Abstract
A retrospective study was undertaken to evaluate the clinical and radiographic outcomes of 74 cementless total hip arthroplasties (THA) in 69 young Chinese patients. The Asian size and MMA AML stems with smoothly tapered tip were used, and the patients were followed up for at least five years. The mean Harris hip score was 45.4 preoperatively and 95.3 at the last follow-up. The incidence of thigh pain was 5.4%, and was related to the short stature of the patient (<160 cm) (P = 0.030). Six patients (6 hips, 8.1%) had acetabular osteolysis in zone 2; reoperation was performed in one patient because of osteolysis and wear of the polyethylene liner. The survival rate of the metal acetabular and femoral components was 100% (95% confidence interval, 0.95–1.0). Primary THA with this AML prosthesis had an acceptable mid-term result in young Chinese patients.
Résumé
Cette étude rétrospective a pour but d’évaluer sur le plan clinique et radiographique le devenir de 74 prothèses de hanche sans ciment posées chez 69 jeunes patients d’origine chinoise. une taille de type asiatique et une pièce fémorale de type MMA AML avec un revêtement de surface discret a été utilisé chez nos patients. Ces patients ont été suivis durant au moins 5 ans. Le score moyen de Harris était de 45,4 en préopératoire et de 95,3 au dernier suivi. Le taux de douleur de cuisse était de 5,4% et ce taux était en rapport avec la petite taille des patients (< à 1m60 p = 0,030). 6 patients (6 hanches, 8,1%) présentaient une ostéolyse acétabulaire en zone 2, une réintervention a été nécessaire chez un patient du fait de cette ostéolyse et d’une usure de l’insert polyéthylène. Le taux de survie du composant de la pièce fémorale et du composant métallique acétabulaire est de 100% (95% intervalle de confiance, 0,95–1,0). les prothèses totales de hanche primaire de type AML ont une bonne tolérance à moyen terme chez les jeunes patients d’origine chinoise.
Introduction
The anatomic medullary locking (AML) prosthesis has an extensively porous-coated surface which allows bone ingrowth over the entire length of the prosthesis. To date, many studies with standard AML cementless total hip arthroplasty (THA) have reported promising results [2, 5, 6, 11, 14, 20, 21, 23]. In our patients, we used the Asian size and MMA (modified medial aspect) AML stems, with a smoothly tapered tip. This stem with such a tip has not been previously mentioned in the literature.
The goal of this prospective study was to assess clinical and radiographic results of cementless THA with AML stems and to determine advantages and limitations of these stems.
Materials and methods
Between July 2000 and June 2002, the senior author (FuXing Pei) performed 91 consecutive primary THA on 80 patients with various disabling hip diseases (Table 1).
Table 1.
Demographic data
| Diagnosis | Hips (%) |
|---|---|
| Osteonecrosis of the femoral head | 51 (56%) |
| Arthritis secondary to dysplasia of the hip | 17 (18.7%) |
| Primary arthritis of the hip | 13 (14.3%) |
| Ankylosing spondylitis | 6 (6.6%) |
| Rheumatoid arthritis | 1 (1.1%) |
| Arthritis secondary to hip pyogenic arthritis in childhood | 1 (1.1%) |
No patients died before the latest follow-up. Eleven patients (17 hips) failed to complete the follow-up and were excluded from the analysis. The remaining 69 patients (74 hips) were followed up from five to seven years with a mean of 6.1 years. There were 46 men and 23 women with a mean age of 47 years (range, 18–72 years). The mean height of the patients was 165 cm (range, 154–180 cm), and the mean weight was 63 kg (range, 44–95 kg).
The Asian size and MMA AML stem has a proportionally smaller diameter and length than the standard one. It is an extensively (5/8) porous-coated stem with a mean pore size of 250 µm (DePuy, Warsaw, Indiana, USA). The components contain CoCr substrates with sintered CoCr beads. The tip of the stem is smoothly tapered, to help reduce the potential for thigh pain. The stem sizes averaged 12.8 mm (range, 10.5–16.5 mm).
