Abstract
We retrospectively evaluated 17 hips in 16 patients who underwent a periacetabular osteotomy for the treatment of dysplastic hip with Perthes-like deformities. These residual deformities were graded using the Stulberg classification system. There were three class II hips, 11 class III hips and three class IV hips preoperatively. The average age of the patients at surgery was 36.9 years and the average follow-up was 6.6 years. The average Harris hip score significantly improved from the preoperative value of 68.2 points to 91.1 points postoperatively. The average postoperative range of motion in all directions did not change significantly from the preoperative value. The average postoperative Harris hip score of class IV hips was smaller than that of the class II or class III hips. The standard radiographic evaluations also showed significant improvements postoperatively. Periacetabular osteotomy without combined femoral osteotomies, as a treatment for patients with Perthes-like deformities, produced good clinical and radiographic results.
Résumé
Nous avons évalué de façon rétrospective 17 hanches chez 16 patients qui ont bénéficié d’une ostéotomie périacétabulaire pour le traitement de hanche dysplasiques avec des déformations de type Perthes. Les déformations résiduelles ont été classées selon la méthode de Stulberg. Il y avait en préopératoire 3 hanches de type II, 11 de type III et 3 de type IV. L’âge moyen des patients au moment de l’intervention était de 36.9 ans et le suivi moyen de 6.6 ans. Le score moyen de Harris a été amélioré de façon significative passant de 68.2 points à 91.1 points en post opératoire. La mobilité post opératoire n’a pas été affectée de façon significative par rapport à la mobilité préopératoire. Le score de Harris moyen post opératoire des hanches de type IV est légèrement inférieur à ceux de type II ou III. Les radiographies standards ont montré une amélioration significative en post opératoire. L’ostéotomie périacétabulaire sans qu’elle soit associée à une ostéotomie fémorale est un traitement qui donne donne de bons résultats tant sur le plan clinique que radiographique sur des hanches déformées de type Perthes.
Introduction
We often see residual deformities of the hip following the treatment for developmental dysplasia of the hip (DDH) or after Legg-Calvé-Perthes disease. Characteristics of these deformities are the shortening of the femoral neck, the relative overgrowth of the greater trochanter, the flattened femoral head and secondary acetabular dysplasia. These are so-called Perthes-like deformities [11]. Surgical treatment for dysplastic hip with Perthes-like deformities in skeletally mature patients remains controversial. It is unclear whether we should treat both the deformed proximal femora and the dysplastic acetabulum or treat them respectively.
Curved periacetabular osteotomy (CPO) [9], a modification of the Bernese periacetabular osteotomy technique developed by Ganz et al. [3], has been used as an effective treatment for osteoarthritis of dysplastic hips at our institution. The effects of this osteotomy on dysplastic hips with Perthes-like deformities have not been evaluated. The purpose of this study was to evaluate the clinical and radiographic results of CPO for dysplastic hips with Perthes-like deformities following the treatment for DDH or after Legg-Calvé-Perthes disease.
Patients and methods
Between 1996 and 2003, 17 consecutive symptomatic hips in 16 patients (six men and ten women) with Perthes-like deformities underwent CPO that was performed by the senior author (MN). Ten hips in ten women had conservative treatments for DDH during childhood. Legg-Calvé-Perthes disease was recognised in three hips in three men. The past history of the remaining four hips in three men was unknown. All 17 hips had secondary acetabular dysplasia.
Preoperative morphology of the hip was graded using the Stulberg classification system as follows [12]. Class I hips were completely normal. Class II hips had a spherical femoral head with one or more of the following abnormal characteristics of the femoral head, neck or acetabulum: (1) larger than normal femoral head; (2) shorter than normal femoral neck; or (3) abnormal steep acetabulum. Class III hips had a non-spherical, non-flat femoral head with abnormal characteristics of the femoral head, neck and acetabulum (as described for class II). Class IV hips had a flat head and abnormalities of the femoral head, femoral neck and acetabulum. Lastly, class V hips had a flat femoral head and a normal femoral neck and normal acetabulum.
