Abstract
The treatment of intra-articular proximal tibial fractures is associated with complications, and much conflicting literature exists concerning the treatment of choice. In our study, an attempt has been made to develop an ideal and adequate treatment protocol for these intra-articular fractures. The principle of double osteosynthesis, i.e., lateral minimally invasive plate osteosynthesis (MIPO), was combined with a medial external fixator to treat 22 intra-articular proximal tibial fractures with soft tissue injury with a mean follow-up of 25 months. Superficial pin track infection was observed in one case, and no soft tissue breakdown was noted. Loss of articular reconstruction was reported in one case. Bridging callus was seen at 12 weeks (8 weeks–7 months). The principle of substitution or double osteosynthesis, i.e., lateral MIPO, was combined with a medial external fixator and proved to be a fairly good method of fixation in terms of results and complications.
Résumé
le traitement des fractures articulaires du tibia proximal est associé à un certain nombre de complications. Les traitements sont multiples. Dans notre étude, nous avons souhaité nous diriger vers un protocole adapté à ces fractures intra articulaires. le principe d’une double ostéosynthèse, c’est-à-dire, ostéosynthèse latérale par voie mini invasive, à l’aide d’une plaque (MIPO) a été combinée avec un fixateur externe par voie interne. 22 patients présentant une telle lésion ont été traités de cette façon avec un suivi moyen de 25 mois. des infections de broches superficielles ont été observées dans un cas sans lésion notable des tissus mous. Un déplacement secondaire articulaire a également été rapporté dans un cas. L’apparition d’un pont osseux se fait généralement à 12 semaines en moyenne (huit semaines à sept mois). le principe d’un tel traitement avec double ostéosynthèse est une bonne méthode pour traiter ces lésions et pour éviter un certain nombre de complications.
Introduction
Among the challenges that commonly faced by the surgeon while dealing with intra-articular proximal tibial fractures, the two most common are; the compromised skin and soft tissue envelope, which invites a high rate of complications following attempted open reduction and internal fixation, and poor bone quality and comminuted fracture patterns creating difficulty in achieving stable fixation [1–4, 9, 14, 15, 17, 19].
Non-operative treatment using traction, casts or braces has been reported to produce excellent results. But these methods are complicated by the loss of reduction, poor functional results and prolonged hospital stays [5, 6].
Arthroscopically assisted fixation and minimal percutaneous pinning have also been reported to give good results but these modalities are suitable for simple split depression and local compression fractures [8, 18].
Open double plate fixation is associated with the dreaded complication of wound dehiscence and infection. Hybrid fixation systems or Illizarov’s fixation systems give functional results, but at increased risk of septic arthritis and pin tract infection and prolonged courses of treatment affecting patient compliance.
Mast applied the technique of double osteosynthesis or combined external and internal fixation for the first time in 1980 in the treatment of complex intraarticular supracondylar humeral fractures. Instead of posterior lateral and medial plates he used a medial plate and a lateral minifixator to neutralise the bending moments on the plate [11].
Open lateral plating and medial fixator in complex bicondylar fractures of the tibia give good functional results minimising soft tissue complications. We have further optimised the biological fixation by doing a lateral MIPO (minimally invasive plate osteosynthesis) and medial external fixator.
Materials and methods
Between 2004 and 2006, 22 patients (16 males and 6 females) with complex upper and tibia fractures were treated with double osteosynthesis. The mean age of the patients was 45 years. The mechanism of injury was road traffic accidents (14 patients) and falls from varying heights (8 patients). Four patients suffered from additional limb fractures, head, chest or abdominal injury. All fractures were classified as complex Schatzker type V or VI. All fractures were closed, but with varying degrees of soft tissue injury, which were graded by the Tscherne and Godzen scale [21]. All fractures were treated by one stage surgery. Eight patients who reported within 48 h of injury were managed immediately, and the rest were managed at 7–10 days as they reported late. Plate osteosynthesis was performed through lateral minimally invasive double incision. Medial unilateral frame with three Schantz pins, one in the proximal fragment and two in the distal fragment to span the whole tibia, were used (Fig. 1). In two patients autologous bone graft was needed at the time of surgery due to bone loss. After surgery, the leg was elevated with a posterior above-knee splint until soft tissue swelling resolved. Knee motion was started on the 3rd day with a CPM machine. Range of motion of an average 100 degrees was obtained by 10 days and the patients were discharged with removal of stitches and removal of the posterior splint. Strict instructions were given regarding pin track care. All patients were seen in an out-patient department every 10 days until the fixator was removed. They were maintained on non-weight-bearing ambulation for 3 months. After a mean time of 8 weeks (range 6–10 weeks) the external fixator was removed in all patients with radiological evidence of progressive fracture consolidation. X-Ray were taken at 1.5 months at the time of removal of the fixator, then every 3 months up to 1 year and at final follow-up.
