Abstract
The purpose of this study is to evaluate the efficacy of the computed tomography (CT)-guided percutaneous radiofrequency thermoablation (PRT) method with a minimum of 2 years follow-up. Twenty-eight patients who were followed for more than 2 years among 35 patients who underwent CT-guided PRT between April 1999 and May 2005 were included in this study. The mean age was 24.5 years (range 7–55 years) and the mean follow-up period was 40.1 months (range 24–66 months). With a radiofrequency electrode, the lesion was heated to 80°C or 90°C for 6.5 mins (range 3–9 mins). Clinical success was assessed at the out-patient clinic by symptoms and radiographs. Twenty-six patients (90%) experienced a total loss of symptoms and additional PRT also relieved the ongoing symptoms in all of the recurrent patients. PRT appears to be a safe and effective method for treating osteoid osteoma and is also effective in recurrent cases. This treatment modality is a minimally invasive procedure and is a good alternative to open surgical treatment.
Résumé
Le propos de cette étude est d’évaluer l’efficacité de cette méthode avec un minimum de deux ans de recul. 28 patients ont été suivis pendant deux ans parmi 35 patients ayant bénéficié entre avril 99 et mai 2005 d’une ablation d’ostéome ostéoide par radio fréquence, guidée sous scanner. L’âge moyen était de 24,5 ans (7 à 55) et le suivi moyen de 40,1 mois (24 à 66). L’électrode permet de chauffer la lésion de 80 à 90°C en moyenne pendant 6,5 minutes (de 3 à 9). 90% des patients (26 à 28) ont pu, grâce à cette méthode, avoir une disparition totale des symptômes et pour ceux qui gardaient une symptomatologie persistante ou récurrente, un geste complémentaire de thermo régulation a été réalisé. Cette méthode apparaît comme une méthode sûre et efficace dans le traitement des ostéomes ostéoides et également dans les récidives. Ce traitement est un traitement mini invasif tout a fait alternatif avec le traitement par voie chirurgicale sanglante.
Introduction
Osteoid osteoma is a benign bone tumour and occurs mainly in children and young adults. They account for approximately 10% of benign bone tumours and most commonly occur in the femur and the tibia [1, 2, 5, 10]. Traditionally, treatment has been either medical methods in the form of long-term administration of non-steroidal anti-inflammatory drugs (NSAIDs) or aspirin, or surgical methods in the form of open curettage or en bloc resection.
The unremitting nature of the pain usually leads to a surgical referral. Complete surgical excision is the classic treatment but this method may result in the resection of substantial amounts of normal bone in an effort to completely excise these small tumours. Moreover, lesions located in anatomical areas that are technically difficult to access can carry substantial postoperative morbidity for these patients [2]. In recent years, the use of the computed tomography (CT)-guided percutaneous radiofrequency thermoablation (PRT) has been reported with good results and this has been shown to have similar recurrence rates to open surgery but with fewer complications and shorter periods of hospital stay [2, 5–7, 10, 14–17]. However, the long-term follow-up of this method is rare and continuous long-term follow-up is required to determine the definite effectiveness of this technique compared to traditional open resection.
The purposes of this study are to: (1) evaluate the effectiveness of PRT for the osteoid osteoma with the clinical results of a minimum of 2 years follow-up and (2) confirm the effectiveness of repeat therapy in the recurrent patients that have already had PLT, although this is a small group.
Materials and methods
Demographics
This retrospective study enrolled 28 patients who were suitable to follow-up for more than 2 years among 35 patients who underwent PRT between April 1999 and May 2005 in our hospital. There were 21 men and 7 women. The mean age was 24.5 years (range 7–55 years) and the mean follow-up period was 40.1 months (range 24–66 months).
Pre-PRT analysis and management of osteoid osteoma
All patients had typical histories and we confirmed the presence of a nidus using plain radiographs in all patients. We performed additional CT or magnetic resonance imaging (MRI) in order to obtain detailed information in 25 patients. Initial medical treatment was performed in all cases, except for two patients who had persistent symptoms after they had undergone open surgical resection or thermoablation in other hospitals. The mean duration of symptoms before PRT was 26.4 months (range 1–180 months).