The acetabular components were tri-spike Duraloc 300 (DePuy, Warsaw, Indiana, USA). This is a hemispherical, porous-coated, titanium acetabular component without a screw hole. A ring-locking mechanism secured the polyethylene liner. In this study, the shell sizes averaged 54 mm (range, 48–62 mm) with a corresponding polyethylene liner thickness averaging 9.7 mm (6.5–13.5 mm). A polyethylene liner with a 10° elevated rim was used in all the hips.
A 28-mm modular chromium-cobalt femoral head was used in all the patients.
All hips were approached posterolaterally without trochanteric osteotomy. The acetabulum was prepared with hemispherical reamers to achieve bleeding cancellous bone. Underreaming of the acetabulum by 2 mm was performed in all acetabular components. The cancellous autograft (resected femoral head) was used to fill any acetabular cyst. The components were inserted by press-fit, as determined by the preoperative use of the templates.
All the patients received prophylactic antibiotics, namely one dose (1.5 g) of intravenous cefuroxime half an hour before the operation, a second dose (1.5 g) during the operation, and a third dose (1.5 g) 12 hours after the operation.
Physical therapy was begun on the first postoperative day to encourage rehabilitation. All the patients were fully weight-bearing at 12 weeks.
The clinical and radiographic follow-ups were performed at two days, and then one, three, six, and 12 months after operation, and yearly thereafter. The Harris hip scores were determined preoperatively and at each follow-up examination. The patients were asked to evaluate the thigh pain subjectively. The clinical result was considered excellent if the score was 90 points or above, good if between 80 and 89, fair if between 70 and 79, and poor if below 70. Any complications and reoperations related to the THA were recorded. The survival statistics were calculated, taking radiographic loosening and revision for any reason as an end point.
The ratio of the width of the femoral component to the width of the femoral canal was calculated according to the method described by Teloken et al. [26]. The position of the acetabular component was assessed at the same time.
The final follow-up radiographs were scrutinised for radiolucent lines around the acetabular component and the femoral component [4, 8]. The stability of the femoral component was assessed [7]. Any vertical subsidence was determined according to the method described by Phillips et al. [22].
Anteversion and abduction angle of the acetabular component were measured according to the method described by Kim [13].
The proximal femoral remodelling was graded according to the method described by Engh et al. [7]. The so-called pedestal formation was recorded if the endosteal condensation of the new bone formation was observed at the tip [7]. All these signs were evaluated with the zonal distribution by Gruen et al. [8]. Heterotopic ossification was graded according to the classification by Brooker et al. [3]. Osteolysis was considered to be present if a progressive radiolucent cavity was identified in the periprosthetic bone. The length and the width of osteolytic lesions were measured on radiographs. The linear wear of the liners was measured by a software program (Canvas X software, ACD Systems, Miami, Florida, USA) according to the method of Martell et al. [19]. The volumetric wear was calculated with the equation V = πr2w, where V is the volumetric wear, r, the radius of the femoral head, and w, the measured linear wear [15].
All the radiographs were reviewed by one independent observer (XYQ) who had not been involved in the patients’ surgery. All the measurements were calibrated for magnification with the implanted femoral head diameter as a reference. The radiographs were digitised by a Lumiscan 200 laser digitiser (Lumisys Inc., Sunnyvale, California, USA) to create TIFF digital images with a pixel size of 0.17×0.17 mm. Measurements of the acetabular component and stem migrations were made between the consecutive images. No additional enhancements were made to the images.
Statistical analysis was performed by the use of the χ2 tests with the Yates correction, the Student 2-tailed t tests, and analysis of the variance. The Kaplan-Meier curve method was used for analysis of the failure-free rate. In addition, the Greenwood formula was used to calculate the confidence interval of the failure-free rate at a certain time point.
Results
The results at last follow-up were 71 hips (96%) excellent, three hips (4%) good, and no fair or poor. The mean Harris hip score was increased from 45.4 points preoperatively (range, 0–86 points) to 95.3 points (range, 84–100 points) at last follow-up.
