Abstract
In this paper, 152 patients with 187 osteonecrotic femoral heads (83 idiopathic, 56 corticosteroid induced, 40 post-traumatic, seven alcohol abuse and one associated with gout) were classified according to the staging by Ficat and Arlet (Ischemia and necroses of bone, Williams and Wilkins, Baltimore, Maryland, pp 171–182, 1980); four were in Stage I, 82 in Stage II and 101 in Stage III. The majority of the patients were young (average age 35.5 years). Multiple drilling, curettage of the necrotic bone and muscle-pedicle bone grafting using tensor fascia lata was carried out in all patients except in six adolescents, where sartorius grafting was performed. Cheilectomy of the femoral head and subcutaneous adductor tenotomy were also performed in the advanced stages. During the follow up of 10 to 21.5 years (average 16.5 years), radiological improvement was noted in 81.3% of patients in Stage II and 70.1% of patients in Stage III cases. Excellent and good results according to the Hospital for Special Surgery (HSS) score were obtained in 100% of cases in Stage I, 92% in Stage II and 80.4% in stage III, with a survivorship of 91% in Stage II and 82% in Stage III cases. The patients having an HSS score below 20 (non-survival) were recommended for total hip replacement (THR) therapy.
Résumé
152 patients présentant 187 nécroses de la tête fémorale (83 idopathiques, 56 après corticoïdes, 40 post-traumatiques, 7 d’origine éthyliques et une associée à une goutte) ont été traités. Selon les classifications de Ficat et Arlet, 4 étaient au stade I, 82 au stade II et 101 au stade III. La majorité des patients étaient jeunes (35,5 ans). Forage et curetage de la nécrose et greffe pédiculaire ont été réalisés chez 6 adolescents. Cheilectomie et ténotomie percutanées des adducteurs ont été également réalisées. Le suivi moyen a été de 16.5 ans (10 à 21.5 ans). Il n’y a pas d’altération radiographique chez les patients de stade I. Une amélioration a été notée dans 81.3% des patients de stade II et 70.1% des patients de stade III. De bons résultats cliniques ont été mis en évidence (score de Salvati et Wilson) dans 100% des patients de stade I, 92% au stade II et 80.4% au stade III avec un taux de survie de 91% au stade II, et 82% de stade III. Les patients présentant une aggravation de la nécrose avec un score en dessous de 20 ont été considérés comme devant bénéficier d’une prothèse totale.
Introduction
Untreated osteonecrosis of the femoral head ultimately leads to collapse and degeneration of the hip joint. The predegenerative stages of osteonecrosis, especially when seen in young individuals, should be treated by a femoral head preserving operation with the objective to delay and possibly avert the above consequences.
Femoral head preserving operations produce good results in the early stages of osteonecrosis but most of their results were inconsistent and have deteriorated markedly in longer follow up, as seen following different osteotomies [5, 7, 12, 20, 23], core decompression [3, 9, 22] and non-vascularised strut grafting with the tibia or fibula [15]. Cancellous bone grafting after the curettage of necrotic bones fails to relieve pain or prevent progressive collapse of the femoral head [13, 18].
Recently, different vascularised bone graftings, such as free vascularised fibular grafting combined with free iliac chip grafting [4, 17, 21, 24] and vascular pedicle iliac crest grafting [8, 11, 16], provided encouraging results, especially in the early stages of necrosis. The use of quadratus femoris (Q-F) muscle-pedicle bone graft (MPBGs) combined with free cancellous grafts provided good results in the early stages of osteonecrosis but poor results in advanced stages [14]. However, even in advanced stages of osteonecrosis, subcutaneous adductor tenotomy, cheilectomy, drilling and muscle-pedicle bone grafting provided symptomatic relief irrespective of femoral head deformity [2].
The results of the use of different MPBGs alone using of Q-F or sartorius or gluteus medius or tensor fascia lata (TFL) in different stages of osteonecrosis of the femoral head were reported by Baksi [1, 2]. But, subsequently, it was felt that, since the necrotic area is predominantly present in the antero-superior aspect of the femoral head, its curettage from anterior aspect and packing with the adjacent MPBG was the treatment of choice. Hence, TFL grafting [2] in adults and sartorius grafting [1] in adolescents providing good vascularity and better strut effects were performed through an anterior approach in both early and advanced predegenerative stages of necrosis. Their long-term results with survivorship analysis over 15 years are being reported.