Technique
The procedures were performed on an in-patient basis and were carried out by an interventional radiologist and orthopaedic surgeon in the CT room. After general or spinal anaesthesia, the patient was positioned on the CT bed and the lesion was confirmed by CT imaging (Fig. 1). The entry point on the skin was marked and aseptic preparation was done. A small skin incision was made at the entry point and blunt dissection was done with haemostat or mosquito to prevent neurovascular injuries. A trochar and cannula was advanced to the bone and the trochar was tapped gently with a mallet until it advanced into the nidus after re-confirming the position of the nidus by CT imaging. The trochar was removed and a straight electrode was placed through the sleeve and thermal ablation was done at 85–90°C for 6.5 mins (range 4–9 mins) (Fig. 2). After the procedure, a compressive sterile dressing was applied. We did not restrict the activity of the patient immediately after the procedure.
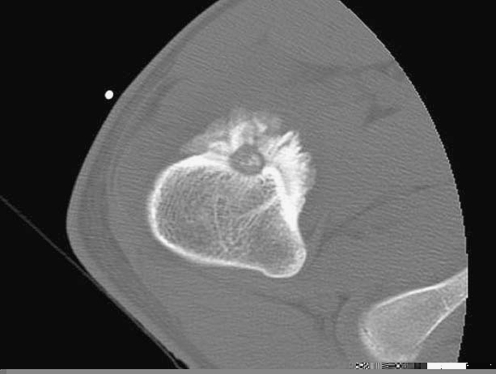
Fig. 1.
Computed tomography (CT) image shows the lesion of osteoid osteoma in the proximal femur
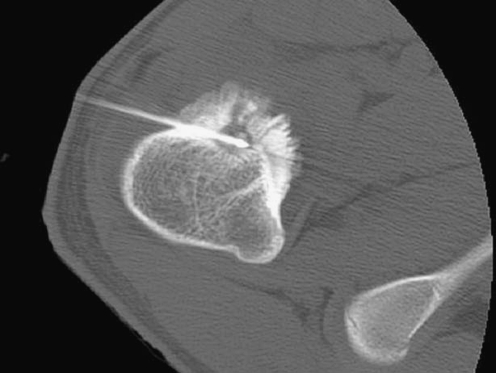
Fig. 2.
The electrode is inserted within the lesion under CT guidance
Evaluation methods
To access short-term outcomes and detect procedure-related problems, the patients were thoroughly examined during the admission period. We evaluated the symptoms on admission, the time that symptoms subside and any complications. To determine the long-term outcome, we divided the patients into three subgroups, denoted as good if the patient did not have any symptoms, fair if the patient had some pain though the symptoms were much improved and poor if the pain was aggravated or the lesion recurred. If the lesion recurred, we checked the MRI and we repeated the PRT using the same method. The chi-squared test was used to compare recurrence with size and location.
Results
Location, size and biopsy
We performed biopsy during PRT procedures in 27 patients and gained definative diagnosis in 11 (40.7%) patients. Inadequate specimens were obtained in 16 patients. There were 18 lesions in the femur, six lesions in the tibia, two in the pelvic bone and one each in the humerus and the fibula. Recurrence occurred in three patients (two femurs, one ilium). There was no significant correlation between lesion location and local recurrence (P > 0.05).
Lesion size was calculated from the CT scan from the axial, sagittal and coronal cuts. The size was measured from 2 × 2 × 1 mm to 14×13×8 mm and there was no significant correlation between lesion size and local recurrence (P > 0.05).
Short-term outcome and complications
The procedure was technically successful in all cases (technical success rate 100%, 28/28 procedures). Minor burn injury occurred in one patient and we performed debridement twice. In this patient, he was satisfied with the procedure because his local pain subsided. After PRT, seven patients reported immediate pain relief, 15 patients within the first day, five patients during the second day and one patient on the seventh day. The mean admission period from PRT to discharge was 1.8 days (range 1–5 days) except for one patient with complications who needed debridement. All patients were free of pain at discharge from the hospital.
Long-term outcome
At the last follow-up, 26 (92.9%) of the patients were classified as good and two (7.1%) as fair. Thus, 100% of the patients had a good or fair rating at the last evaluation. During the follow-up period, three patients showed recurrence and we performed repeat thermoablation good results at the last follow-up without recurrence. We did not performed additional procedures for the fair group.
Re-trial of recurred patients
In this study, there were five recurrent patients. Two of them had had either open resection or PRT at other hospitals. We performed PRT on them and gained good results at the last follow-up. The remaining three patients had PRT in our hospital but they showed good results at the last follow-up after repeat PRT (Table 1).
Table 1.