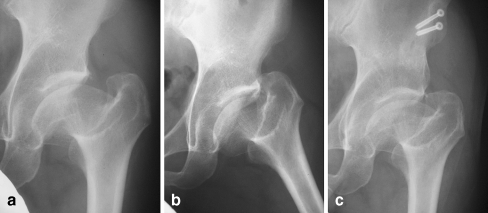
Indications for CPO included symptomatic acetabular dysplasia lasting longer than five months, a lateral centre-edge angle (CE angle) of Wiberg [15] less than 16° on anteroposterior (AP) radiographs and an improvement in joint congruency on AP radiograph in the abducted hip position [8]. The average age of the patients at the time of surgery was 36.9 years (range 20–54 years) and the average follow-up period was 6.6 years (range 3–10 years). Preoperatively, we observed the widening of the cartilage space on an AP radiograph of the pelvis in the abducted position for all hips (Fig. 1).
Fig. 1.
a A preoperative anteroposterior (AP) radiograph of the left hip of a 25 year-old woman shows Perthes-like deformities of class III. b A preoperative AP radiograph of the left hip in the abducted position showing the widening of the join space. c A postoperative AP radiograph of the left hip, taken 5 years postoperatively. The progression of osteoarthritis has not been recognised at the time of writing
We performed CPO through the anterior approach as described previously [9]. The skin incision for this osteotomy was relatively small, approximately 12 cm long. The lateral femoral cutaneous nerve was dissected free from the surrounding connective tissues. After we osteotomised the anterior superior iliac spine, it was retracted medially with the sartorius muscle attached. The iliac muscle was detached and a C-shaped osteotomy line from the anteroinferior iliac spine to the distal part of the quadrilateral surface was marked using an airtome. To preserve the blood supply to the acetabular fragment, we did not strip the gluteus muscles from the iliac bone. This also enabled acetabular reorientation because the osteotomy surfaces had the same curvatures. Osteotomy of the quadrilateral surface was first carried out using a curved osteotome, and the ischium, superior ramus of the pubis and ilium were osteotomised. We usually reoriented the acetabular fragment laterally and then fixed it with two or three screws. Immediately after fixation of the reoriented acetabular fragment, we confirmed the range of motion in the hip. Active motion exercises were begun on postoperative day and partial weight bearing on two crutches was allowed on the third postoperative day. The weight was increased by 10 kg every 2 weeks and full weight bearing was allowed after 8 weeks.
Clinical evaluations were performed preoperatively and at the latest follow-up using the Harris hip score [4]. The range of motion and leg length discrepancy was also measured preoperatively and at the latest follow-up. All clinical evaluations were performed by one of the authors (YN). Another author (TK) performed radiographic evaluations using CE angle, the acetabular head index (AHI) [5] and acetabular roof obliquity (ARO) [6] preoperatively and at the latest follow-up. The degree of the osteoarthritis was graded using the Tönnis classification system [7, 13] preoperatively and at the latest follow-up. A normal joint space was rated as Grade 0, slight narrowing of the joint space was rated as Grade 1, moderate (<50%) narrowing of the joint space was rated Grade 2 and severe (>50%) narrowing of the joint space was rated as Grade 3.
Statistics
The chi-square test was used to compare the changes preoperatively and at the latest follow-up in the clinical results and various radiographic parameters. Significance was defined as p < 0.05.
Results
According to the Stulberg classification system, there were no class I hips, three class II hips, 11 class III hips, three class IV hips and no class V hips preoperatively.
The average Harris hip score improved from 68.2 points (range 51–91 points) preoperatively to 91.1 points (range 61–98 points) at the latest follow-up, which was mainly due to decreased pain.
The average range of motion is shown in Table 1. Significant differences were not seen in the range of motion from flexion to extension between preoperative values and those at the latest follow-up (p > 0.05). Similarly, there were no significant differences in the range of motion from abduction to adduction and from external rotation to internal rotation between preoperative values and those obtained at the latest follow-up (p > 0.05).
Table 1 .