Materials and methods
One hundred and fifty two patients with 187 osteonecrotic femoral heads who gave informed consent to undergo this study were treated during the period from June 1983 to December 1997 by TFL MPBG in all except in six adolescents, where sartorius MPBG was used, since their iliac crest was cartilaginous. TFL MPBG is seen to be more vascular than sartorius grafts. Eleven patients were lost to follow up. Eighty three (44.3%) osteonecrotic femoral heads were idiopathic, 56 (30%) corticosteroid induced, 40 (21.4%) post-traumatic (36 after the union of femoral neck fractures and four after dislocations of the hip), seven (3.8%) after alcohol abuse and one (0.5%) associated with gout. The ages of the patients varied from 16 to 62 years (average 35.5). Ninety one were men and 61 women. Sixty four had osteonecrosis on the right hip, 53 on the left and 35 had bilateral involvement.
The indication of surgery was pain and discomfort around the hip during walking, sitting cross-legged and even at rest and the limitation of movement of the hip, particularly in advanced stages of osteonecrosis, where 70–90° flexion was often preserved but other movements were considerably restricted or absent. The presence of a good range of movement at least in one direction, particularly flexion, was considered important for this femoral head preserving operation. The average duration of symptoms before this operation was 17.5 months.
Osteonecrosis was diagnosed by clinical and radiological studies in all cases and magnetic resonance imaging (MRI) and computed tomography (CT) scanning in selected cases. Since the late 1980s, MRI has been used in cases where there was diagnostic dilemma. CT scanning was necessary particularly to evaluate the distorted trabecular pattern of the femoral head and study the pseudofracture line in the osteonecrotic zone. The diagnosis was confirmed by histopathological examination of the subarticular bone obtained from the femoral head during the operation in all cases. Clinical evaluation pre- and postoperatively was carried out using the hip rating system of the Hospital for Special Surgery (HSS) [19], which measured pain, walking, muscle power and the range of motion and function. Each function was scored from 0 (worst) to 10 (normal).
Preoperative radiological staging of osteonecrosis was done according to Ficat and Arlet [6]. Accordingly, among the 176 cases studied, four were in Stage I, 75 in Stage II and 97 in Stage III necrosis. However, badly damaged femoral heads with a collapse of 5 mm or more were not included here. Postoperative radiological assessment of the cases was carried out on the basis of radiological criteria of healing [2]. The patients were followed up for 10 to 21.5 years (average 16.5 years).
The result was considered to be successful (survived) if the patient was asymptomatic without radiological deterioration of the disease or radiological progression to a higher stage of Ficat and Arlet [6] or symptomatic with a clinical HSS [19] score of 20 or above, even in the presence of mild radiological deterioration or degenerative change. On the other hand, the result was considered to be unsuccessful (non-survived) if the patient was symptomatic with radiological deterioration, resulting in the reduction of the clinical HSS score to below 20, requiring subsequent operative intervention. For practical purposes, survival analysis of our treatment modalities was performed on the basis of the survival definition as stated above. The survival probabilities have been estimated using the Kaplan-Meier estimator [10], along with 95% confidence intervals for Stages II and III in 10-year and 15-year intervals, respectively. We have used the S Plus statistical package for our analysis and to draw the graphs.
Surgical technique of the tensor fascia lata muscle-pedicle bone graft
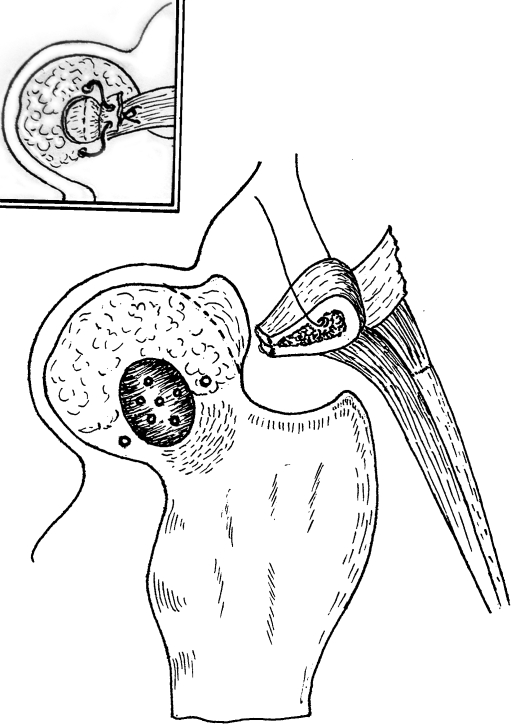
Through an anterior approach to the affected hip, the surgical technique described by Baksi [2] was followed. TFL MPBG with an isolated overlying piece of fascial sleeve was prepared with the anterior-most 2.5 cm fibres of TFL muscle, along with the osteotomised corresponding 2.5 cm length and height of the iliac graft (Fig. 1). The gluteus minimus fibres which are intermingled with TFL muscle of the graft in the deeper plane are separated. The straight head of the rectus femoris which lies deep to the sartorius is sectioned transversely 2 cm below its origin. The capsulotomy, curettage, of the necrotic area and multiple drilling of the femoral head and TFL muscle-pedicle bone grafting was performed inside the slot made over the antero-superior aspect of the femoral head in all stages of necrosis. The cheilectomy of the femoral head in its superior, anterior and antero-inferior part whenever required and subcutaneous adductor tenotomy were added for the improvement of limited movement in advanced stages of osteonecrosis.