No patient used any support. Sixty-two patients (89.9%) had no detectable limp, six patients (8.7%) had mild limp, and one (1.4%) had moderate limp. All patients markedly improved their ability to use stairs and public transportation and to put on shoes and cut toenails after the operation.
Four patients (4 hips, 5.4%) complained of anterior thigh pain during the first year, usually within three to eight months after surgery. The onset coincided with weight bearing. All four patients were shorter than 160 cm. The pain did not limit function and could be relieved by rest. Analgesics were not used. One year later, only one patient continued to complain of occasional pain along the anterior thigh at the level of the distal end of the stem without any evidence of infection or loosening, and the pain did not limit daily activities. The Harris score was 95 points (Fig. 1). Based on the statistical analysis, we found a higher incidence of thigh pain in patients who had short stature (<160 cm) (regression test, P = 0.030).
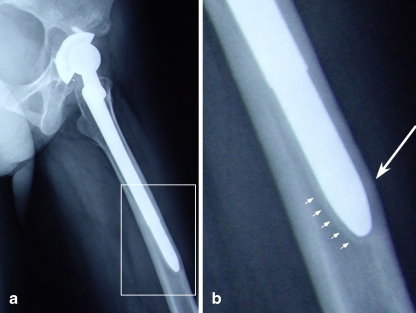
Fig. 1.
A 26-year-old female with a height of 156 cm. At 6.8-years follow-up, acetabular osteolysis was identified in zone 2; the tip of the stem impacted the anterior cortex of the femur (a), and an intramedullary sclerotic line and the associated radiolucent line were found at the end of the stem (b)
All the femoral components had bone ingrowth. No stems had subsidence or loosening. Periprosthetic radiolucent lines of the femoral stems were found in two hips in zone 1. Osteoporosis of the proximal femur and calcar was found in all patients, 65 hips had grade 2 proximal femoral remodelling, and two hips had grade 3 femoral remodelling. Seventeen hips (23%) had reactive hypertrophy of the cortical bone surrounding the distal portion of the stem in zones 3 and 5.
Sixty-nine stems (93.2%) filled the canal satisfactorily in both the coronal and sagittal planes. Five stems (6.8%) filled the canal satisfactorily in the coronal plane but not in the sagittal plane (<70% filling).
Six patients (6 hips, 8.1%) had acetabular osteolysis in zone 2. The average size of the osteolytic lesion was 4.9 ± 0.55 cm2 (range, 3.8–6.3 cm2). The lesions were first seen in radiographs at a mean of 5.1 years (range, 4–6.7 years) after surgery, and then they were confirmed by CT (Fig. 2). None of the six patients had osteolysis in the proximal femur, and there was no relationship between osteolysis and patient’s age (P = 0.41).
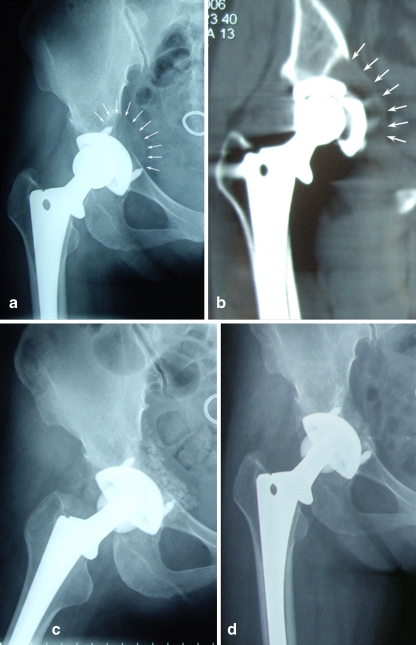
Fig. 2.
A 37-year-old female experienced severe pain in the groin and the femoral head was about to wear through the polyethylene liner. At seven years follow-up, the anteroposterial radiograph shows osteolysis in DeLee and Charnley zone 2 (a), which was confirmed by CT (b). After removal of the osteolysis granuloma, we filled the cyst with cancellous autograft and replaced the polyethylene liner and the femoral head component (c). Three months later the patient had excellent clinical function with no notable pain (d); the Harris hip score was 98 points
Five patients (5 hips, 6.8%) had femoral osteolysis, four hips in zone 1 and one hip in zone 7, but no distal osteolysis was found. The femoral lesions were less than 1.5 cm2. There was no shedding of the beads or breakage of the stems.