Second percutaneous radiofrequency thermoablation (PRT) of the recurred five patients
| Case | Sex | Age | Site and size(mm) | PP* | RFP† (month) | FFS‡ (month) | Results |
|---|---|---|---|---|---|---|---|
| 1 | F | 18 | Femur (7×6×4) | Open excision | 1 | 57 | Good |
| 2 | M | 21 | Femur (4×4×2) | Thermoablation | 4 | 43 | Good |
| 3 | M | 26 | Femur (4×5×4) | Thermoablation | 16 | 54 | Good |
| 4 | M | 31 | Ilium (14×13×3) | Thermoablation | 2 | 66 | Good |
| 5 | M | 17 | Femur (6×8×4) | Thermoablation | 8 | 24 | Good |
*Primary procedure
†Recurrence period from primary procedure
‡Follow-up from second procedure
Discussion
The diagnosis of osteoid osteoma mainly relies on history and radiological information. Because a biopsy of the lesion was not always taken at the time of operative treatment, an argument could be made that a portion of patients in this study may not have had the condition in question [2, 14, 17]. Histological confirmation with minimal-access techniques is only available in approximately 36–75% of cases [4]. Peyser et al. [12] obtained a definite diagnosis in 15 (46.9%) among our 32 patients we also obtained a definite diagnosis in only 11 (40.7%) patients during PRT.
Many patients with osteoid osteoma are able to tolerate their pain with or without the use of analgesics. If symptoms persist, initial treatment usually consists of a trial of medical therapy using aspirin or other NSAIDs. With regards to medical treatment, long-term medication is needed and symptoms may recur after the discontinuation of medication [2, 9]. With increasing pain and associated insomnia, many seek definitive treatment traditionally achieved by surgical resection [4]. Traditional surgical treatments have ranged from local resection with a burr and curettage to wide resection with bone grafting and metallic fixation. Surgical therapy is successful in 88–100% of cases in the published series [4]. However, surgery requires longer in-patient treatment with longer anaesthesia times, more extensive tissue exposure, tissue damage, scarring, morbidity and recovery time [2, 4]. Surgery still has a role for those appendicular lesions where the neurovascular bundle is within 1–1.5 cm of the nidus, where the histology of the lesion is in doubt or for the persistence of symptoms after two ablative procedures [4].
Primary PRT has, in series totalling over 200 patients, had a success rate of 76–100%. In our series, we gained a success rate of 92.9% (26/28), an average of 1.8 days of hospital stay and one minor complication. These results are comparable with other good results. Rosenthal et al. [15] compared the results of open versus percutaneous treatment of osteoid osteoma; 68 were treated with open techniques and 33 were treated with percutaneous radiofrequency ablation. Those patients treated with radiofrequency ablation were followed up for an average of 3.4 years and had a 12% incidence of recurrence. The investigators stated that there was no statistical difference in the recurrence rates between the two methods. Their study also showed an average hospital stay of 4.7 days for the patients who had open treatment versus 0.18 days for patients who had radiofrequency ablation. Other authors have reported similar good results and short hospital stays for those patients treated with PRT [1, 3, 5, 8, 11].
With regard to the recurrent cases, it is generally said that recurrence after surgical therapy can occur up to 13 years after surgery [4]. The latest recurrence following PRT was at 44 months, although follow-up in these patients is considerably shorter than surgical series, most recurrences occur in the first 7 months after primary treatment [4]. We experienced recurrence in three patients and the period to recurrence from PRT were 2, 8 and 16 months, respectively. Recurrence response to a second PRT treatment is 50–100% in the 15 patients identified [4, 10, 13, 14]. We followed up the second PRT of the five recurrent patients for 24, 43, 54, 57 and 66 months, respectively, and obtained good results in all five patients.
A limitation of this study is the small number of recurrent patients followed-up to evaluate the effectiveness of a second PRT and longer follow-up is needed to accurately evaluate the effectiveness of primary PRT.
With our minimum 2 years follow-up, we concluded that PRT is a good treatment method that has many advantages for the treatment of osteoid osteoma which do not respond to medical treatment. We think that a second PRT is also as effective for the treatment of recurrent cases with similar results to primary cases, though the number is small in our study.