Fig. 1.
Tensor fascia lata (TFL) muscle-pedicle bone graft (MPBG) is prepared with the passage of a Vicryl thread through the bone. A slot with multiple drill holes at its depth is shown over the antero-superior aspect of the femoral head for grafting. The line of cheilectomy is shown by dotted lines over the deformed femoral head. Two drill holes are shown on either side of the slot for the passage of the Vicryl thread for anchoring the graft through its fascial sleeve after impaction inside the slot (inset)
The above technique was improved further by taking special measures for the fixation of the MPBG as follows (Fig. 1). The prepared TFL MPBG. is brought to the slot, splitting the inferiorly retracted gluteus minimus muscle fibres for its direct passage without any tension. The bony portion of the MPBG is shaved according to the contour of the slot. One drill hole is made on either side of the slot over the femoral head (Fig. 1) and also along the axial length of the MPBG for the passage of one Vicryl thread (Fig. 1) for anchoring the graft over the femoral head. The MPBG is impacted inside the slot and anchored with the above Vicryl thread. It is then tied together with the overlying fascial sleeve (Fig. 1 inset). The divided ends of the rectus femoris are reattached. The separated gluteus minimus fibres are stitched back into the iliac crest. The wound is closed in layers around the two suction drains.
Surgical technique of the sartorius MPBG
The technique was described by Baksi [1] where the sartorius origins into the anterior-superior iliac spine and the notch below it, together with a portion of the corresponding segment of ilium was osteotomised to prepare the MPBG. The above technique is improved further by anchoring the sartorius graft using a Vicryl thread passed through holes made on either side of the slot over the femoral head.
Aftercare
Associated hip movements are encouraged in the early postoperative period. Vigorous hip movements are started at four weeks with the patients lying on the bed. The cases with significant preoperative limitation of movement of the hip in advanced stages are treated during the early postoperative period with 7.5 to 10 lbs skin traction of the operated limb for 2–3 weeks, accompanied by intermittent hip motion. Non-weight-bearing crutch walking is started from five weeks. Full weight-bearing is allowed from four to five months after the operation. In bilateral cases, a wheel chair is used during the period of non-weight-bearing.
Results
Clinical improvement was considered according to the criteria of HSS score [19]. The radiological criteria [2] of improvement was judged by the diminution of density of the necrotic portion of the femoral head, return to normal density of the preoperative rarefied areas (particularly in early cortisone-induced and idiopathic disease), restoration of the normal trabecular pattern, disappearance of the crescent sign, healing of cystic areas and of the fracture line within the necrotic area or between it and the healthy bone, improvement in the shape of the femoral head, particularly after cheilectomy, and improvement of the radiological joint space. Both early and advanced stages of the disease showed significant postoperative clinical improvement (Table 1) and radiological improvement (Table 2). Overall results in different stages of osteonecrosis are shown in Table 3. Examples of excellent results of Stage III osteonecrosis are shown in Fig. 2. Survival analysis (along with 95% confidence intervals) was carried out according to the criteria of survivorship as stated before and the results are shown in Figs. 3 and 4.
Table 1.
Clinical improvement of the average score according to Salvati and Wilson [19] in different stages of osteonecrosis (average 16.5 years follow up)
| Score | Stage I | Stage II | Stage III |
|---|---|---|---|
| Preoperative | 34 | 26.5 | 22 |
| Postoperative | |||
| At 5 years | 37.5 | 33.3 | 31 |
| At 10 years | 35 | 32.1 | 28.7 |
| At 15 years | 35 | 31.3 | 25.6 |
Table 2.