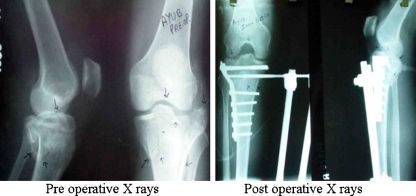
Fig. 1.
Preoperative and postoperative X-rays. Anteroposterior and lateral views of Schatzker type V tibial plateau fracture
Results
In all 22 patients the fracture healed uneventfully. No wound dehiscence or infection was noted. None of the patients developed joint infection. One patient had pin-tract infection, which was suppressed with daily care and antibiotics. In one patient, loss of articular reconstruction occurred, but the functional painless range of motion of the patient was 150° of flexion. None of the patients developed a varus deformity.
At the final physical examination, the mean range of motion in all operated knees was flexion 132° (range 115°–150°) and extension −3° (range −8° to + 4°) (Fig. 2).
Fig. 2.
Clinical follow-up photographs of a patient showing full extension and flexion
Discussion
Anatomical joint reconstruction, axial alignment and the relative stability of the proximal tibia allowing the earliest joint mobilisation, while keeping complications to a minimum, are the major goals in the treatment of complex proximal tibial fractures. Traction is associated with long hospital stays and morbidity related to immobilisation. Cast or cast bracing does not provide enough stability and leads to a loss of reduction and malunion respectively with loss of functional outcome due to prolonged immobilisation [5, 6].
In order to stabilise bicondylar and complex proximal tibial fractures, both medial and lateral columns should be reduced and fixed. Although dual plating successfully addresses the mechanical part of the problem by buttressing both columns, the high rate of complications associated with this open technique is a real concern, with a reported rate of deep infection of 20–80%. Moore et al. reported wound dehiscence and/or infection in 8 of 11 bicondylar fractures treated with double plate fixation [12]. These fractures usually have associated injuries to the distal femur with extensive soft tissue injury [7]. The soft tissue problems are more on the anteromedial aspect. Especially with the extensive soft tissue injury produced by double plating, the incidence of infection and dehiscence are very high. In our study superficial pin track infection was observed in one case and no soft tissue breakdown was noted. Loss of articular reconstruction was reported in one case.
In this context the use of an external fixator to optimise the fixation without severely aggravating the already jeopardised soft tissue envelope is a welcome concept. Marsh et al. presented 21 complex tibial plateau fractures treated by closed reduction, interfragmentory screw fixation and application of half pin fixator with good results [10]. Pin track infection occurred in seven cases and septic arthritis in two cases mainly due to the long time that the external fixator was left in place. Barbary et al. in their study of 30 tibial plateau fractures (Schatzker type VI) treated with Ilizarov fixator concluded that the use of external fixation and minimal internal fixation resulted in clinical success and low morbidity [7]. Mechanical properties of the fixator do not allow aggressive mobilisation [20, 23]. Pin track infection and pin loosening are known to be very frequent problems with external fixation, but these can be reduced by decreasing the period that the external fixator is left in situ and with meticulous pin track care. Septic arthritis can be avoided by placing the pin 2 cm away from the joint line.
The use of the Sheffield Hybrid Fixator (SHF), an all ring fine wire system, has been used in some centres successfully in the management of complex fractures, particularly in intra-articular injuries with good clinical outcome. But the literature still lacks the biomechanical evidence to support the use of this method for the treatment of bicondylar tibial plateau fractures [22].
At the proximal end of tibia one can theoretically use two fixator systems (composite fixator), one medial and other lateral, for neutralisation of adverse forces that develop during functional rehabilitation of complex fractures. This type of mechanical optimisation can be provided by circular ring type systems such as Illizarov’s or hybrid systems, but the lateral pins pass through a rather mobile soft tissue layer compared with the medial side, with an increased risk of pin tract infection and arthritis [13]. On the other hand the advantage of an external fixator is that it helps in reducing the number of screws and size of the plate if both systems of fixation are used simultaneously. The mechanical properties of tension, compression and correction of axial deviation varus or valgus in the postoperative period are also possible.
The technique of double osteosynthesis or substitution combines the principles of stability, restoration of anatomy and early motion, while eliminating the need for excessive soft tissue dissection. The relatively short time period of external fixation ensures that the wound dehiscence, infection and pin track complications are negligible. This method is a further improvement on the open, more extensive lateral approach with a medial fixator [10, 16]. The rates of malunion are low because of the optimal strength provided by two fixator systems.