The average acetabular component angle was 45.2° from the horizontal (range, 38.9°–54.3°), and the anteversion angle was 13.2° (range, 10.4°–17.2°). Four acetabular components (5.4%) had a radiolucent line below 1 mm at the bone–socket interface in zone 1 or 2. No acetabular component showed aseptic loosening.
The mean wear rate of the polyethylene liner was 0.14 ± 0.11 mm/y (range, 0.09–0.37 mm/y), and the average amount of the volumetric wear was 415.773 ± 127.139 mm3 (range, 157.471–647.674 mm3). We found increased wear rates in the patients who were younger than 50 years (P = 0.022), the male patients (Student t test, P = 0.027), and the patients with a higher abduction angle (>50°) of the acetabular component (P = 0.031). There was no association between the wear and weight (regression test, P = 0.35) or the Harris score (P = 0.28).
Kaplan-Meier survivorship analysis was performed, taking radiographic loosening and revision for any reason as an endpoint. The survival rate after five years was 98.9% (95% confidence interval, 0.95–1.0).
Three hips (4.1%) were complicated by dislocation, which occurred once in all three hips. All of them were treated successfully with closed reduction under general anaesthesia, after abducted immobilisation for three months, there was no recurrence. There were no intraoperative fractures, infections, thromboembolic events, or neurological injuries. Seven hips (9.5%) had heterotopic ossification; five hips were Brooker grade 1, and two hips were Brooker grade 2.
Discussion
This study presents a group of young patients followed for a mean of 6.1 years after cementless THA with Asian size and MMA AML prosthesis. Seventy-one hips (96%) had excellent results, and three hips (4%) had good results. One hip had the head and liner revised because of osteolysis and massive wear of the polyethylene liner. The overall results were promising compared with the early results reported in past literature [5, 6, 14, 20, 21].
The incidence of anterior thigh pain with standard AML stems ranges from 8% to 81% [6, 10, 12, 14, 16, 20, 21]. Hartley et al. [9] and Kronick et al. [18] reported that micromotion between the stems and the femoral cortex may be the reason. Kim et al. [17] also suggested that an undersized femoral stem may be the reason for thigh pain. In our study, four patients complained of anterior thigh pain during the first year. One of them continued to complain of occasional pain after the first year of operation, and we also found that the stem filled the canal satisfactorily in the coronal plane but not in the sagittal plane. In the other three patients, the stem filled the canal satisfactorily in both planes. However, the tip of the stem impacted the anterior cortex of the femur, and an intramedullary sclerotic line and the associated radiolucent line were found at the end of the stem. This finding also suggests that there was micromotion. We speculated that after bone remodelling, there was enough space for the toggle of the stem, so the stress concentration disappeared, and the thigh pain subsequently resolved. Moreover, the incidence of transient thigh pain was higher in patients of short stature (<160 cm) in our study. We believe that the anterior bowing of the femur may be a major factor of anterior thigh pain. Long prostheses, such as AML stems, would increase the potential for impact with the anterior cortex of the femur, especially in those patients of short stature. Thus, we suggested that long prostheses should not be used in patients of short stature.
In our series, six patients (6 hips, 8.1%) had acetabular osteolysis in zone 2. None of the six patients had osteolysis in the proximal femur. Five patients had no pain and refused revision. They were requested to follow-up more closely in order to monitor the progression of the lesion to avoid catastrophic results. One patient had a severe pain in the groin, and the femoral head was about to wear through the polyethylene liner. Revision was performed. At operation, we found the metal acetabular shell still had bone ingrowth. After removal of the osteolysis granuloma, we filled the cyst with cancellous autograft and allograft and replaced the polyethylene liner and the femoral head component. We noticed a higher wear rate in this case (mean, 0.31 mm/year); such severe wear was not found in others. We determined that the reasons for the high wear rate were the younger age (35 years at the time of operation), smaller acetabular component (48 mm), and thin polyethylene liner (6.5 mm).