Postoperative radiological analysis in different stages of osteonecrosis (average 16.5 years follow up)
| Radiological alterations | Stage I, n = 4 | Stage II, n = 75 | Stage III, n = 97 |
|---|---|---|---|
| Radiological improvement | 4 (100.0%) | 61 (81.3%) | 68 (70.1%) |
| Collapse | |||
| <2 mm | − | 3 (4%) | 14 (14.4%) |
| 2−3 mm | − | − | 2 (2.1%) |
| >3 mm | − | − | − |
| Osteoarthrosis | − | 11 (14.7%) | 12 (12.4%) |
| Radiological progression | − | 14 (18.6%) | 29 (29.9%) |
Table 3.
Overall results in different stages of osteonecrosis (average 16.5 years follow up)
| Gradation of results | Stage I, n = 4 | Stage II, n = 75 | Stage III, n = 97 |
|---|---|---|---|
| Excellent | 4 (100%) | 61 (81.3%) | 35 (36.1%) |
| Good | − | 8 (10.7%) | 43 (44.3%) |
| Fair | − | 6 (8%) | 16 (16.5%) |
| Poor | − | − | 2 (2.1%) |
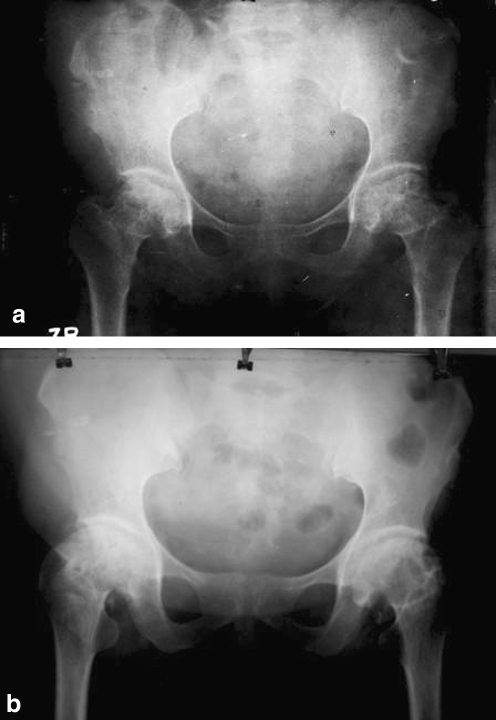
Fig. 2.
a Preoperative antero-posterior (AP) radiograph of a 35-year-old lady with bilateral idiopathic osteonecrosis (Stage III) with 2-mm collapse. b Seventeen-year follow up AP radiograph of the same patient showing satisfactory healing of the necrotic area, with further improvement of the shape of the femoral head. The clinical result was excellent (hip score=34)
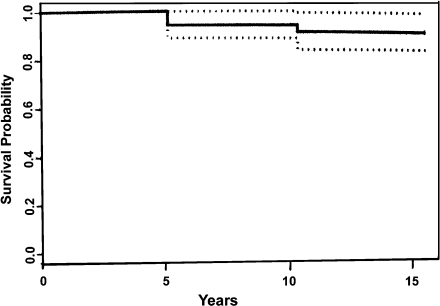
Fig. 3.
Kaplan-Meier survival probabilities for Stage II (at 10 years and 15 years after operation) with 95% confidence intervals (shown by the dotted lines)
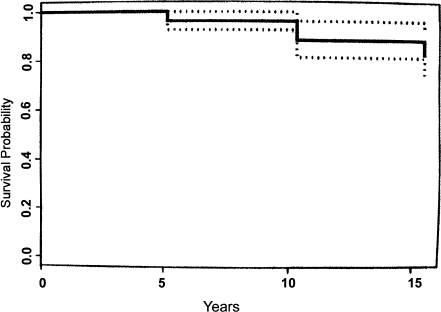
Fig. 4.
Kaplan-Meier survival probabilities for Stage III (at 10 and 15 years after operation) with 95% confidence intervals (shown by the dotted lines)
All four cases of Stage I osteonecrosis showed clinical improvement without radiological alteration throughout the period of follow up.