Range of motion before and after periacetabular osteotomy
| Preoperative value (average, range) | Value at the latest follow-up (average, range) | Significance | |
|---|---|---|---|
| Flexion | 119° (110–120) | 115° (70–120) | NS |
| Extension | 6.47° (0–10) | 5.30° (0–10) | NS |
| Abduction | 33.2° (30–40) | 30.6° (5–40) | NS |
| Adduction | 14.7° (10–20) | 13.5° (0–20) | NS |
| External rotation | 35.9° (30–40) | 34.7° (10–40) | NS |
| Internal rotation | 35.3° (30–40) | 32.4° (5–40) | NS |
NS=not significant
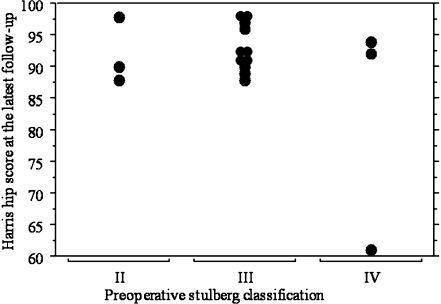
Only one patient with a class IV hip has been converted to total hip arthroplasty since CPO was performed 10 years ago (Fig. 2). The average Harris hip score of class IV hips was lower than that of class II or class III hips (Fig. 3). Leg length discrepancy had been recognised in ten hips preoperatively and this number did not change at the latest follow-up. The average leg length discrepancy in these ten hips was 1.1 cm (range 0–2.5 cm).
Fig. 2.

A 39 year-old woman had conservative treatments for dysplasia of the hip (DDH) during childhood. She had Perthes-like deformities of Stulberg class IV and osteoarthritis of Tönnis Grade 2 at the time of operation. A radiograph of the right hip, taken 10 years postoperatively, shows the progress of osteoarthritis
Fig. 3.
The relationship between preoperative Stulberg classification and the Harris hip score at the latest follow-up. The average Harris hip score at the latest follow-up of class II, class III and class IV hips was 92.0, 93.3 and 82.3, respectively. The average postoperative Harris hip score of class IV hips was smaller than that of class II or class III hips
Radiographically, the average lateral CE angle improved from a mean of −0.3° (range −22°–16°) preoperatively to a mean of 30.4° (range 15°–45°) at the latest follow-up, the ARO value improved from a mean of 29.6° (range 18°–42°) to a mean of 7.6° (range −10°–22°) and the AHI improved from a mean of 49.9% (range 39–80%) to a mean of 82.6% (range 70–100%). The lateral CE angle, ARO values and AHI at the latest follow-up showed significant improvements (p < 0.01, p < 0.01 and p < 0.01, respectively) compared with their preoperative values. Preoperative assessment of the secondary osteoarthritis by Tönnis classification revealed nine hips to be Grade 0, seven hips to be Grade 1, one hip to be Grade 2 and no hips to be Grade 3. At the latest follow-up, the distribution had changed to nine Grade 0, five Grade 1 and two Grade 2. The remaining hip, a class IV hip of Stulberg classification, had been converted to total hip arthroplasty, as described above.
Discussion
Surgical treatment for skeletally immature patients with Perthes-like deformities has previously been reported [1, 16]. However, to the best of our knowledge, only one study has evaluated the results of surgery for dysplastic hips with these deformities in skeletally mature patients. Nunley et al. [11] reported the clinical results of periacetabular osteotomy for the treatment of these deformities in 24 hips in 20 patients. Intertrochanteric osteotomy was simultaneously performed in 14 of the 24 hips. The average Harris hip score in their patients was generally equal to that in our patients preoperatively and at follow-up. However, they described that six of the 24 hips had additional surgical procedures or major complications. In our institution, we have performed CPO without any other combined osteotomy for the treatment of dysplastic hip with Perthes-like deformities to improve the coverage of the femoral head and the steep acetabulum. None of our patients had additional surgical procedures or a major complication.
Some authors [7, 14] have described good clinical and radiographic results after periacetabular osteotomy for dysplastic hips, including moderate or advanced osteoarthritis. Good clinical and radiographic results of CPO for early or advanced osteoarthritis have also been reported [2, 9, 10]. The improvement in joint congruency in the abducted hip position preoperatively was an important factor to gain good clinical results of periacetabular osteotomy [8]. However, the improvement in joint congruency in the abducted position in hips with Perthes-like deformities in this series was less optimal compared to that in hips without these deformities, because the proximal femora in all of the hips of all classes except class I already had several deformities. The clinical results were generally satisfactory. Nevertheless, such disadvantages existed preoperatively. Our results suggest that stresses to the articular cartilage of acetabulum and femoral head were reduced because of the improvement of the CE angle, ARO value and AHI. The progression of osteoarthritis was recognised in only one patient who had had a class IV hip preoperatively and she has converted to total hip arthroplasty 10 years postoperatively. However, we think that CPO was useful even in this patient because she could play for time.