There was an alarmingly high incidence of pelvic osteolysis in zone 2 with the use of Duraloc 300 series acetabular components. Engh et al. [5] reported that 27 of 165 hips had an acetabular osteolytic lesion after 13.9 years follow-up, and only four hips had osteolysis in zone 2. In our study, six hips had osteolytic lesions in zone 2, and the lesions were larger than 1.5 cm2. In those patients, no other osteolytic lesion was found in zones 1 or 3 of the acetabulum or in the femur. We believe that those lesions were induced by the wear debris from the cup–liner interface. The Duraloc 300 series acetabular components can not prevent the rotation of the polyethylene liner. Thus, there was relative movement between the metal shell and the polyethylene liner; the center hole might have allowed debris to reach the pelvic trabecular bone. This may explain why the osteolytic lesions were located towards the central hole of the metal shell. Polyethylene wear leading to osteolysis is a common reason for revision [1, 5, 6, 14, 25], and the wear rate was higher with thin polyethylene liners [1]. In our study, the average thickness of the polyethylene liner was 9.7 mm (range, 6.5–13.5 mm), and we used 28-mm CoCr alloy heads as routine to avoid excessive polyethylene wear.
In our patients, the incidence of femoral osteolysis was lower than Engh et al. reported [6]. In our series, all of the femoral osteolytic lesions were in Gruen zones 1 or 7, which was the same as Engh et al. described [6]. This could be due to the satisfactory filling of the femur and the extensively porous-coated surface which limits the effective joint space [24]. Additionally, it is possible that the osteolysis rate was relatively low in our study because of the limited duration of the follow-up.
This study revealed that primary THA with Asian size and MMA AML stems had acceptable mid-term result in young Chinese patients. Wear of the polyethylene liner and massive osteolysis in the pelvis are still our great concerns, as they may create potential problems for future revision. Therefore, further studies are still needed.
References
- 1.Astion DJ, Saluan P, Stulberg BN, Rimnac CM, Li S. The porous-coated anatomic total hip prosthesis: failure of the metal-backed acetabular component. J Bone Joint Surg Am. 1996;78:755–766. doi: 10.2106/00004623-199605000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Bessette BJ, Fassier F, Tanzer M, Brooks CE. Total hip arthroplasty in patients younger than 21 years: a minimum, 10-year follow-up. Can J Surg. 2003;46:257–262. [PMC free article] [PubMed] [Google Scholar]
- 3.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 4.DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 20–32 [PubMed]
- 5.Engh CA Jr, Claus AM, Hopper RH Jr, Engh CA (2001) Long-term results using the anatomic medullary locking hip prosthesis. Clin Orthop Relat Res 137–146 [DOI] [PubMed]
- 6.Engh CA, Jr, Culpepper WJ, Engh CA. Long-term results of use of the anatomic medullary locking prosthesis in total hip arthroplasty. J Bone Joint Surg Am. 1997;79:177–184. doi: 10.1302/0301-620X.79B2.7640. [DOI] [PubMed] [Google Scholar]
- 7.Engh CA, Massin P, Suthers KE (1990) Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res 107–128 [PubMed]
- 8.Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 17–27 [PubMed]