Overall, clinical improvement having excellent and good results (a score of more than 24) were obtained in 69 (92%) patients of Stage II and 78 (80.4%) patients of Stage III whereas clinical and radiological improvement was noted in 61 (81.3%) patients of Stage II and 68 (70.1%) patients of Stage III cases during the follow up period of 10 to 21.05 years (average 16.5 years). The survival probability estimated for Stage II was 0.91 (Fig. 3) and for Stage III was 0.82 (Fig. 4) after 15 years.
Complications
Several complications included superficial wound infection in nine (5.1%) hips, terminal limitation of hip movements in 20 (11.4%) and the persistence of painless limp in 16 (9.09%) cases in advanced stages of osteonecrosis.
Discussion
Most of the femoral head preserving operations, being extra-articular procedures, fail to rectify the associated intracapsular pathological alterations, particularly in advanced stages, thereby, they fail to provide satisfactory long-term outcomes, in spite of their good results during early follow up.
All four cases of Stage I osteonecrosis followed during this study showed clinical improvement without radiological alteration throughout the period of follow up. In Stage II cases, clinical improvement (HSS score of more than 24) were obtained in 69 (92%) patients, whereas radiological improvement was noted in 61 (81.3%) patients. The clinical results did not correlate with the radiological alterations of the femoral head, since most of them achieved satisfactory clinical scoring, despite the lack of radiological improvement or the occurrence of limited collapse and early osteoarthrosis. Therefore, the survival probability for Stage II is 0.91 after 15 years (Fig. 3).
In Stage III cases, clinical improvement (HSS score of more than 24) was noted in 78 (80.4%) patients, whereas radiological improvement was obtained in 68 (70.1%) patients. Most of the cases who had a preoperative 2- to 4-mm collapsed segment demonstrated clinical improvement without radiological deterioration. Most of the cases having fair results did not show further clinical deterioration but showed degenerative changes at 15 years follow up and achieved a clinical score above 20 were classed as “survived”. Therefore, the overall survival probability of Stage III cases was 0.82 after 15 years (Fig. 4). The cases who showed moderate degenerative change or the progression of collapse resulting in symptomatic deterioration and the reduction of clinical score below 20 were considered as failure or non-survived. Most of them are managing their daily activities with occasional pain and functional disability, though they may need total hip replacement (THR) therapy in due course.
The results were good and comparable among the cases of idiopathic and steroid-induced osteonecrosis who stopped steroid intake pre- and postoperatively. However, the results among the post-traumatic cases of osteonecrosis showed delayed healing and functional recovery.
In our series, immediate relief of pain was regularly achieved by the relief of increased subarticular venous pressure in osteonecrosis and intracystic pressure in the presence of osteoarthrosis by multiple drilling and judicious curettage of the necrotic area and the release of capsular stretching effect by cheilectomy. The permeation of granulation tissues into the drilled area growing from the adjacent MPBG helps in revascularisation of the necrotic area, resulting in long-lasting pain relief. The above factors, in addition to subcutaneous adductor tenotomy in advanced stages, improved the hip movement.
Preoperative radiographic lesion of larger size did not appear to be an adverse factor for the success of our technique because the actual necrotic area which needs to be removed is often much smaller than the radiograph suggests and can usually be repaired with the MPBG alone [2]. The radiographically, a dense or rarefied zone surrounding the actual necrotic area is usually viable and is seen to bleed during drilling.
In our cases of pre-collapse stage of osteonecrosis, TFL or sartorius MPBG being cortico-cancellous provided a better strut effect to the subchondral area and prevented their collapse more efficiently than those obtained by Q-F [14] or gluteus medius MPBG [1], having mostly spongy bones [2]. Moreover, the Q-F muscle is too short in length to reach the centre or antero-superior part of the femoral head where the osteonecrotic area predominates. Overall, we observed an 11.3% incidence of collapse in our series, compared to 60% [13] and 39% [18] incidence with the use of free cancellous bone grafts, suggesting the superiority of the MPBG in terms of repair of the necrotic segment.
Even the presence of limited (up to 2–4 mm) preoperative collapse was compatible with a successful functional outcome, as well as long-term survivorship noted in our series, because the repair of the necrotic area as above and the rectification of the deformed femoral head (Fig. 3) by cheilectomy and elevation of the collapsed segment by packing of the MPBG, in most cases, improved functional outcome. However, on rare occasions, the cases having ongoing necrosis or technical failure developed pain in the hip with further collapse and progressive degeneration with deterioration of functional outcome may need THR in due course. Furthermore, in most of the advanced stages, articular cartilage appeared almost normal or minimally affected as the osteonecrotic cases in our series were usually of several months to a few years duration. In those cases, the cartilage which yielded to gentle pressure retained elasticity and recovered with improvement or maintenance of the radiological joint space in the majority following this procedure.