References
- 1.Apley A. Fractures of the tibial plateau. Orthop Clin North Am. 1979;10:61–74. [PubMed] [Google Scholar]
- 2.Bach AW, Hansen ST. Plates versus external fixation in severe open tibial shaft fractures. Clin Orthop. 1989;241:89–94. [PubMed] [Google Scholar]
- 3.Blokker CP, Rorabeck CH, Bourne RB. Tibial plateau fractures and analysis of treatment in 60 patients. Clin Orthop. 1984;182:193–198. [PubMed] [Google Scholar]
- 4.Christensen K, Powell J, Bucholz R. Early results of a new technique for treatment of high grade tibial plateau fractures. J Orthop Trauma. 1990;4:226. doi: 10.1097/00005131-199004020-00059. [DOI] [Google Scholar]
- 5.DeCoster TA, Nepola JV, El-Khoury GY. Cast brace treatment of proximal tibia fractures. A 10-year follow-up study. Clin Orthop. 1998;231:196–204. [PubMed] [Google Scholar]
- 6.Delamarter R, Hohl M. The cast brace and tibial plateau fractures. Clin Orthop. 1989;242:26–31. [PubMed] [Google Scholar]
- 7.Barbary H, Abdel Ghani H, Misbah H, Salem K. Complex tibial plateau fractures treated with Ilizarov external fixator with or without minimal internal fixation. Int Orthop. 2005;29(3):182–185. doi: 10.1007/s00264-005-0638-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gaunche CA, Markman AW. Arthroscopic Management of Tibial Plateau Fractures. Arthroscopy. 1993;9:467. doi: 10.1016/S0749-8063(05)80324-X. [DOI] [PubMed] [Google Scholar]
- 9.Jensen DB, Rude C, Duus B, Bjerg-Nielsen A. Tibial plateau fractures. A comparison of conservative and surgical treatment. J Bone Joint Surg (Br) 1990;72:49–52. doi: 10.1302/0301-620X.72B1.2298794. [DOI] [PubMed] [Google Scholar]
- 10.Marsh JL, Smith ST, Do TT. External fixation and limited internal fixation for complex fractures of the tibial plateau. J Bone Joint Surg. 1995;77A:661. doi: 10.2106/00004623-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Mast J, Jakob R, Ganz R. Planning and reduction technique in fracture surgery. New York: Springer; 1989. [Google Scholar]
- 12.Moore T, Patzakis M, Harvey J. Tibial plateau fractures, definition, demographics, treatment rationale and long-term results of closed traction management or operative reduction. J Orthop Trauma. 1987;1(2):97–119. doi: 10.1097/00005131-198702010-00001. [DOI] [PubMed] [Google Scholar]
- 13.Morandi MM, Landi S, Kilaghbian V, Randelli P. Shatzker Type VI Tibial Plateau Fractures Treated with the Ilizarov External Fixator. Bull Hosp Jt Dis. 1997;56:46. [PubMed] [Google Scholar]
- 14.Perry CR, Evans G. New surgical approach to fractures of the lateral tibial plateau. J Bone Joint Surg [Am] 1984;66:1236–1240. [PubMed] [Google Scholar]
- 15.Ras’mussen P. Tibial condylar fractures, impairment of knee joint stability as an indicator for surgical treatment. J Bone Joint Surg [Am] 1973;55:1331–1350. [PubMed] [Google Scholar]
- 16.Ries MD, Meinhard BP. Medial external fixation with lateral plate internal fixation in metaphyseal tibial fractures. A report of 8 cases associated with severe soft tissue injuries. Clin Orthop. 1990;256:215–223. [PubMed] [Google Scholar]
- 17.Schatzker J. Tibial plateau fractures. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal trauma. Philadelphia: WB Saunders; 1992. pp. 2143–2186. [Google Scholar]
- 18.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture: the Toronto experience 1968–1975. Clin Orthop. 1979;138:94. [PubMed] [Google Scholar]
- 19.Szyszkowitz R. Patella and tibia. In: Müller ME, Allgöwer M, Schneider R, Willenegger H, editors. Manual of internal fixation. 3. Berlin: Springer; 1995. p. 554. [Google Scholar]
- 20.Toulatios AS, Xenakis T, Soucacos PK, Soucacos PN. Surgical management of tibial plateau fractures. Acta Orthop Scand. 1997;75:92. doi: 10.1080/17453674.1997.11744755. [DOI] [PubMed] [Google Scholar]
- 21.Tscherne H, Rojczyk M. The treatment of closed fractures with soft tissue injuries. In: Tscherne H, Gotzen L, editors. Fractures with soft tissue injuries. Berlin, Germany: Springer; 1984. pp. 39–45. [Google Scholar]
- 22.Weiner LS, Kelley M, Yang E, et al. The use of combination internal fixation and hybrid external fixation in severe proximal tibial fractures. J Orthop Trauma. 1995;9:244. doi: 10.1097/00005131-199506000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Orthop Rev. 1994;2:149. [PubMed] [Google Scholar]