References
- 1.Akhlaghpoor S, Tomasian A, Arjmand Shabestari A, Ebrahimi M, Alinaghizadeh MR. Percutaneous osteoid osteoma treatment with combination of radiofrequency and alcohol ablation. Clin Radiol. 2007;62:268–273. doi: 10.1016/j.crad.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 2.Barei DP, Moreau G, Scarborough MT, Neel MD. Percutaneous radiofrequency ablation of osteoid osteoma. Clin Orthop Relat Res. 2000;373:115–124. doi: 10.1097/00003086-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Cantwell CP, O’Byrne J, Eustace S. Radiofrequency ablation of osteoid osteoma with cooled probes and impedance-control energy delivery. AJR Am J Roentgenol. 2006;186:S244–S248. doi: 10.2214/AJR.04.0938. [DOI] [PubMed] [Google Scholar]
- 4.Cantwell CP, O’Byrne J, Eustace S. Current trends in treatment of osteoid osteoma with an emphasis on radiofrequency ablation. Eur Radiol. 2004;14:607–617. doi: 10.1007/s00330-003-2171-6. [DOI] [PubMed] [Google Scholar]
- 5.Cribb GL, Goude WH, Cool P, Tins B, Cassar-Pullicino VN, Mangham DC. Percutaneous radiofrequency thermocoagulation of osteoid osteomas: factors affecting therapeutic outcome. Skeletal Radiol. 2005;34:702–706. doi: 10.1007/s00256-005-0947-2. [DOI] [PubMed] [Google Scholar]
- 6.Gangi A, Basile A, Buy X, Alizadeh H, Sauer B, Bierry G. Radiofrequency and laser ablation of spinal lesions. Semin Ultrasound CT MR. 2005;26:89–97. doi: 10.1053/j.sult.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Ghanem I, Collet LM, Kharrat K, Samaha E, Deramon H, Mertl P, Dagher F. Percutaneous radiofrequency coagulation of osteoid osteoma in children and adolescents. J Pediatr Orthop B. 2003;12:244–252. doi: 10.1097/00009957-200307000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Kjar RA, Powell GJ, Schilcht SM, Smith PJ, Slavin J, Choong PF. Percutaneous radiofrequency ablation for osteoid osteoma: experience with a new treatment. Med J Aust. 2006;184:563–565. doi: 10.5694/j.1326-5377.2006.tb00381.x. [DOI] [PubMed] [Google Scholar]
- 9.Kneisl JS, Simon MA. Medical management compared with operative treatment for osteoid-osteoma. J Bone Joint Surg Am. 1992;74:179–185. [PubMed] [Google Scholar]
- 10.Lindner NJ, Ozaki T, Roedl R, Gosheger G, Winkelmann W, Wörtler K. Percutaneous radiofrequency ablation in osteoid osteoma. J Bone Joint Surg Br. 2001;83:391–396. doi: 10.1302/0301-620X.83B3.11679. [DOI] [PubMed] [Google Scholar]
- 11.Mahnken AH, Tacke JA, Wildberger JE, Günther RW. Radiofrequency ablation of osteoid osteoma: initial results with a bipolar ablation device. J Vasc Interv Radiol. 2006;17:1465–1470. doi: 10.1097/01.RVI.0000235737.22496.6A. [DOI] [PubMed] [Google Scholar]
- 12.Peyser A, Applbaum Y, Khoury A, Liebergall M, Atesok K. Osteoid osteoma: CT-guided radiofrequency ablation using a water-cooled probe. Ann Surg Oncol. 2007;14:591–596. doi: 10.1245/s10434-006-9293-4. [DOI] [PubMed] [Google Scholar]
- 13.Rosenthal DI. Percutaneious radiofrequency treatment of osteoid osteomas. Semin Musculoskelet Radiol. 1997;1:265–272. doi: 10.1055/s-2008-1080147. [DOI] [PubMed] [Google Scholar]
- 14.Rosenthal DI, Hornicek FJ, Torriani M, Gebhardt MC, Mankin HJ. Osteoid osteoma: percutaneous treatment with radiofrequency energy. Radiology. 2003;229:171–175. doi: 10.1148/radiol.2291021053. [DOI] [PubMed] [Google Scholar]
- 15.Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, Mankin HJ. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am. 1998;80:815–821. doi: 10.2106/00004623-199806000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Venbrux AC, Montague BJ, Murphy KP, Bobonis LA, Washington SB, Soltes AP, Frassica FJ. Image-guided percutaneous radiofrequency ablation for osteoid osteomas. J Vasc Interv Radiol. 2003;14:375–380. doi: 10.1097/01.rvi.0000058420.01661.8c. [DOI] [PubMed] [Google Scholar]
- 17.Woertler K, Vestring T, Boettner F, Winkelmann W, Heindel W, Lindner N. Osteoid osteoma: CT-guided percutaneous radiofrequency ablation and follow-up in 47 patients. J Vasc Interv Radiol. 2001;12:717–722. doi: 10.1016/S1051-0443(07)61443-2. [DOI] [PubMed] [Google Scholar]