- 9.Hartley WT, McAuley JP, Culpepper WJ, Engh CA, Jr, Engh CA., Sr Osteonecrosis of the femoral head treated with cementless total hip arthroplasty. J Bone Joint Surg Am. 2000;82-A:1408–1413. doi: 10.2106/00004623-200010000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Heekin RD, Callaghan JJ, Hopkinson WJ, Savory CG, Xenos JS. The porous-coated anatomic total hip prosthesis, inserted without cement. Results after five to seven years in a prospective study. J Bone Joint Surg Am. 1993;75:77–91. doi: 10.2106/00004623-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Jana AK, Engh CA, Jr, Lewandowski PJ, Hopper RH, Jr, Engh CA. Total hip arthroplasty using porous-coated femoral components in patients with rheumatoid arthritis. J Bone Joint Surg Br. 2001;83:686–690. doi: 10.1302/0301-620X.83B5.11539. [DOI] [PubMed] [Google Scholar]
- 12.Johnston DW, Davies DM, Beaupre LA, Lavoie G. Standard anatomical medullary locking (AML) versus tricalcium phosphate-coated AML femoral prostheses. Can J Surg. 2001;44:421–427. [PMC free article] [PubMed] [Google Scholar]
- 13.Kim YH. Cementless total hip arthroplasty with a close proximal fit and short tapered distal stem (third-generation) prosthesis. J Arthr. 2002;17(7):841–850. doi: 10.1054/arth.2002.33555. [DOI] [PubMed] [Google Scholar]
- 14.Kim YH, Kim JS, Cho SH (1999) Primary total hip arthroplasty with the AML total hip prosthesis. Clin Orthop Relat Res 147–158 [DOI] [PubMed]
- 15.Kim YH, Kim JS, Oh SH, Kim JM. Comparison of porous-coated titanium femoral stems with and without hydroxyapatite coating. J Bone Joint Surg Am. 2003;85-A:1682–1688. doi: 10.2106/00004623-200309000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Kim YH, Kim VE. Cementless porous-coated anatomic medullary locking total hip prostheses. J Arthr. 1994;9:243–252. doi: 10.1016/0883-5403(94)90078-7. [DOI] [PubMed] [Google Scholar]
- 17.Kim YH, Oh SH, Kim JS, Koo KH. Contemporary total hip arthroplasty with and without cement in patients with osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85-A:675–681. doi: 10.2106/00004623-200304000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Kronick JL, Barba ML, and Paprosky WG (1997) Extensively coated femoral components in young patients. Clin Orthop Relat Res 263–274 [PubMed]
- 19.Martell JM, Berdia S. Determination of polyethylene wear in total hip replacements with use of digital radiographs. J Bone Joint Surg Am. 1997;79:1635–1641. doi: 10.2106/00004623-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Nercessian OA, Wu WH, Sarkissian H. Clinical and radiographic results of cementless AML total hip arthroplasty in young patients. J Arthr. 2001;16:312–316. doi: 10.1054/arth.2001.21503. [DOI] [PubMed] [Google Scholar]
- 21.Ohsawa S, Fukuda K, Matsushita S, et al. Middle-term results of anatomic medullary locking total hip arthroplasty. Arch Orthop Trauma Surg. 1998;118:14–20. doi: 10.1007/s004020050302. [DOI] [PubMed] [Google Scholar]
- 22.Phillips NJ, Stockley I, Wilkinson JM. Direct plain radiographic methods versus EBRA-digital for measuring implant migration after total hip arthroplasty. J Arthr. 2002;17:917–925. doi: 10.1054/arth.2002.34529. [DOI] [PubMed] [Google Scholar]
- 23.Purtill JJ, Rothman RH, Hozack WJ, Sharkey PF (2001) Total hip arthroplasty using two different cementless tapered stems. Clin Orthop Relat Res 121–127 [DOI] [PubMed]
- 24.Schmalzried TP, Jasty M, Harris WH. Periprosthetic bone loss in total hip arthroplasty. Polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg Am. 1992;74:849–863. [PubMed] [Google Scholar]
- 25.Stulberg BN, Singer R, Goldner J, Stulberg J (1997) Uncemented total hip arthroplasty in osteonecrosis: a 2- to 10-year evaluation. Clin Orthop Relat Res 116–123 [PubMed]
- 26.Teloken MA, Bissett G, Hozack WJ, Sharkey PF, Rothman RH. Ten to fifteen-year follow-up after total hip arthroplasty with a tapered cobalt-chromium femoral component (tri-lock) inserted without cement. J Bone Joint Surg Am. 2002;84-A:2140–2144. doi: 10.2106/00004623-200212000-00003. [DOI] [PubMed] [Google Scholar]