Overall, in our series, the preoperative score of Salvati and Wilson [19] improved significantly in the pre-collapse stage of osteonecrosis and also in the post-collapse predegenerative stage, irrespective of the preoperative size of the lesion and the limited degree of collapse of the femoral head.
The vascularised fibular bone grafting combined with free iliac bone chips provided 86% survivorship, compared to 30% using non-vascularised fibular grafting in seven years follow up only in the early stage of necrosis [17], whereas they showed only 69.6% survivorship in five years when performed among combined early and Stage III necrosis [24]. The vascular pedicle iliac crest grafting provided 40% [16] to 52% [11] good results for Stage II and early Stage III necrosis during four to 14 years follow up and provided a survival rate of 85% in five years and 61% in 10 years, mostly among Stage II cases [8]. Our procedures showed over 80% survivorship in all of the predegenerative stages of necrosis at 15 years follow up. The confidence bands are also narrow, indicating that our estimates have little variability.
The vascularised fibular or iliac crest grafting procedures are technically demanding and, based on a single arteriovenous pedicle, may undergo torsion or injury or thrombosis per- and postoperatively, resulting in the loss of their vascularity and viability, which may be the reason of their unsatisfactory long-term results. On the other hand, numerous vascular communications of MPBGs are well-protected within the muscle bed, unless the muscle fibres undergo acute angulation or torsion, and then the grafting procedures appear relatively easier technically.
Since this method provided satisfactory overall results in all of the predegenerative stages and significant functional outcome with improved shape of the femoral head, this treatment protocol can be recommended among patients with a predegenerative stage of osteonecrosis of the femoral head, where the majority of cases are young. In the event of its long-term failure, THR can always be carried out.
Acknowledgement
We are grateful to Dr. Saurabh Ghosh, Assistant Professor, Applied Statistics Unit, Indian Statistical Institute, Kolkata, India, for his kind help in the statistical analysis of the survivorship data.
Contributor Information
Durgapada P. Baksi, Phone: +91-33-22344901, Email: dpbaksiorth@hotmail.com
Ananda Kisor Pal, Email: orthoakpal@yahoo.com.
Debadyuti D. Baksi, Email: ddbaksiorth@gmail.com
References
- 1.Baksi DP. Treatment of post-traumatic avascular necrosis of the femoral head by multiple drilling and muscle-pedicle bone grafting. Preliminary report. J Bone Joint Surg Br. 1983;65:268–273. doi: 10.1302/0301-620X.65B3.6341373. [DOI] [PubMed] [Google Scholar]
- 2.Baksi DP. Treatment of osteonecrosis of the femoral head by drilling and muscle-pedicle bone grafting. J Bone Joint Surg Br. 1991;73:241–245. doi: 10.1302/0301-620X.73B2.2005147. [DOI] [PubMed] [Google Scholar]
- 3.Bozic KJ, Zurakowski D, Thornhill TS. Survivorship analysis of hips treated with core decompression for nontraumatic osteonecrosis of the femoral head. J Bone Joint Surg Am. 1999;81(2):200–209. doi: 10.2106/00004623-199902000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Brunelli G, Brunelli G., Jr Free microvascular fibular transfer for idiopathic femoral head necrosis: long-term follow-up. J Reconstr Microsurg. 1991;7:285–295. doi: 10.1055/s-2007-1006786. [DOI] [PubMed] [Google Scholar]
- 5.Dean MT, Cabanela ME. Transtrochanteric anterior rotational osteotomy for avascular necrosis of the femoral head. Long-term results. J Bone Joint Surg Br. 1993;75:597–601. doi: 10.1302/0301-620X.75B4.8331115. [DOI] [PubMed] [Google Scholar]
- 6.Ficat RP, Arlet J. Treatment of bone ischemia and necrosis. In: Hungerford DS, editor. Ischemia and necroses of bone. Baltimore, Maryland: Williams and Wilkins; 1980. pp. 171–182. [Google Scholar]
- 7.Gottschalk F. Indications and results of intertrochanteric osteotomy in osteonecrosis of the femoral head. Clin Orthop Relat Res. 1989;249:219–222. [PubMed] [Google Scholar]