We assumed that the range of motion of the hip might decrease after periacetabular osteotomy, since patients with Perthes-like deformities have a shortening of the femoral neck and relative overgrowth of the greater trochanter. However, there were no significant differences in the range of motion in all directions between preoperative values and those at the latest follow-up. We suggest that there was no significant impingement between the reoriented acetabulum and the greater trochanter because the greater trochanter locates posterolaterally from the femoral head.
Patients with Perthes-like deformities usually have a leg length discrepancy because the femoral neck is shortened. In our study, however, most patients did not complain of the existence of a leg length discrepancy preoperatively or at the latest follow-up. There are likely two reasons for this: first, the degree of leg length discrepancy was not remarkable and second, the chief preoperative complaint of these patients was hip pain, which had improved at the latest follow-up. We recommend a sole brace to correct the leg length discrepancy in patients with a leg length discrepancy of more than 2 cm.
There is a limitation of this study though; the number of patients is small. However, we believe that good clinical and radiographic results would be obtained with our procedure, even if the number of patients was bigger than that in the present study.
Our mid-term results suggest that periacetabular osteotomy without any combined other procedure, as a treatment for patients with Perthes-like deformities, is an effective surgical treatment. Long-term follow-up will be essential because the joint congruency of hips with Perthes-like deformities is less optimal than that in hips with spherical femoral heads.
References
- 1.Cohen J. Congenital dislocation of the hip. Case report of an unusual complication and unusual treatment. J Bone Joint Surg Am. 1971;53:1007–1011. [PubMed] [Google Scholar]
- 2.Ezoe M, Naito M, Asayama I. Muscle strength improves after abductor-sparing periacetabular osteotomy. Clin Orthop Relat Res. 2006;444:161–168. doi: 10.1097/01.blo.0000196475.40151.8b. [DOI] [PubMed] [Google Scholar]
- 3.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular ostetomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 4.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 5.Heyman CH, Herndon CH. Legg-Perthes disease; a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32:767–778. [PubMed] [Google Scholar]
- 6.Massie WK, Howorth MB. Congenital dislocation of the hip. Part I. Method of grading results. J Bone Joint Surg Am. 1950;32:519–532. [PubMed] [Google Scholar]
- 7.Mayo KA, Trumble SJ, Mast JW. Results of periacetabular osteotomy in patients with previous surgery for hip dysplasia. Clin Orthop Relat Res. 1999;363:73–80. doi: 10.1097/00003086-199906000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Murphy S, Deshmukh R. Periacetabular osteotomy: preoperative radiographic predictors of outcome. Clin Orthop Relat Res. 2002;405:168–174. doi: 10.1097/00003086-200212000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Naito M, Shiramizu K, Akiyoshi Y, Ezoe M, Nakamura Y. Curved periacetabular osteotomy for treatment of dysplastic hip. Clin Orthop Relat Res. 2005;433:129–135. doi: 10.1097/01.blo.0000153281.75265.1d. [DOI] [PubMed] [Google Scholar]
- 10.Nakamura Y, Naito M, Akiyoshi Y, Shitama T. Acetabular cysts heal after successful periacetabular osteotomy. Clin Orthop Relat Res. 2007;454:120–126. doi: 10.1097/01.blo.0000229370.88479.76. [DOI] [PubMed] [Google Scholar]
- 11.Nunley RM, Clohisy JC, Schoenecker PL (2007) Periacetabular osteotomy for the treatment of Perthes-like deformities of the hip. American Academy of Orthopaedic Surgeons (AAOS), pp 403 (abstract)
- 12.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108. [PubMed] [Google Scholar]
- 13.Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. New York: Springer-Verlag; 1987. pp. 165–171. [Google Scholar]
- 14.Trousdale RT, Ekkernkamp A, Ganzy R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995;77:73–85. doi: 10.2106/00004623-199501000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(Suppl 58):1–135. [Google Scholar]
- 16.Westin GW, Ilfeld FW, Provost J. Total avascular necrosis of the capital femoral epiphysis in congenital dislocated hips. Clin Orthop Relat Res. 1976;119:93–98. [PubMed] [Google Scholar]