubMed] [Google Scholar]
- 10.Joseph C, Pathak SS, Aravinda M, Rajan D. Is ACL reconstruction only for athletes? A study of the incidence of meniscal and cartilage injuries in an ACL-deficient athlete and non-athlete population – an Indian experience. Int Orthop (SICOT) 2008;32:57–61. doi: 10.1007/s00264-006-0273-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Justice WW, Quinn SF. Error patterns in the MR imaging evaluation of menisci of the knee. Radiology. 1995;196:617–621. doi: 10.1148/radiology.196.3.7644620. [DOI] [PubMed] [Google Scholar]
- 12.Nakamura N, Horibe S, Toritsuka Y, Mitsuoka T, Yoshikawa H, Shino K. Acute grade III medial collateral ligament injury of the knee associated with anterior cruciate ligament tear: the usefulness of magnetic resonance imaging in determining a treatment regimen. Am J Sports Med. 2003;31:261–267. doi: 10.1177/03635465030310021801. [DOI] [PubMed] [Google Scholar]
- 13.Noyes FR, Barber-Westin SD. The treatment of acute combined ruptures of the anterior cruciate and medial collateral ligament of the knee. Am J Sports Med. 1995;23:380–389. doi: 10.1177/036354659502300402. [DOI] [PubMed] [Google Scholar]
- 14.Paletta GA, Levine DS, O’Brien SJ, et al. Patterns of meniscal injury associated with acute anterior cruciate ligament injury in skiers. Am J Sports Med. 1992;20(5):542–547. doi: 10.1177/036354659202000510. [DOI] [PubMed] [Google Scholar]
- 15.Prickett WD, Ward SI, Matava MJ. Magnetic resonance imaging of the knee. Sports Med. 2001;31(14):997–1019. doi: 10.2165/00007256-200131140-00004. [DOI] [PubMed] [Google Scholar]
- 16.Rubin DA, Kettering JM, Towers JD, et al. MR imaging of knees having isolated and combined ligament injuries. AJR Am J Roentgenol. 1998;170(5):1207–1213. doi: 10.2214/ajr.170.5.9574586. [DOI] [PubMed] [Google Scholar]
- 17.Yoon Y-S, Rah J-H, Park H-J. A prospective study of the accuracy of clinical examination evaluated by arthroscopy of the knee. Int Orthop (SICOT) 1997;21:223–227. doi: 10.1007/s002640050155. [DOI] [PMC free article] [PubMed] [Google Scholar]