- 8.Hasegawa Y, Sakano S, Iwase T, Iwasada S, Torii S, Iwata H. Pedicle bone grafting versus transtrochanteric rotational osteotomy for avascular necrosis of the femoral head. J Bone Joint Surg Br. 2003;85:191–198. doi: 10.1302/0301-620X.85B2.13190. [DOI] [PubMed] [Google Scholar]
- 9.Hungerford DS, Lennox DW. Diagnosis and treatment of ischaemic necrosis of the femoral head. In: Evarts MC, editor. Surgery of the musculoskeletal system. 2. New York: Churchill Livingstone; 1990. pp. 2757–2794. [Google Scholar]
- 10.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Statist Assn. 1958;53:457–481. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 11.Leung PC. Femoral head reconstruction and revascularization. Treatment for ischemic necrosis. Clin Otrhop Relat Res. 1996;323:139–145. doi: 10.1097/00003086-199602000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Maistrelli G, Fusco U, Avai A, Bombelli R. Osteonecrosis of the hip treated by intertrochanteric osteotomy. A four- to 15-year follow-up. J Bone Joint Surg Br. 1988;70(5):761–766. doi: 10.1302/0301-620X.70B5.3192575. [DOI] [PubMed] [Google Scholar]
- 13.Merle d’Aubigne R, Postel M, Mazabraud A, Gueguen J. Idiopathic necrosis of the femoral head in adults. J Bone Joint Surg Br. 1965;47:612–633. [PubMed] [Google Scholar]
- 14.Meyers MH. The treatment of osteonecrosis of the hip with fresh osteochondral allografts and with the muscle pedicle graft technique. Clin Orthop Relat Res. 1978;130:202–209. [PubMed] [Google Scholar]
- 15.Nelson LM, Clark CR. Efficacy of phemister bone grafting in non-traumatic aseptic necrosis of the femoral head. J Arthroplasty. 1993;8:253–258. doi: 10.1016/S0883-5403(06)80086-0. [DOI] [PubMed] [Google Scholar]
- 16.Pavlocic V, Dolinar D, Arnež Z. Femoral head necrosis treated with vascularized iliac crest graft. Int Orthop. 1999;23:150–153. doi: 10.1007/s002640050334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Plakseychuk AY, Kim S-Y, Park B-C, Varitimidis SE, Rubash HE, Sotereanos DG. Vascularized compared with nonvascularized fibular grafting for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85:589–596. doi: 10.2106/00004623-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Saito S, Ohzono K, Ono K. Joint-preserving operations for idiopathic avascular necrosis of the femoral head. Results of core decompression, grafting and osteotomy. J Bone Joint Surg Br. 1988;70:78–84. doi: 10.1302/0301-620X.70B1.3276703. [DOI] [PubMed] [Google Scholar]
- 19.Salvati EA, Wilson PD., Jr Long-term results of femoral-head replacement. J Bone Joint Surg Am. 1973;55:516–524. [PubMed] [Google Scholar]
- 20.Schneider W, Aigner N, Pinggera O, Knahr K. Intertrochanteric osteotomy for avascular necrosis of the head of the femur. Survival probability of two different methods. J Bone Joint Surg Br. 2002;84:817–824. doi: 10.1302/0301-620X.84B6.12837. [DOI] [PubMed] [Google Scholar]
- 21.Scully SP, Aaron RK, Urbaniak JR. Survival analysis of hips treated with core decompression or vascularized fibular grafting because of avascular necrosis. J Bone Joint Surg Am. 1998;80:1270–1275. doi: 10.2106/00004623-199809000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Simank HG, Brocai DRC, Brill C, Lukoschek M. Comparison of results of core decompression and intertrochanteric osteotomy for nontraumatic osteonecrosis of the femoral head using Cox regression and survivorship analysis. J Arthroplasty. 2001;16:790–794. doi: 10.1054/arth.2001.23580. [DOI] [PubMed] [Google Scholar]
- 23.Tooke SMT, Amstutz HC, Hedley AK. Results of transtrochanteric rotational osteotomy for femoral head osteonecrosis. Clin Orthop Relat Res. 1987;224:150–157. [PubMed] [Google Scholar]
- 24.Urbaniak JR, Coogan PG, Gunneson EB, Nunley JA. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting. A long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am. 1995;77:681–694. doi: 10.2106/00004623-199505000-00004. [DOI] [PubMed] [Google Scholar]